Abstract
Noradrenergic and dopaminergic mechanisms have been proposed for the pathophysiology of seasonal affective disorder (SAD). We investigated the effects of catecholamine depletion using α-methyl-para-tyrosine (AMPT), an inhibitor of tyrosine hydroxylase, in patients with SAD in natural summer remission. Nine drug-free patients with SAD by DSM-IV criteria, in summer remission for at least eight weeks, completed a double-blind, crossover study. Behavioral ratings and serum HVA and MHPG levels were obtained for 3-day sessions during which patients took AMPT or an active control drug, diphenhydramine.The active AMPT session significantly reduced serum levels of HVA and MHPG compared with the control diphenhydramine session. The AMPT session resulted in higher depression ratings with all nine patients having significant clinical relapse, compared with two patients during the diphenhydramine session. All patients returned to baseline scores after drug discontinuation. Catecholamine depletion results in significant clinical relapse in patients with SAD in the untreated, summer-remitted state. AMPT-induced depressive relapse may be a trait marker for SAD, and/or brain catecholamines may play a direct role in the pathogenesis of SAD.
Similar content being viewed by others
Main
Seasonal affective disorder (SAD) is classified as a subtype of major depression characterized by recurrent seasonal depressive episodes (Rosenthal et al. 1984). These episodes usually have a fall/winter onset and pattern, with full remission of symptoms (or a switch into hypomania/mania) during spring/summer. Exposure to bright artificial light, termed light therapy or phototherapy, is an effective treatment that is currently recommended in clinical guidelines for SAD (Lam and Levitt 1999).
Monoamine neurotransmitter hypotheses have been proposed for the pathophysiology of SAD and the mechanism of action of light therapy. Many studies have focused on disturbances of serotonin (5-HT), but other studies have found evidence for catecholamine (dopamine, DA, and norepinephrine, NE) dysfunction in SAD (for review see Lam and Levitan 2000).
Reduced dopaminergic function in SAD is supported by findings of abnormalities of basal serum prolactin levels in winter and summer (Depue et al. 1989, 1990) and reduced heat-loss response to thermal challenge in winter (Arbisi et al. 1989, 1994). Reduced eye blink rates indicative of lower dopaminergic tone were found in some studies (Depue et al. 1988) but not in others (Barbato et al. 1993). Negative findings include normal levels of catecholamine metabolites in the cerebrospinal fluid (CSF) of SAD patients before and after light therapy (Rudorfer et al. 1993). Also, a placebo-controlled treatment study found no significant overall effects of l-dopa for SAD (Oren et al. 1994).
Evidence for noradrenergic dysfunction in SAD includes blunted NE responses to orthostatic challenge (Rosenthal et al. 1987) and to the serotonin and α2-adrenergic agonist m-CPP (Schwartz et al. 1997). SAD patients tend to have lower baseline NE levels compared with controls (Schwartz et al. 1997) with increased NE levels after light therapy (Anderson et al. 1992). Bupropion, an antidepressant that acts on noradrenergic/dopaminergic systems, has some benefit for SAD patients (Dilsaver et al. 1992).
Catecholamine levels can be experimentally manipulated using α-methyl-para-tyrosine (AMPT). AMPT reduces synthesis of NE and DA by reversibly inhibiting the rate-limiting enzyme, tyrosine hydroxylase, thereby blocking conversion of tyrosine to l-dopa. A dose of 3 g/day of AMPT can reliably reduce urinary MHPG (a NE metabolite) by 70%, and CSF levels of HVA (a DA metabolite) by 60% with no change in CSF 5-HIAA (a 5-HT metabolite) (Bunney et al. 1971). Maximum catecholamine reduction occurs two to three days after starting AMPT, and levels return to baseline within two to three days of stopping the drug. The behavioral effects and side effects of AMPT are minimal in medically ill, non-psychiatric patients during chronic AMPT treatment (Engelman et al. 1968). Early studies involving small numbers of subjects suggested that AMPT depletion led to increase in depressive symptoms in depressed patients (Bunney et al. 1971), but more recent placebo-controlled studies have not shown mood effects in depressed patients (Miller et al. 1996). A recent study found that, in patients with SAD who were in early remission with light therapy during winter, both AMPT depletion and tryptophan depletion resulted in depressive relapses (Neumeister et al. 1998b). These results suggest that the antidepressant response of light therapy is mediated at least partially through the catecholaminergic system.
Given that summer remission of symptoms is a criterion for the clinical definition of SAD, it is of interest to determine the effects of catecholamine depletion in SAD patients in summer. We hypothesized that, if catecholamine dysfunction was critical in the pathophysiology of SAD, reducing catecholamines using AMPT would transiently induce depressive symptoms in SAD patients in natural summer remission.
METHODS
This study was approved by the human ethics committee of the University of British Columbia. After giving written informed consent, patients were administered the Structured Clinical Interview for DSM-IV (SCID) (Williams et al. 1992) and met DSM-IV criteria for recurrent unipolar major depressive disorder with a seasonal, winter pattern. Severity of symptoms was evaluated using the Structured Interview Guide for the Hamilton Depression Rating Scale, Seasonal Affective Disorders Version (SIGH-SAD) (Williams et al. 1988). Entry criteria included a period of remission, defined as a score of 10 or less on the 29-item SIGH-SAD, of at least eight weeks without treatment. Exclusion criteria included significant medical conditions or psychotropic medication use within eight weeks. Females were studied during the early follicular phase of their menstrual cycle to control for menstrual variation in catecholamine metabolism. All subjects were medically healthy as determined by a physical examination, blood tests, an electrocardiogram, urinalysis, and a pregnancy test.
The subjects then underwent a randomized, double-blind protocol with two test sessions separated by at least five days. Each test session consisted of two days of drug treatment and a follow-up day. For the catecholamine depletion session, patients took AMPT 1 gram orally t.i.d for the first day followed by 1 g b.i.d. for the second day. Because AMPT has significant sedative side effects, an active control drug was used to preserve the blind: diphenhydramine, a sedating antihistamine with no known mood effects during short-term use, was given at 50 mg t.i.d. for the first day followed by 50 mg b.i.d for the second day. The last dose of medication was given at noon on Day 2. Patients returned at 9 A.M. on Day 3 for an assessment.
Behavioral ratings were obtained by raters blind to session condition on Day 1 (at 9 A.M. prior to starting drug, and at 4 P.M.), Day 2 (9 A.M. and 4 P.M.), and Day 3 (9 A.M.). Ratings included the HAM-20, consisting of the 29-item SIGH-SAD modified to exclude the nine items that could not be rated within the same day. The Profile of Mood States (POMS) (McNair et al. 1988) was also administered to detect subclinical changes in mood. Blood samples were drawn at 9 A.M. each session day and frozen at −70°C for later assay. Serum samples of 3-MHPG and HVA levels were assayed separately in batches using gas chromatography and mass spectrometry, with deuterated internal standards. HVA was measured as its methylated, then acetylated, derivative (Warsh et al. 1987) and MHPG was measured as its 4-acetyl-di-trifluoroacetyl derivative (Takahashi et al. 1977).
Data were analyzed using repeated measures analysis of variance (ANOVA) with one between-subjects variable: order of session, and two within-subjects variables: time of assessment (5 time points), and session (AMPT, diphenhydramine). Post hoc paired t-tests were conducted to determine which time points showed significant differences. We also analyzed the peak Ham-20 score (highest score at any time point during drug administration) and the ΔHam-20 score (change score calculated by subtracting the baseline Ham-20 score from the peak Ham-20 score). Clinical relapse rates (defined as at least 100% increase in Ham-20 score from baseline to a score of 12 or greater) were compared using McNemar's test for proportions. All results are reported as mean ± SD.
RESULTS
Ten patients started the protocol but one patient withdrew after one session because of scheduling conflicts; analysis is based on the 9 patients (1 male, 8 female) completing the protocol. The SAD patients had, on average, 13.1 ± 9.4 past episodes of winter depression, but had been in clinical remission for an average of 14.8 ± 3.9 weeks (range: 11 to 22 weeks).
Figure 1 shows the serum HVA and MHPG concentrations during the AMPT and diphenhydramine sessions. There were no significant differences in baseline (Day 1, 9 A.M.) levels between the two sessions. The repeated measures ANOVA found significant main effects of time and session, and significant session-by-time interaction effects, for each of the HVA and MHPG results. As expected, AMPT significantly reduced serum HVA and MHPG by an average of 49% and 57% of baseline levels, respectively, while diphenhydramine had only minimal increases of 14% and 9%, respectively. There were no significant main effects of order, or interaction effects with session, for either of the serum data sets.
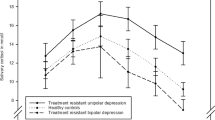
Figure 2 shows the HAM-20 scores of the SAD patients during the active AMPT and sham diphenhydramine depletion sessions. There were no significant differences in baseline, pre-drug scores between the two sessions (t = 0.8, df = 8, p < .45). There were significant main effects of session (F = 30.1, df = 1, p < .001) and time (F = 7.2, df = 1, p < .03), and a significant session-by-time interaction effect (F = 5.5, df = 1, p < .05). There were no significant effects of order of session. Post hoc paired t-tests showed that the Ham-20 scores were significantly higher during the AMPT session at time points Day 2, 9 A.M. (t = 3.6, df = 8, p < .01), Day 2, 4 P.M. (t = 2.6, df = 8, p < .03) and Day 3, 9 A.M. (t = 3.1, df = 8, p < .02). The peak Ham-20 scores were also significantly higher during the AMPT session compared with the diphenhydramine session (16.6 ± 4.8 vs. 8.7 ± 6.2, respectively; t = 4.7, df = 8, p < .002), as were the ΔHam-20 scores (13.8 ± 3.6 vs. 7.8 ± 6.2, respectively; t = 3.4, df = 8, p < .01).
Inspection of individual patient responses found that all nine patients showed significant clinical relapse, as previously defined, at some time point during the AMPT session, while two patients had clinical relapse during the diphenhydramine session (100% vs. 22%, respectively; p < .02 by McNemar's test). The patient who completed only a single session was found to be on AMPT, and she also showed a clinical relapse during the session. Analyses of both the Mood item score on the Ham-20 and the Depression-Dejection subscale of the POMS showed higher scores (i.e., more depressed mood) during the AMPT session (F = 18.8, df = 1, p < .002 and F = 5.3, df = 1, p < .05, respectively).
All subjects had depression scores back within the normal range within 48 h of discontinuing medications (i.e., by Day 4). None of the subjects had serious adverse effects from the study medications.
DISCUSSION
The primary finding of this study was that patients with SAD, in untreated, natural summer remission, experienced transient depressive relapses during the catecholamine depletion session, but not during an active control session. These depressive relapses were both statistically and clinically significant.
There are some limitations of the study design: AMPT depletion significantly reduced serum levels of metabolites of DA and NE within the time course of the behavioral changes, but there are no measures of brain catecholamine activity. AMPT, however, readily crosses the blood-brain barrier so that central effects can be expected based on the effects on peripheral measures. The AMPT also has significant sedative side effects, and some items in the behavioral measures of depression include items for fatigue and energy loss. Sedation likely explains the modest increase in Ham-20 score during Day 1 of the diphenhydramine session. The large increases in Ham-20 score with AMPT cannot be attributed solely to sedative effects, however, because the Ham-20 mood item and the POMS depression-dejection subscale results parallel the Ham-20 findings. Hence, the core symptoms of depression were experienced during AMPT use, not just fatigue or physical symptoms.
Within these limitations, catecholamine depletion appears to induce depressive relapses in SAD patients during an untreated period of remission. This may indicate that catecholamine depletion is a vulnerability or trait marker for SAD. This finding may not be specific to SAD, however, as patients with a history of nonseasonal depression may also show AMPT-induced relapses (Berman et al. 1999). It is also possible that reduced central catecholamines levels in winter directly cause depressive episodes in SAD. If so, patients with mild depressive symptoms early in the autumn/winter should experience worsening of their depression with further reduction of catecholamines with AMPT. This does not appear to be true in nonseasonal depression, since an AMPT study did not find worsening of mood in untreated depressed patients (Miller et al. 1996). It will be thus be important to determine how depressed SAD patients respond to AMPT depletion in winter.
It is of interest to compare the results of catecholamine depletion in SAD with those of tryptophan depletion. The therapeutic effect of light therapy is reversed by both AMPT depletion and tryptophan depletion (Neumeister et al. 1998b). However, effects of tryptophan depletion in SAD patients in summer remission are less consistent. One study found a significant clinical relapse (Neumeister et al. 1998a), while another study did not (Lam et al. 2000). This parallels the findings in nonseasonal depression, where some studies have shown tryptophan depletion-induced relapses in remitted patients (Smith et al. 1997), while others have not (Leyton et al. 1997; Moore et al. 1998).
Finally, the AMPT depletion results in reducing both DA and NE. Depletion studies using more specific medications may help to determine which neurotransmitter is important in the behavioral response. For example, fusaric acid can inhibit DOPA decarboxylase and reduce NE, but not DA (Nagatsu et al. 1970; Matta and Wooten 1973; Goodwin and Sack 1974; Hartmann et al. 1983). Combining AMPT and fusaric acid depletion in the same patients would differentiate the contributions of NE and DA to the depressive response.
References
Anderson JL, Vasile RG, Mooney JJ, Bloomingdale KL, Samson JA, Schildkraut JJ . (1992): Changes in norepinephrine output following light therapy for fall/winter seasonal depression. Biol Psychiatry 32: 700–704
Arbisi PA, Depue RA, Krauss S, Spoont MR, Leon A, Ainsworth B, Muir R . (1994): Heat-loss response to a thermal challenge in seasonal affective disorder. Psychiatry Res 52: 199–214
Arbisi PA, Depue RA, Spoont MR, Leon A, Ainsworth B . (1989): Thermoregulatory response to thermal challenge in seasonal affective disorder: a preliminary report. Psychiatry Res 28: 323–334
Barbato G, Moul DE, Schwartz P, Rosenthal NE, Oren DA . (1993): Spontaneous eye blink rate in winter seasonal affective disorder. Psychiatry Res 47: 79–85
Berman RM, Narasimhan M, Miller HL, Anand A, Cappiello A, Oren DA, Heninger GR, Charney DS . (1999): Transient depressive relapse induced by catecholamine depletion: potential phenotypic vulnerability marker? Arch Gen Psychiatry 56: 395–403
Bunney WEJ, Brodie HK, Murphy DL, Goodwin FK . (1971): Studies of alpha-methyl-para-tyrosine, L-dopa, and L-tryptophan in depression and mania. Am J Psychiatry 127: 872–881
Depue RA, Arbisi P, Krauss S, Iacono WG, Leon A, Muir R, Allen J . (1990): Seasonal independence of low prolactin concentration and high spontaneous eye blink rates in unipolar and bipolar II seasonal affective disorder. Arch Gen Psychiatry 47: 356–364
Depue RA, Arbisi P, Spoont MR, Krauss S, Leon A, Ainsworth B . (1989): Seasonal and mood independence of low basal prolactin secretion in premenopausal women with seasonal affective disorder. Am J Psychiatry 146: 989–995
Depue RA, Iacono WG, Muir R, Arbisi P . (1988): Effect of phototherapy on spontaneous eye blink rate in subjects with seasonal affective disorder. Am J Psychiatry 145: 1457–1459
Dilsaver SC, Qamar AB, Del Medico VJ . (1992): The efficacy of bupropion in winter depression: results of an open trial. J Clin Psychiatry 53: 252–255
Engelman K, Horwitz D, Jequier E, Sjoerdsma A . (1968): Biochemical and pharmacologic effects of alpha-methyltyrosine in man. J Clin Invest 47: 577–594
Goodwin FK, Sack RL . (1974): Behavioral effects of a new dopamine-beta-hydroxylase inhibitor (fusaric acid) in man. J Psychiatr Res 11: 211–217
Hartmann E, Oldfield M, Adelman S, Edelberg R . (1983): Psychological effects of dopamine beta-hydroxylase inhibition: a failure to replicate. Psychopharmacology 79: 352–356
Lam RW, Bowering TA, Tam EM, Grewal A, Yatham LN, Shiah IS, Zis AP . (2000): Effects of rapid tryptophan depletion in patients with seasonal affective disorder in natural summer remission. Psychol Med 30: 79–87
Lam RW, Levitan RD . (2000): Pathophysiology of seasonal affective disorder: a review. J Psychiatr Neurosci 25: 469–480
Lam RW, Levitt AJ . (1999): Canadian Consensus Guidelines for the Treatment of Seasonal Affective Disorder. Vancouver BC, Clinical & Academic Publishing
Leyton M, Young SN, Blier P, Ellenbogen MA, Palmour RM, Ghadirian AM, Benkelfat C . (1997): The effect of tryptophan depletion on mood in medication-free, former patients with major affective disorder. Neuropsychopharmacology 16: 294–297
Matta RJ, Wooten GF . (1973): Pharmacology of fusaric acid in man. Clin Pharmacol Ther 14: 541–546
McNair DM, Lorr D, Droppelman LF . (1988): Manual for the Profile of Mood States. San Diego, CA, Educational Testing Services.
Miller HL, Delgado PL, Salomon RM, Heninger GR, Charney DS . (1996): Effects of alpha-methyl-para-tyrosine (AMPT) in drug-free depressed patients. Neuropsychopharmacology 14: 151–157
Moore P, Gillin JC, Bhatti T, Demodena A, Seifritz E, Clark C, Stahl Rapaport M, Kelsoe J . (1998): Rapid tryptophan depletion, sleep electroencephalogram, and mood in men with remitted depression on serotonin reuptake inhibitors. Arch Gen Psychiatry 55: 534–539
Nagatsu T, Hidaka H, Kuzuya H, Takeya K, Umezawa H . (1970): Inhibition of dopamine beta-hydroxylase by fusaric acid (5-butylpicolinic acid) in vitro and in vivo. Biochem Pharmacol 19: 35–44
Neumeister A, Praschak-Rieder N, Hesselmann B, Vitouch O, Rauh M, Barocka A, Kasper S . (1998a): Effects of tryptophan depletion in fully remitted patients with seasonal affective disorder during summer. Psychol Med 28: 257–264
Neumeister A, Turner EH, Matthews JR, Postolache TT, Barnett RL, Rauh M, Vetticad RG, Kasper S, Rosenthal NE . (1998b): Effects of tryptophan depletion vs catecholamine depletion in patients with seasonal affective disorder in remission with light therapy. Arch Gen Psychiatry 55: 524–530
Oren DA, Moul DE, Schwartz PJ, Wehr TA, Rosenthal NE . (1994): A controlled trial of levodopa plus carbidopa in the treatment of winter seasonal affective disorder: a test of the dopamine hypothesis. J Clin Psychopharmacol 14: 196–200
Rosenthal NE, Sack DA, Gillin JC, Lewy AJ, Goodwin FK, Davenport Y, Mueller PS, Newsome DA, Wehr TA . (1984): Seasonal affective disorder: a description of the syndrome and preliminary findings with light therapy. Arch Gen Psychiatry 41: 72–80
Rosenthal NE, Skwerer RG, Sack DA, Duncan CC, Jacobsen FM, Tamarkin L, Wehr TA . (1987): Biological effects of morning-plus-evening bright light treatment of seasonal affective disorder. Psychopharmacol Bull 23: 364–369
Rudorfer MV, Skwerer RG, Rosenthal NE . (1993): Biogenic amines in seasonal affective disorder: effects of light therapy. Psychiatry Res 46: 19–28
Schwartz PJ, Murphy DL, Wehr TA, Garcia-Borreguero D, Oren DA, Moul DE, Ozaki N, Snelbaker AJ, Rosenthal NE . (1997): Effects of meta-chlorophenylpiperazine infusions in patients with seasonal affective disorder and healthy control subjects. Diurnal responses and nocturnal regulatory mechanisms. Arch Gen Psychiatry 54: 375–385
Smith KA, Fairburn CG, Cowen PJ . (1997): Relapse of depression after rapid depletion of tryptophan. Lancet 349: 915–919
Takahashi S, Godse DD, Warsh JJ, Stancer HC . (1977): A gas chromatographic-mass spectrometric (GC-MS) assay for 3-methoxy-4-hydroxyphenethyleneglycol and vanilmandelic acid in human serum. Clin Chim Acta 81: 183–192
Warsh JJ, Godse DD, Li PP . (1987): Quantitation of catecholamine metabolites by gas chromatography-mass spectrometry with selected ion monitoring. Methods Enzymol 142: 571–582
Williams JBW, Gibbon M, First MB . (1992): The Structured Clinical Interview for DSM-III-R (SCID), I: history, rationale, and description. Arch Gen Psychiatry 49: 624–629
Williams JBW, Link MJ, Rosenthal NE, Terman M . (1988): Structured Interview Guide for the Hamilton Depression Rating Scale, Seasonal Affective Disorders Version (SIGH-SAD). New York, New York Psychiatric Institute
Acknowledgements
Supported by a grant from the Canadian Psychiatric Research Foundation (to RWL). Preliminary results from this study were presented at the J.C. Gillin Festschrift, Department of Psychiatry, University of California, San Diego, on October 28, 2000, and at the 13th Annual Meeting of the Society for Light Treatment and Biological Rhythms, Stockholm, June 24, 2001. The authors thank Dr. Edward Dunn and the Psychopharmacology Research Laboratory at the Centre for Addiction and Mental Health, Toronto, for assistance with the blood assays.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lam, R., Tam, E., Grewal, A. et al. Effects of Alpha-Methyl-Para-Tyrosine-Induced Catecholamine Depletion in Patients with Seasonal Affective Disorder in Summer Remission. Neuropsychopharmacol 25 (Suppl 1), S97–S101 (2001). https://doi.org/10.1016/S0893-133X(01)00337-2
Issue Date:
DOI: https://doi.org/10.1016/S0893-133X(01)00337-2
Keywords
This article is cited by
-
Neural Correlates of Impaired Reward–Effort Integration in Remitted Bulimia Nervosa
Neuropsychopharmacology (2018)
-
Finding Order in Human Neurological Disorder Using a Tadpole
Current Pathobiology Reports (2015)
-
Association of Changes in Norepinephrine and Serotonin Transporter Expression with the Long-Term Behavioral Effects of Antidepressant Drugs
Neuropsychopharmacology (2009)
-
Illumination controls differentiation of dopamine neurons regulating behaviour
Nature (2008)
-
Norepinephrine Transporter Regulation Mediates the Long-Term Behavioral Effects of the Antidepressant Desipramine
Neuropsychopharmacology (2008)