Abstract
Phospholipase C (PLC) and protein kinase C (PKC) are important components of the phosphoinositide (PI) signaling system. To examine if the abnormalities observed in the PI signaling system of patients with affective disorders, reported in previous studies, are related to abnormalities in one or more of its components, we studied PKC, PI-PLC activity, the expression of their specific isozymes, and expression of myristoylated alanine-rich C-kinase substrate (MARCKS) in platelets obtained from 15 drug-free hospitalized patients with bipolar disorder and 15 with major depressive disorder (unipolar) and from 15 nonhospitalized normal control subjects. We observed a significant decrease in PI-PLC and PKC activity and the expression of selective PKC α, βI, βII, and PLC δ1 isozymes in membrane and cytosol fraction of platelets from bipolar but not unipolar patients. On the other hand, the level of MARCKS was significantly increased in membrane and cytosol fraction of platelets from patients with bipolar but not unipolar disorders. These results suggest that alterations in PKC, PLC, and MARCKS may be involved in the pathophysiology of bipolar illness.
Similar content being viewed by others
Main
In the phosphoinositide (PI) signaling system, agonist stimulation of G-protein–coupled receptors causes hydrolysis of the substrate, phosphatidyl inositol 4,5-bisphosphate (PIP2), by the enzyme phospholipase C (PLC), resulting in the formation of two second messengers, inositol 1,4,5-trisphophate (IP3) and diacylglycerol (DAG) (Berridge and Irvine 1989). IP3 stimulates the release of intracellular calcium from the endoplasmic reticulum, and DAG stimulates the enzyme protein kinase C (PKC) (Nishizuka 1992), which is one of the major intracellular mediators of signals generated by the stimulation of cell surface receptors.
Several studies indicate abnormalities of the PI signaling system in patients with unipolar or bipolar disorders. It has been reported that the hydrolysis of PIP2 by several agonists, such as sodium fluoride (NaF) and GTPγS, is altered in the postmortem brain of depressed suicide victims and bipolar patients (Jope et al. 1996; Pacheco et al. 1996). PI signal transduction determined by serotonin (5HT)-, thrombin-, and NaF-stimulated IP formation has also been reported to be increased in platelets of depressed patients (Mikuni et al. 1991; Karege et al. 1996). These abnormalities may be related to abnormalities in receptors, such as 5HT2A, 5HT2C, muscarinic M1 and M2, or α2 adrenergic receptors linked to the PI signaling system or to abnormal levels of substrates, such as PIP2, or to components of the signaling cascade, such as G-proteins, PKC, or PLC. Abnormalities in 5HT2A (Pandey et al. 1995), α2 adrenergic receptors (Pandey et al. 1990), G-proteins (Garcia-Sevilla et al. 1997; Karege et al. 1998; Gurguis et al. 1999), and levels of PIP2, a substrate for PI-PLC (Brown et al. 1993; Soares and Mallinger 1996; Soares et al. 1999), have been reported in platelets of unipolar and/or bipolar patients.
PLC and PKC are two crucial components of the PI signaling system. Both PKC and PLC have been shown to be involved in a variety of physiological functions, such as synthesis, release, and reuptake of neurotransmitters, neuronal development, transcription, long-term potentiation (LTP), and behavioral responses (Nishizuka 1992). Although the role of PLC in affective disorders has not been fully investigated, some studies have shown abnormalities of PLC in depression and suicide (Pacheco et al. 1996; Pandey et al. 1999). On the other hand, very few studies have examined the role of PKC in bipolar or unipolar disorders, although PKC has been implicated in the pathophysiology of bipolar disorders. For example, it has been reported that PKC activity as well as translocation of PKC from cytosol to membrane are increased in platelets of bipolar patients and that lithium treatment alters the activity of PKC in platelets (Friedman et al. 1993; Wang et al. 1999). Further evidence for the involvement of PKC in bipolar disorders is derived from observations that lithium exerts significant effects on PKC in a number of cell systems, including central nervous system (CNS) (Manji et al. 1993; Manji et al. 1995; Manji and Lenox 1999). Therefore, it has been suggested by some investigators that PKC may be an important target for the action of mood stabilizers, such as lithium and valproate (Lenox and Manji 1998; Ikonomov and Manji 1999; Jope 1999).
Although activation of PKC causes a variety of physiological responses, the steps involved between the activation of PKC and subsequent physiological responses are not known. One approach to examine the molecular steps between the activation of PKC and subsequent physiological responses is study of the substrates for PKC, which may help in understanding the downstream events. The activation of PKC causes phosphorylation of a number of membrane-associated protein substrates, such as myristoylated alanine-rich C-kinase substrate (MARCKS), which is a 30-kilodalton (kD) acidic and heat-stable protein (Aderem 1992; Blackshear 1993; Aderem 1995) that is highly expressed in developing and adult brain. MARCKS contains a basic middle region, termed the effector domain, that binds acidic phospholipids, actin, and calcium/calmodulin (Yamauchi et al. 1998). It also contains PKC phosphorylating sites, which are in close proximity to the effector domain. MARCKS is anchored to membranes by an amino-terminal myristic acid moiety and by the electrostatic interaction of the effctor domain to the acidic membrane phospholipids, phosphatidyl serine and PIP2 (McLaughlin and Aderem 1995). MARCKS has been implicated in many cellular functions, including secretion (Goodall et al. 1997), phagocytosis, and actin membrane interactions (Allen and Aderem 1995; Myat et al. 1997). MARCKS can inhibit PLC in vitro by sequestering its substrate, PIP2 (Glaser et al. 1996), suggesting that MARCKS may modulate the availability of this lipid.
Because PKC has been implicated as a possible site for the therapeutic action of lithium, interactions of MARCKS with the short-term and long-term effects of lithium have been studied in immortalized hippocampal cells as well as in rat brain. Administration of lithium causes the downregulation of MARCKS in rat hippocampus (Lenox et al. 1992), and in immortalized hippocampal cells (Watson et al. 1994; Watson and Lenox 1996; Wang et al. 2000), suggesting a relationship between bipolar disorders and alteration in MARCKS. Although MARCKS has been studied in postmortem brain of suicide victims (McNarmara et al. 1999), there have been no studies of MARCKS in patients with bipolar or unipolar disorders.
To test the hypothesis that the abnormalities of the PI signaling system observed in brain and platelets of patients with affective disorders may be related to abnormalities in one or more of its components, and that these abnormalities may cause downstream changes in the PI signaling system, we studied PI-PLC and PKC activity and expression of their specific isozymes and expression of MARCKS in platelets of drug-free patients with unipolar or bipolar disorders and normal control subjects.
METHODS
Patients
These studies were conducted in patients with bipolar or unipolar disorders admitted to the Psychiatric Clinical Research Center, as a part of the General Clinical Research Center (GCRC), University of Illinois at Chicago. This study was approved by the Institutional Review Board of the University of Illinois at Chicago.
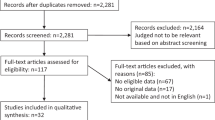
The comparison subjects were nonhospitalized normal control subjects. The control subjects for unipolar and bipolar groups were not the same, although the number of control subjects is the same in both groups (n = 15). All patients gave informed consent for the study and were kept drug free for a period of up to 2 weeks. During the drug-free washout period, blood was obtained for the studies and clinical assessments were performed. Normal controls were drug free at the time the blood was drawn and abstained from alcohol at least 2 days before blood drawing.
Clinical Assessments
Patients were diagnosed as having bipolar disorder or major depressive disorder (herein referred to as unipolar disorder) according to Research Diagnostic Criteria (RDC) and the DSM-IV criteria derived by consensus between two trained raters and also based on clinical interviews as well as all other available clinical information. Diagnostic and clinical assessments were conducted at admission and at discharge. The discharge diagnosis was considered definitive. Behavioral ratings included the Hamilton Depression Rating Scale (HDRS) and the Clinician-Administered Rating Scale for Mania (CARS-M) (Altman et al. 1994).
Normal controls were recruited for the study through advertisements on hospital notice boards, by referral from normal controls, or by referral from hospital employees. Control subjects had no history of psychiatric or major medical disorders. The normal controls abstained from any medication for at least 2 weeks before assessment and blood drawing. All subjects gave informed consent for the study.
Isolation of Platelets
Human venous blood was collected into a tube containing 3.8% (wt/vol) sodium citrate (1 vol:9 vol blood). The blood was centrifuged immediately at 210 g for 10 min at 4°C to obtain platelet-rich plasma, which was centrifuged at 4000 g for 10 min at 4°C to obtain the platelet pellet. The pellet was resuspended in Tris-HCl buffer (pH 7.4) and centrifuged at 4000 g to obtain the final platelet pellet.
Preparation of Membrane and Cytosol Fractions
The platelet pellet was homogenized in homogenizing buffer containing 20 mM Tris-HCl (pH 7.4), 2 mM ethylene glycol-bis (β-aminoethyl ether) -N,N,N′,N′-tetraacetic acid, 5 mM ethylenediamine tetraacetic acid, 1.5 mM pepstatin, 2 mM leupeptin, 0.5 mM phenylmethylsulfonyl fluoride, 0.2 units/ml aprotinin, and 2 mM dithiothreitol using the Polytron®. The supernatant was centrifuged at 100,000 g for 60 min at 4°C. The resulting supernatant was the cytosol fraction, and the pellet was resuspended in the homogenizing buffer containing 0.2% (wt/vol) Triton X-100. The homogenate was kept at 4°C for 60 min with occasional stirring and then centrifuged at 100,000 g for 60 min at 4°C. The resulting supernatant was used as the membrane fraction. The concentration of protein in these fractions was determined using the procedure of Lowry et al. (1951).
Determination of PKC Activity in Membrane and Cytosol Fractions
PKC activity in membrane and cytosol fractions was measured by the procedure described earlier by us (Dwivedi and Pandey 1999a). An Amersham enzyme assay kit was used to determine PKC activity. A PKC-specific target peptide and all the necessary cofactors were provided in the kit. Assay tubes (with a final incubation volume of 75 μl) contained 25 μl of a component mixture [3 mM Ca(C3H302)2, 75 μg/ml L-α-phosphatidyl-L-serine, 6 μg/ml phorbol 12-myristate 13-acetate, 225 μM substrate peptide, and 7.5 mM dithiothreitol in 50 mM Tris-HCl containing 0.05% sodium azide, pH 7.5] and 25 μl of the membrane or cytosol fraction. The reaction was initiated by addition of 25 μl of Mg-ATP buffer (10 μCi/ml [γ32P]ATP, 1.2 mM ATP, 72 mM MgC12, and 30 mM HEPES, pH 7.4) to each tube. The tubes were incubated for 15 min at 37°C, and the reaction was terminated by addition of 100 μl of the “stop” reagent (300 mM orthophosphoric acid containing corrosive acid) to each tube. An aliquot of the solution from each tube (35 μl) was blotted onto individual peptide-binding papers. Papers were washed with 75 mM phosphoric acid twice for 5 min. Papers were dried, and the retained radioactivity was counted by a liquid scintillation counter. The result was expressed as nanomoles per minute per milligram of protein. Before starting our experiments, the specificity of the PKC assay in membrane and cytosol fractions was determined using staurosporine (100 nM) as the PKC inhibitor. It was observed that in the presence of staurosporine, PKC activity was inhibited by 99.94%.
Determination of PI-PLC Activity in Membrane and Cytosol Fractions
PI-PLC activity was measured in both membrane and cytosol fractions by the procedures described earlier by us (Dwivedi and Pandey 1999b) using 5 μg protein/tube in an incubation buffer (20 mM Tris-HCl, 1 mM CaCl2, and 100 mM KCl, pH 7.4) containing 10 mM lithium chloride, PIP2 substrate (50 μM unlabeled PIP2, 2.0 μCi/ml [3H] PIP2, and 0.5 mg/ml certimide) in a total volume of 100 μl at 37°C for 10 min. The reaction was terminated by the addition of 500 μl of 1 M HCl and 500 μl of a mixture of chloroform/methanol (l:l vol/vol). The tubes were vigorously mixed and centrifuged at 1000 g for 10 min. The aqueous (upper) phase was transferred to a scintillation vial containing scintillation liquid, and the radioactivity was counted in a liquid scintillation counter. Each experiment had its blank, in which the protein suspension was added after stopping the reaction with chloroform/methanol. PI-PLC activity is expressed as the amount of [3H]IP3 formed (dpm) per minute per milligram of protein.
Quantitation of PKC and PLC Isozymes and MARCKS in Membrane and Cytosol Fractions by Western Blot
Immunolabeling of PKC α, βI, βII, δ, and PLC β1, δ1, and γl isozymes was determined as described previously (Dwivedi and Pandey 1999a; Dwivedi and Pandey 1999b). Equal volumes of tissue samples and gel loading solution (50 mM Tris-HCl [pH 6.8], 4% β-mercaptoethanol, 1% sodium dodecylsulfate (SDS), 40% glycerol, and bromphenol blue) were mixed, and the tissue samples were boiled for 3 min and then kept on ice for 10 min. The tissue samples (30 μg protein in each lane) were loaded onto 7.5% (wt/vol) acrylamide gel using the Mini Protein II gel apparatus (BioRad, Hercules, CA). The gels were run using 25 mM Tris-base, 192 mM glycine, and 0.1% (wt/vol) SDS at 150 volts. The proteins were subsequently transferred electrophoretically to an ECL nitrocellulose membrane (Amersham, Piscataway, NJ) using the Mini Trans Blot transfer unit (BioRad) at 0.150 amp constant current. Membranes were washed with TBST buffer (10 mM Tris-base, 0.15 M NaCl, and 0.05% [vol/vol] Tween 20) for 10 min. The blots were blocked by incubating with 5% (wt/vol) powdered nonfat milk in TBST, 2 ml nonidet P-40, and 0.02% (wt/vol) SDS (pH 8.0). The blots were then incubated with anti-MARCKS or anti-PKC α, βI, βII, or δ antibodies overnight at 4°C or with anti-PLC β1, δ1 or γl antibodies for 90 min at 21°C. The dilution of antibodies ranged from 1:3000 to 1:5000 depending on the antibody used. Membranes were washed with TBST and incubated with horseradish peroxidase–linked secondary antibody (anti-rabbit or anti-mouse IgG) for 1–5 h at room temperature. Membranes were extensively washed with TBST and exposed to enhanced chemiluminescent (ECL) film. Membranes were stripped using stripping solution (Chemicon International, Temecula, CA), and monoclonal β-actin antibody (1:5000 for 2 h) was probed, followed by secondary anti-mouse IgG antibody (1:5000 for 2 h). The bands on the autoradiogram were quantified using the Loats Image Analysis System (Westminster, MD), and the optical density of each band of the PKC and the PLC isozymes was corrected by the optical density of the corresponding β-actin band. The values are represented as a percentage of the control. β-actin was used as internal control to reduce interblot variability.
Statistical Analysis
The statistical analysis of the data was performed using the SPSS software for Windows version 9.0 (SPSS Inc.). Results are expressed as the mean ± standard deviation (SD). The comparison of data between normal controls and unipolar and normal controls and bipolar patients was performed by using an independent sample (two-tailed) t-test for equal or unequal variance as appropriate. We performed the t-test because the control subjects for unipolar and bipolar studies were different. A Pearson correlation product moment analysis was applied to determine the relationship of PKC, PI-PLC activity, and immunolabeling of PKC and PLC isozymes and MARCKS with age, gender, HDRS, and CARS-M.
RESULTS
Effect of Age and Gender on PKC, PLC, and MARCKS
We determined PKC, PLC, and MARCKS in 15 patients with bipolar disorders, 15 patients with unipolar disorders, and 15 normal control subjects (referred to as normal controls). The demographic and clinical characteristics of the study subjects are shown in Table 1 . The symptom scores (HDRS and CARS-M) are provided in Table 1. Manic patients had higher CARS-M scores than bipolar depressed or unipolar patients, and unipolar patients had higher HDRS scores than bipolar manic patients. The mean length of illness for bipolar patients was 11.5 ± 7.4 years, and bipolar patients had been treated with a variety of medications, for example, risperidone, depakote, and lithium, before admission. Only one patient with unipolar illness was on fluoxetine at the time of admission for the study. There were no significant differences in the ages of patients and normal control subjects. The male/female ratio was similar in all groups. To examine if age or gender had any significant effect on PKC, PLC, or MARCKS, we determined the correlation between age and gender with PKC, PLC, and MARCKS. We did not observe any significant correlation of age and gender with any of the measures of PKC, PLC, or MARCKS.
PKC Activity and Immunolabeling of PKC Isozymes in Platelets of Bipolar and Unipolar Patients and Normal Control Subjects
We determined PKC activity in membrane and cytosol fractions from bipolar patients and normal control subjects, and the results are shown in Figure 1A.. There was a significant decrease in PKC activity in membrane and cytosol fractions of platelets from bipolar patients compared with normal subjects. To determine if there was an alteration in the ratio of PKC activity in platelets of bipolar patients, we calculated the ratio of PKC activity in membrane and cytosol fractions. Although there was a decrease in PKC activity in membrane and cytosol fractions of platelets from bipolar patients, there were no significant differences in membrane-to-cytosol ratio in PKC activity between control subjects (0.34 ± 0.04) and bipolar patients (0.30 ± 0.12). These results indicated that the decrease in PKC activity in membrane and cytosol fractions observed in platelets of bipolar patients was not related to an abnormal translocation of PKC.
When we compared PKC activity in membrane and cytosol fractions of unipolar patients with those of normal controls, we did not find any significant differences in PKC activity (Figure 1B). We also did not find any significant difference in membrane-to-cytosol ratio of PKC activity between these two groups. These results indicated that a decrease in PKC activity in membrane and cytosolic fractions was observed in platelets of bipolar but not unipolar patients.
Because we observed a decrease in PKC activity in membrane and cytosol fractions of platelets of bipolar patients, we next examined if this decrease was related to the altered expression of any of the PKC isozymes. We determined the immunolabeling of PKC isozymes in membrane and cytosol fractions of platelets from bipolar and unipolar patients and normal control subjects. Figure 2A.. shows representative immunoblots of various isozymes of PKC in membrane and cytosol fractions of one normal control and one bipolar patient. As reported in the literature, PKC α, βI, and βII isozymes migrated to 80 kD, whereas PKC δ migrated to 78 kD. The molecular mass of β-actin was 46 kD. As can be seen in Figure 2A, there is an apparent decrease in the levels of PKC α, PKC βI, and PKC βII isozymes in membrane and cytosol fractions of platelets obtained from one bipolar patient. Mean levels of PKC isozymes in bipolar patients and normal control subjects are graphically shown in Figure 2B. Comparison of PKC isozymes in bipolar patients and normal control subjects revealed that PKC α, PKC βI, and PKC βII levels were significantly decreased in membrane and cytosol fractions of platelets from bipolar patients, whereas no differences were observed in PKC δ compared with normal control subjects. As observed with PKC activity, none of the PKC isozymes showed any significant differences in membrane or cytosol fractions of platelets of unipolar patients compared with normal controls. The mean and SD values (percentage of control) for various PKC isozymes in bipolar patients against normal controls are as follows: membrane: PKC α, 99.28 ± 39.12; PKC βI, 97.63 ± 38.40; PKC βII, 96.79 ± 39.00; PKC δ, 107.01 ± 37.28; cytosol: PKC α, 105.44 ± 37.96; PKC βI, 104.55 ± 40.97; PKC βII, 107.40 ± 46.16; PKC δ, 103.91 ± 45.01.
(A) Representative Western blots of PKC isozymes in membrane and cytosol fractions of platelets from one normal control and one bipolar subject. Protein samples (30 μg) were electrophoresed on 7.5% polyacrylamide gel followed by electrotransfer to intracellulose membrane. The blots were probed with monoclonal anti-PKC α, βI, βII, or δ antibody (1:3000 dilution). The molecular weights for PKC α, βI, and βII was 80 kD, whereas for PKC δ, it was 78 kD. The blots were stripped and reprobed with β-actin antibody (1:5000 dilution). β-Actin migrated to 46 kD. The ratios of the optical densities of PKC α, βI, βII, and δ to the optical density of β-actin were calculated. (B) Immunolabeling of PKC isozymes in membrane and cytosol fractions of platelets from normal controls and bipolar patients. Values are the mean ± SD. The bipolar group was compared with the normal control group. p values are a, .001; b, .002; c, .003; d, .03; e, .014.
PI-PLC Activity and Immunolabeling of PLC Isozymes in Platelets of Bipolar and Unipolar Patients and Normal Control Subjects
We determined PI-PLC activity in platelets of 15 bipolar patients,15 unipolar patients, and 15 normal control subjects. We observed that PI-PLC activity was significantly decreased in membrane and cytosol fractions of platelets from bipolar patients compared with normal control subjects, as shown in Figure 3A.. On the other hand, there was no significant difference in PI-PLC activity between unipolar patients and normal controls (Figure 3B). To examine if the decrease in PI-PLC activity was related to any specific isozymes of PLC, we determined the immunolabeling of several isozymes of PLC (β1, δ1,γ1) in bipolar patients and normal control subjects. Figure 4A. shows a representative immunoblot depicting the levels of various PLC isozymes in membrane and cytosol fractions of a bipolar patient and a normal control subject. PLC β1 migrated to 96 kD, whereas PLC δ1 and γ1 migrated to 85 and 150 kD, respectively. As can be seen in Figure 4A, there appeared to be a decrease in the levels of PLC δ1 in membrane and cytosol fractions but not in other PLC isozymes. Figure 4B shows the mean levels of PLC isozymes in platelets of bipolar patients and normal control subjects. Similar to the observation in the representative immunoblots, there was a significant decrease in PLC δ1 levels in membrane and cytosol fractions of platelets from bipolar patients and normal control subjects; however, there were no significant differences in PLC β1 or γ1, either in membrane or cytosol fractions of platelets from bipolar patients and normal control subjects. These results indicate that PI-PLC activity and expression of PLC δ1 but not of PLC β1 or γ1 are significantly decreased in membrane and cytosolic fractions of platelets from bipolar patients. As with PI-PLC activity, the immunolabeling of PLC isozymes in both membrane and cytosol fractions in platelets of unipolar patients was not different from normal controls. The mean and SD values (percentage of control) for PLC isozymes in unipolar patients against normal controls is as follows: membrane: PLC βI, 101.42 ± 42; PLC γ1, 93.15 ± 44.74; PLC δ1, 104.93 ± 34.69; cytosol: PLC β1, 98.16 ± 42.24; PLC γ1, 109.81 ± 36.79; PLC δ1, 107.86 ± 35.79.
(A) Representative Western blots of PLC isozymes in membrane and cytosol fractions of platelets from one normal control and one bipolar subject. Protein samples (30 μg) were electrophoresed on 7.5% polyacrylamide gel and then electrotransferred to intracellulose membrane. The blots were probed with monoclonal anti-PLC β1, δ1, or -γ1 antibodies (1:1000 dilution). The molecular weights for the PLC β1, δ1, and γ1 isozymes were 96, 150, and 85 kD, respectively. The blots were stripped and reprobed with β-actin antibody (1:5000 dilution). β-actin migrated to 46 kD. The ratios of the optical densities of PLC β1, δ1, or γ1 to the optical density of β-actin were calculated. (B) Immunolabeling of PLC isozymes in membrane and cytosol fractions of platelets from normal controls and bipolar patients. Values are the mean ± SD. The bipolar group was compared with the normal control group. p values are a, .009; b, .001.
MARCKS Expression in Platelets of Bipolar Patients, Unipolar Patients, and Normal Control Subjects
MARCKS is one of the primary substrates for PKC action and has been implicated in the therapeutic action of lithium. Because we found a decrease in PKC activity and in some PKC isozymes in platelets of bipolar patients, we examined whether these decreases were associated with changes in MARCKS expression. We therefore determined levels of MARCKS in platelets of bipolar patients, unipolar patients, and normal control subjects. Representative Western blots showing immunolabeling of MARCKS in one normal control and one bipolar patient in membrane and cytosol fractions are depicted in Figure 5A.. MARCKS migrated to 46 kD. The comparison of MARCKS expression in patients shows that the level of MARCKS was significantly increased in the cytosol and membrane fractions of platelets from bipolar patients (Figure 5B) but not in those from unipolar patients (Figure 5C) compared with normal control subjects.
(A) Representative Western blots of MARCKS protein in membrane and cytosol fractions of platelets from one normal control and one bipolar subject. Protein samples (20 μg) were electrophoresed on 7.5% polyacrylamide gel and then electrotransferred to nitrocellulose membrane. The blots were probed with monoclonal anti-MARCKS antibody (1:1000 dilution). The molecular weight of MARCKS was 30 kD. The blots were stripped and reprobed with β-actin antibody (1:5000 dilution). β-Actin migrated to 46 kD. The ratio of the optical density of MARCKS to the optical density of β-actin was calculated. (B and C) Bar diagrams of the immunolabeling of MARCKS in platelets of bipolar and normal controls (B) and unipolar and normal controls (C). Values are the mean ± SD. The bipolar or unipolar group was compared with the normal control group. p values are a, .004; b, .016
DISCUSSION
This study demonstrates a decrease in PKC and PI-PLC activity in membrane and cytosol fractions of platelets obtained from drug-free bipolar patients and a significant decrease in the expression of specific isoforms of PKC and PLC, that is, PKC α, PKC βI, PKC βII, and PLC δ1. We also observed that the levels of MARCKS are significantly increased in membrane and cytosol fractions in platelets from bipolar patients; however, there were no significant changes in PKC and PI-PLC activity, their isozymes, or the levels of MARCKS in either membrane or cytosol fractions of platelets from unipolar patients compared with normal controls.
Because we did not observe any changes in PKC, PLC, or MARCKS in platelets of unipolar patients, we examined whether the changes in PKC, PLC, or MARCKS are related to the manic or the depressed phase of bipolar patients. Of the 15 patients we studied, 6 were in the manic phase, 5 were in the depressed phase, and 4 were mixed. We found that there was no significant difference in PKC and PI- PLC activity or in the levels of any of the isozymes of PKC, PLC, or MARCKS among bipolar patients in the manic, depressed, or mixed phases. However, PKC and PI-PLC activity and expression of PLC δ1, PKC α, PKC βI, and PKC βII were significantly decreased and levels of MARCKS were increased in platelets of bipolar patients in either the manic or the depressed phase compared with control subjects.
We next examined if the decreased PKC activity was related to changes in any of the specific PKC isozymes. PKC consists of a family of at least 12 closely-related isoforms that are differentially activated by phospholipids and Ca2+ and have been classified according to their co-factor dependency. The conventional isoforms of PKC, consisting of α, βI and βII, and γ, are calcium dependent in their activity, whereas the novel PKCs, δ, ɛ, η, and ξ isozymes, are calcium independent, and the atypical PKCs have reduced sensitivity to phorbol esters (Nishizuka 1992). Initially, we characterized the immunolabeling of PKC isozymes in human platelets and, as observed by other investigators (Baldassare et al. 1992; Grabarek et al. 1992), we found that the platelets contain PKC α, βI, βII, and δ isozymes. However, we could not detect any band for PKC γ and ɛ isozymes. Our results show a significant decrease in PKC α, βI, and βII, but not PKC δ in both membrane and cytosol fractions of platelets of bipolar patients compared with normal control subjects. Because PKC α and β isozymes belong to the Ca2+-dependent family of PKC isozymes, our results suggest that the decrease in PKC activity in platelets of bipolar patients is restricted to the conventional Ca2+-dependent enzymes and is not found in Ca2+-independent PKC isozymes.
Previous studies of PKC activity or PKC isozymes in bipolar patients are very limited. The observations by Friedman et al. (1993) and Wang et al. (1999) that PKC activity is increased in the platelets of bipolar patients during the manic phase is contrary to our observations. Young et al. (1999) did not find any differences in PKC α either in membrane or cytosol fractions of platelets between bipolar patients and normal control subjects. Soares et al. (2000) found a significant decrease in PKC α but not PKC βI, βII, δ, and ɛ in platelets of lithium-treated patients compared with control subjects. Whereas the discrepancy between our results and those of Soares et al. (2000) could be attributed to previous treatment with lithium, the reasons for discrepancy in our results and those of Friedman et al. (1993) and Young et al. (1999) are unclear.
Several mechanisms may be associated with the decrease in PKC activity and PKC isoforms observed in bipolar patients in this study. Hyperactive PI signaling has previously been observed in postmortem brain of bipolar patients (Jope et al., 1996). A sustained increase in phosphoinositide metabolism resulting in increased levels of DAG may cause a desensitization in PKC activity and a decrease in the expression of PKC isoforms as a result of persistent stimulation of PKC by increased levels of DAG. Such an explanation is consistent with a recent report by Manji and Lenox (1999), who observed a decrease in PKC α by in vitro exposure of HN33 cells to lithium. They attributed this decrease to an increase in the formation of DAG, which is responsible for the activation of PKC. It has also been argued that the activation of PKC is often followed by its rapid proteolytic degradation (Kishimoto et al. 1989; Young et al. 1999). The overactive PI signaling in platelets of bipolar patients reported by several investigators may result in the increased formation of DAG and the activation and translocation of PKC to membrane and its subsequent proteolytic degradation. Whether such a mechanism in fact causes PKC downregulation in platelets of bipolar patients needs to be further tested. On the other hand, it is also possible that changes in PKC or PLC may be unrelated to a hyperactive PI signaling system and that these are abnormal in this part of the signaling system in BP patients. Another possibility for the observed decrease in PKC activity may be the increased phosphorylation of PKC isozymes. Increased phosphorylation of PKC may decrease the activity of PKC isozymes.
Although we found a significant decrease in PKC activity and some of its specific isozymes in platelets of bipolar patients, we did not observe any changes in either PKC activity or any of the PKC isozymes in membrane or cytosol fractions of platelets from unipolar patients compared with normal controls. We had previously reported an increase in PKC binding sites using 3H-phorbol dibutyrate as the ligand in the cytosol but not in the membrane fraction of platelets from unipolar patients (Pandey et al. 1998). The reason for this discrepancy is not clear, but it could have various explanations; for exampe, some reports suggest that 3H-PDBU Phorbol dibutyrate also binds to receptors other than PKC, including n-chimerin and Unc-13 (Hall et al. 1990; Wilkinson and Hallam 1994). Therefore, it is possible that the increased binding observed by us in the cytosol fraction of platelets of unipolar patients may be due to increased binding to sites other than PKC.
Although we performed these studies on platelets obtained from drug-free patients, the mean drug-free period (9 days) in bipolar patients may not be long enough to completely rule out the effects of previous treatment on the parameters studied. Whereas all the changes observed in these parameters are not likely to be due to previous medication, it is quite possible that part of these effects may be due to residual effects of previous drug treatment.
Also, we had one unipolar patient who was previously treated with fluoxetine, a long-acting antidepressant. This patient did not have sufficient drug-free days to rule out the effects of fluoxetine. Hence, we also analyzed the data excluding this patient. However, exclusion of this patient did not alter the results, that is, unipolar patients were still not significantly different from controls in any of the parameters we studied.
The decrease in PKC isozyme levels may also be related to changes in the activity of the effector PLC. To examine this possibility, we determined PI-PLC activity and the immunoreactivity of PLC isozymes in platelets of bipolar and unipolar patients. We observed a significant decrease in PI-PLC activity in platelets of bipolar patients compared with control subjects. Furthermore, we observed that whereas there was no significant difference in the protein expression of PLC β1 or γ1 isozymes in membrane or cytosol fractions, the protein expression of PLC δ1 was significantly decreased in both membrane and cytosol fractions of platelets from bipolar patients. However, we did not find any significant differences in the PI-PLC activity or levels of PLC β1, PLC γ1, or PLC δ1 in unipolar patients and normal controls.
The reasons for a specific decrease in PLC δ1 and its significance are unclear. There are three main families of PI-PLC; namely, PLC β, PLC γ, and PLC δ. All PLC isozymes recognize PIP2 as a substrate and carry out Ca2+-dependent hydrolysis of inositol lipids; however, these isozymes are differentially regulated and expressed. PLC β is activated by receptors that activate α or β subunits of the heterotrimeric Gq proteins, and PLC γ is activated by receptor and nonreceptor tyrosine kinases. The regulatory mechanisms of the PLC δ isoform family are not well understood (Cockcroft and Thomas 1992); however, one of the mechanisms that cause a decrease in PLC δ1 could be related to altered levels of PIP2. It has been reported that MARCKS inhibits the activity of PLC δ1 by binding with a significant fraction of PIP2 (Wang et al. 2001). Because a change in PIP2 levels has been reported in platelets of bipolar patients (Soares et al. 2000) and because we observed an increase in levels of MARCKS in platelets of bipolar patients, it is possible that alterations in the levels of PIP2, probably caused by binding of MARCKS, may result in decreased PI-PLC activity and PLC δ1 levels. This possibility needs to be further explored.
Another issue is the significance and/or consequence of altered PKC in bipolar illness. Although PKC is involved in many physiological processes, the mechanisms by which PKC produces these effects are unclear. It has been suggested that a possible mechanism may be the action of PKC on one of its main substrates, MARCKS. That alterations of MARCKS may be involved in bipolar illness is derived from the observation that lithium causes decreased MARCKS expression in immortalized hippocampal cells and rat hippocampus (Watson et al. 1994, Watson and Lenox 1996, Wang et al. 2001). To our knowledge, MARCKS has not been studied in patients with bipolar or unipolar illness. We observed a higher expression of MARCKS in both membrane and cytosol fractions of platelets from bipolar but not unipolar patients, suggesting that bipolar illness may be associated with increased MARCKS expression. Whether this increase is a consequence of the illness or secondary to other changes due to the illness, such as alterations in PKC isozymes, is not known. For example, changes in various receptors, such as muscarinic receptors, may cause alterations in MARCKS, because it has been reported that the activation of muscarinic receptors potentiates the downregulation of MARCKS in the presence of lithium (Watson and Lenox 1996). Therefore, alterations in any of these receptors, such as M1, M2, or 5HT2A, which are linked to PI signaling cascade, may cause changes in MARCKS.
It has also been shown that activation of PKC by phorbol esters in hippocampal cells causes the downregulation of MARCKS (Watson et al., 1994). Because we have observed a decrease in PKC in bipolar disorders, it is attractive to speculate that the decrease in PKC in platelets of bipolar patients may cause a compensatory increase in the expression of MARCKS. In this respect, it is important to note that we observed a reduction in PKC α and PKC β isoforms but not in other isoforms in platelets of bipolar patients. Chen et al. (1996) observed that MARCKS is a more favored substrate compared with neuromodulin and neurogranin for phosphorylation by PKC α than PKC β or PKC δ, thus supporting our hypothesis that the upregulation of MARCKS in bipolar patients may be related to a decrease in PKC α and β.
Recent studies have demonstrated that MARCKS and a peptide corresponding to its basic effector domain (151–175) inhibit PI-specific PLC-catalyzed hydrolysis of PIP2 in vesicles (Glaser et al. 1996), and it is also reported that the addition of 10–100 nM MARCKS (151–175) to a subphase containing either PLC δ1 and β1 inhibits hydrolysis of PIP2 (Wang et al. 2001). In the present study, we found that MARCKS levels are increased in bipolar patients, and hence this increase may cause decreases in hydrolysis of PIP2 by inhibiting PI-PLC activity, because MARCKS interacts with PIP2 substrate and inhibits the PLC-catalyzed hydrolysis of PIP2 and the expression of PLC δ1 (Wang et al. 2001).
Regardless of the mechanism that may be responsible for alterations in MARCKS in platelets of bipolar patients and its possible consequences, our study provides direct evidence that MARCKS is increased in platelets of bipolar patients and thus supports previous suggestions that MARCKS may be altered in bipolar illness, even though this suggestion was primarily based on changes caused in MARCKS by lithium treatment. In this study, we did not observe any differences in PKC or PI-PLC activity or in any of the PKC or PLC isozymes in unipolar patients and normal controls. Previous studies have shown abnormalities in overall PI signaling, G-protein levels, and G-protein coupling to receptors in platelets of depressed patients (Karege et al. 1998; Gurguis et al. 1999) and postmortem brain of depressed suicide victims (Pacheco et al. 1996; Mathews et al. 1997). Our study indicates that the abnormal PI signaling in unipolar patients is not related to downstream events, such as PI-PLC, PKC, or MARCKS, but may be related to alterations in G-proteins. On the other hand, our study demonstrates that abnormalities of PKC and MARCKS are specific to bipolar illness.
In summary, our study suggests abnormalities in PKC and PLC activity as well as in the protein expression of specific PKC and PLC isozymes in platelets of drug-free bipolar patients. Because PKC has been postulated to be crucial in the pathophysiology of bipolar disorders and a target for the therapeutic action of lithium, these results may be important in further understanding of the neurobiology of this illness.
References
Aderem A . (1992): The MARCKS brothers: A family of protein kinase C substrates. Cell 71: 713–716
Aderem A . (1995): The MARCKS family of protein kinase-C substrates. Biochem Soc Trans 23: 587–591
Allen LH, Aderem A . (1995): A role for MARCKS, the alpha isozyme of protein kinase C and myosin I in zymosan phagocytosis by macrophages. J Exp Med 182: 829–840
Altman EG, Hedeker DR, Janicak PG, Peterson JL, Davis JM . (1994): The clinician-administered rating scale for mania (CARS-M): Development, reliability, and validity. Biol Psychiatry 36: 124–134
Baldassare JJ, Henderson PA, Burns D, Loomis C, Fisher GJ . (1992): Translocation of protein kinase C isozymes in thrombin-stimulated human platelets. Correlation with 1,2-diacylglycerol levels. J Biol Chem 267: 15585–15590
Berridge MJ, Irvine RF . (1989): Inositol phosphatase and cell signaling. Nature 341: 197–205
Blackshear PJ . (1993): The MARCKS family of cellular protein kinase C substrates. J Biol Chem 268: 1501–1504
Brown AS, Mallinger AG, Renbaum LC . (1993): Elevated platelet membrane phosphatidyl inositol 4–5 bisphosphate in bipolar mania. Am J Psychiatry 150: 1252–1254
Chen J, Chang S, Duncan SA, Okano HJ, Fishell G, Aderem A . (1996): Disruption of the MacMARCKS gene prevents cranial neural tube closure and results in anencephaly. Proc Natl Acad Sci USA 93: 6275–6279
Cockcroft S, Thomas GMH . (1992): Inositol-lipid-specific phospholipase C isoenzymes and their differential regulation by receptors. Biochem J 288: 1–14
Dwivedi Y, Pandey GN . (1999a): Administration of dexamethasone up-regulates protein kinase C activity and the expression of gamma and epsilon protein kinase C isozymes in the rat brain. J Neurochem 72: 380–387
Dwivedi Y, Pandey GN . (1999b): Repeated administration of dexamethasone increases phosphoinositide-specific phospholipase C activity and mRNA and protein expression of the phospholipase C beta 1 isozyme in rat brain. J Neurochem 73: 780–790
Friedman E, Hoau Yan-Wang, Levinson D, Connell TA, Singh H . (1993): Altered platelet protein kinase C activity in bipolar affective disorder, manic episode. Biol Psychiatry 33: 520–525
Garcia-Sevilla JA, Walzer C, Busquets X, Escriba PV, Balant L, Guimon J . (1997): Density of guanine nucleotide-binding proteins in platelets of patients with major depression: Increased abundance of the G alpha i2 subunit and down-regulation by antidepressant drug treatment. Biol Psychiatry 42: 704–712
Glaser M, Wanaski S, Buser CA, Boguslavsky V, Rashidzada W, Morris A, Rebecchi M, Scarlata SF, Runnels LW, Prestwich GD, Chen J, Aderem A, Ahn J, McLaughlin S . (1996): Myristoylated alanine-rich C kinase substrate (MARCKS) produces reversible inhibition of phospholipase C by sequestering phosphatidylinositol 4,5-bisphosphate in lateral domains. J Biol Chem 271: 26187–26193
Goodall AR, Turner NA, Walker JH, Ball SG, Vaughan PF . (1997): Activation of protein kinase C-alpha and translocation of the myristoylated alanine-rich C-kinase substrate correlate with phorbol ester-enhanced noradrenaline release from SH-SY5Y human neuroblastoma cells. J Neurochem 68: 392–401
Grabarek J, Raychowdhury M, Ravid K, Kent KC, Newman PJ, Ware JA . (1992): Identification and functional characterization of protein kinase C isozymes in platelets and HEL cells. J Biol Chem 267: 10011–10017
Gurguis GN, Vo SP, Griffith JM, Rush AJ . (1999): Platelet alpha-2A-adrenoceptor function in major depression: Gi coupling, effects of imipramine and relationship to treatment outcome. Psychiatry Res 89: 73–95
Hall C, Monfries C, Smith P, Lim HH, Kozma R, Ahmed S, Vanniasingham V, Leung T, Lim L . (1990): Novel human brain cDNA encoding a 24,000 Mr protein n-chimaerin, related to both the regulatory domain of protein kinase C and BCR, the product of the breakpoint cluster region gene. J Mol Biol 211: 11–16
Ikonomov OC, Manji HK . (1999): Molecular mechanisms underlying mood stabilization in manic-depressive illness: The phenotype challenge. Am J Psychiatry 156: 1506–1514
Jope RS . (1999): Anti-bipolar therapy: Mechanism of action of lithium. Mol Psychiatry 4: 117–128
Jope RS, Song L, Li PP, Young LT, Kish SJ, Pacheco MA, Warsh JJ . (1996): The phosphoinositide signal transduction system is impaired in bipolar affective disorder brain. J Neurochem 66: 2402–2409
Karege F, Bovier P, Rudolph W, Gaillard JM . (1996): Platelet phosphoinositide signaling system: An overstimulated pathway in depression. Biol Psychiatry 39: 697–702
Karege F, Bovier P, Stepanin R, Malafosse A . (1998): The effect of clinical outcome on platelet G proteins of major depressed patients. Eur Neuropsychopharmacol 8: 89–94
Kishimoto A, Mikawa K, Hashimoto K, Yasuda I, Tanaka S, Tominaga M, Kuroda T, Nishizuka Y . (1989): Limited proteolysis of protein kinase C subspecies by calcium-dependent neutral protease (calpain). J Biol Chem 264: 4088–4092
Lenox RH, Manji KK . (1998): Lithium. In Schatzberg AF, Nemeroff CB (eds), American Psychiatric Press Textbook of Psychopharmacology, 2nd ed. Washington, DC, American Psychiatric Press, pp 379–429
Lenox RH, Watson DG, Patel J, Ellis J . (1992): Chronic lithium administration alters a prominent PKC substrate in rat hippocampus. Brain Res 570: 333–340
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ . (1951): Protein measurement with the folin phenol reagent. J Biol Chem 193: 265–275
Manji HK, Lenox RH . (1999): Protein kinase C signaling in the brain: Molecular transduction of mood stabilization in the treatment of manic depressive illness. Biol Psychiatry 46: 1328–1351
Manji HK, Etcheberrigaray R, Chen G, Olds JL . (1993): Lithium decreases membrane-associated protein kinase C in hippocampus: Selectivity for the α isozyme. J Neurochem 61: 2302–2310
Manji HK, Potter WZ, Lenox RH . (1995): Signal transduction pathways: Molecular targets for lithium's action. Arch Gen Psychiatry 52: 531–543
Mathews R, Li PP, Young LT, Kish SJ . (1997): Increased Gαq/11 immunoreactivity in postmortem occipital cortex from platelets with bipolar affective disorder. Biol Psychiatry 41: 649–656
McLaughlin S, Aderem A . (1995): The myristoyl-electrostatic switch: A modulator of reversible protein-membrane interactions. Trends Biochem Sci 20: 272–276
McNamara RK, Hyde TM, Kleinman JE, Lenox RH . (1999): Expression of the myristoylated alanine-rich C kinase substrate (MARCKS) and MARCKS-related protein (MRP) in the prefrontal cortex and hippocampus of suicide victims. J Clin Psychiatry 60 (Suppl 2): 21–26
Mikuni M, Kusumi I, Kagaya A, Kuroda Y, Mori H, Takahashi K . (1991): Increased 5-HT2 receptor function as measured by serotonin stimulated phosphoinositide hydrolysis in platelets of depressed patients. Prog Neuropsychopharmacol Biol Psychiatry 15: 49–61
Myat MM, Anderson S, Allen LA, Aderem A . (1997): MARCKS regulates membrane ruffling and cell spreading. Curr Biol 7: 611–614
Nishizuka Y . (1992): Intracellular signaling by hydrolysis of phospholipids and activation of protein kinase C. Science 258: 607–613
Pacheco MA, Stockmeier C, Meltzer HY, Overholser JC, Dilley GE, Jope RS . (1996): Alterations in phosphoinositide signaling and G-protein levels in depressed suicide brain. Brain Res 723: 37–45
Pandey GN, Pandey SC, Davis JM . (1990): Peripheral adrenergic receptors in affective illness and schizophrenia. Pharmacol Toxicol 66 (Suppl 3): 13–36
Pandey GN, Pandey SC, Dwivedi Y, Sharma RP, Janicak PG, Davis JM . (1995): Platelet serotonin-2A receptors: A potential biological marker for suicidal behavior. Am J Psychiatry 152: 850–855
Pandey GN, Dwivedi Y, Kumari R, Janicak PG . (1998): Protein kinase C in platelets of depressed patients. Biol. Psychiatry 44: 909–911
Pandey GN, Dwivedi Y, Pandey SC, Teas SS, Conley RR, Roberts RC, Tamminga CA . (1999): Low phosphoinositide-specific phospholipase C activity and expression of phospholipase C beta1 protein in the prefrontal cortex of teenage suicide subjects. Am J Psychiatry 156: 1895–1901
Soares JC, Mallinger AG . (1996): Abnormal phosphatidylinositol (PI)-signaling in bipolar disorder. Biol Psychiatry 39: 461–464
Soares JC, Barwell M, Mallinger AG, Kupfer DJ, Frank E . (1999): Adjunctive antipsychotic use in bipolar patients: an open 6-month prospective study following an acute episode. J Affect Disord 56: 1–8
Soares JC, Chen G, Dippold CS, Wells KF, Frank E, Kuppfer DJ, Manji HK, Mallinger AG . (2000): Concurrent measures of protein kinase C and phosphoinositide in lithium treated bipolar patients and healthy individuals: A preliminary study. Psychiatry Res 95: 109–118
Wang HY, Markowitz P, Levinson D, Undie AS, Friedman E . (1999): Increased membrane-associated protein kinase C activity and translocation in blood platelets. J Psychiatr Res 33: 171–179
Wang J, Arbuzova A, Hangyas-Mihalyne G, McLaughlin S . (2001): The effector domain of myristoylated alanine-rich C kinase substrate (MARCKS) binds strongly to phosphatidylinositol 4,5-bisphosphate (PIP2). J Biol Chem 276: 5012–5019
Wang L, Watson DG, Lenox RH . (2000): Myristoylation alters retinoic acid-induced down-regulation of MARCKS in immortalized hippocampal cells. Biochem Biophys Res Commun 276: 183–188
Watson DG, Lenox RH . (1996): Chronic lithium-induced down-regulation of MARCKS in immortalized hippocampal cells: Potentiation by muscarinic receptor activation. J Neurochem 67: 767–777
Watson DG, Wainer BH, Lenox RH . (1994): Phorbol ester and retinoic acid-induced regulation of the protein kinase C substrate MARCKS in immortalized hippocampal cells. J Neurochem 63: 1666–1674
Wilkinson SE, Hallam TJ . (1994): Protein kinase C: Is its pivotal role in cellular activation over-stated? Trends Pharmacol Sci 15: 53–57
Yamauchi E, Kiyonami R, Kanai M, Taniguchi H . (1998): The C-terminal conserved domain of MARCKS is phosphorylated in vivo by proline-directed protein kinase. Application of ion trap mass spectrometry to the determination of protein phosphorylation sites. J Biol Chem 273: 4367–4371
Young LT, Wang JF, Woods CM, Robb JC . (1999): Platelet protein kinase C alpha levels in drug-free and lithium-treated subjects with bipolar disorder. Neuropsychobiology 40: 63–66
Acknowledgements
The technical assistance of Barbara Brown and Miljana Petkovic and the help of Jim Peterson in diagnosing patients and blood collection are gratefully acknowledged. This work was supported by a grant from the National Institute of Mental Health (RO1-MH-56528 to GNP) and in part by a General Clinical Research Center Program Project from National Institute of Health (MO1RR13987 to Dr. G. Moss).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pandey, G., Dwivedi, Y., SridharaRao, J. et al. Protein Kinase C and Phospholipase C Activity and Expression of Their Specific Isozymes Is Decreased and Expression of MARCKS Is Increased in Platelets of Bipolar but Not in Unipolar Patients. Neuropsychopharmacol 26, 216–228 (2002). https://doi.org/10.1016/S0893-133X(01)00327-X
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1016/S0893-133X(01)00327-X
Keywords
This article is cited by
-
The neurobiology of suicide - A Review of post-mortem studies
Journal of Molecular Psychiatry (2013)
-
A Role for the PKC Signaling System in the Pathophysiology and Treatment of Mood Disorders: Involvement of a Functional Imbalance?
Molecular Neurobiology (2011)
-
Evidence for rare and common genetic risk variants for schizophrenia at protein kinase C, alpha
Molecular Psychiatry (2010)
-
Gene expression and association analyses of LIM (PDLIM5) in bipolar disorder and schizophrenia
Molecular Psychiatry (2005)
-
Decreased Serotonin 5-HT2A Receptor-Stimulated Phosphoinositide Signaling in Fibroblasts from Melancholic Depressed Patients
Neuropsychopharmacology (2004)