Abstract
In several reports, the acute oral administration of the partial serotonergic agonist meta-chlorophenylpiperazine (mCPP) in dose of 0.5 mg/kg induced a significant worsening of obsessive-compulsive (OC) symptoms in a number of patients. The aim of our study was to test the 0.25 mg/kg mCPP dose, which was hypothesized to be more specific for OC symptoms and was until now tested only on healthy subjects. In a double-blind, controlled crossover study, 12 OC patients participated on three test days, receiving one of the following on each day: oral 0.5 mg/kg mCPP (standard dose), 0.25 mg/kg mCPP (low dose), or placebo. Behavioral ratings were obtained by means of Visual Analogue Scale (VAS) ratings. The low dose mCPP induced a significant worsening of OC symptoms in 50% (6/12) of the patients, whereas 8.3% (1/12) of the patients showed a worsening after the standard dose. On the other hand, only the standard dose mCPP induced a worsening, although not statistically significant, of anxiety ratings. Our data show that the 0.25 mg/kg dose mCPP induces a specific response in OC symptoms, with little anxiogenic effect. To confirm these preliminary data, future studies will be needed on larger samples and with more sensitive rating scales.
Similar content being viewed by others
Main
Meta-chlorophenylpiperazine (mCPP), the main metabolite of the antidepressant trazodone (Caccia et al. 1981), has various 5-HT agonist properties that have recently been used to assess central 5-HT receptor sensitivity in psychiatric disorders (Charney et al. 1987; Zohar et al. 1987; Hollander et al. 1992; Goodman et al. 1995; Hott Pian et al. 1998; Broocks et al. 1998).
mCPP has complex effects on brain 5-HT systems: it binds potently to 5-HT2c receptors and, with weaker affinity, to 5-HT1a receptors (Kahn and Wetzler 1991). Animal models of anxiety (i.e., social interaction, dark/light box) suggest that mCPP anxiogenic effects are mediated through agonist action on 5-HT2c (ex 5-HT1c) receptors (Curzon and Kennett 1990).
Several studies have evaluated behavioral responses to mCPP in obsessive compulsive (OC) patients. In three double blind, placebo controlled studies (Zohar et al. 1987; Pigott et al. 1991; Hollander et al. 1992), oral mCPP administration in dose of 0.5 mg/kg induced a significant worsening of obsessive-compulsive symptoms in a number of patients. These results have been interpreted as a possible evidence of a serotonergic postsynaptic hypersensitivity in OC patients. On the other hand, in more recent studies (Goodman et al. 1995; Hott Pian et al. 1998), oral mCPP administration (0.5 mg/kg) did not show any evidence of OC symptoms exacerbation in drug-free patients with obsessive compulsive disorder (OCD).
The choice of the standard mCPP dose (0.5 mg/kg) was done according to the hypothesis of an hyposensitivity of 5-HT receptors related to the hypothalamus-pituitary-adrenal (HPA) axis in OCD (Pigott et al. 1991), suggesting that 5-HT receptor stimulation should be large enough to detect a blunted hormone response in comparison to control subjects. However, if serotonergic hypersensitivity is suspected in OCD, then 5-HT receptor stimulation should be low enough to avoid a ceiling effect (Kahn et al. 1990) of the behavioral responses (i.e., higher anxiety levels might mask underlying OC symptoms).
We designed the present study to evaluate behavioral responses of OC patients to different oral doses of mCPP: a standard dose (0.5 mg/kg) to replicate results from literature, and a low dose (0.25 mg/kg), according to the hypothesis of a serotonergic hypersensitivity, to test a possible major specificity of the low-dose challenge for OCD.
METHODS
Subjects
Twelve patients (eight men and four women, mean age 27.7 ± 9.9 years) participated in the study. After complete description of the study, carried out in accordance with the Declaration of Helsinki, both oral and written informed consents were obtained from all subjects before their enrolment.
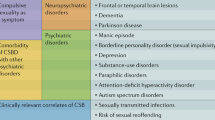
The investigation included all consenting and eligible patients who were admitted to the Department of Neuropsychiatric Sciences at S. Raffaele Hospital, University of Milan. These patients met DSM-IV criteria (American Psychiatric Association 1994) for OCD and were drug-free for at least five weeks. Inclusion criteria consisted of: age from 18 to 60 years, DSM-IV diagnosis of OCD, absence of other lifetime and/or current coexisting Axis I diagnoses. Exclusion criteria consisted of: renal, hepatic, and/or thyroid abnormalities indicated by anamnesis and routine analyses, as well as other serious general medical conditions.
Clinical Assessment
On admission, all patients received a DSM-IV clinical diagnosis of OCD. Therefore, to confirm diagnosis of OCD and to exclude coexisting Axis I diagnoses, the Italian version of the Diagnostic Interview Schedule-Revised (DIS-R) (Robins et al. 1989) was routinely administered by a resident in psychiatry (M.H.), trained and experienced in the use of the instrument. The data collected were scored by a computer program (Marcus et al. 1990) and then modified according to DSM-IV criteria where appropriate.
To quantify baseline OCD symptom severity, we used the Yale Brown Obsessive Compulsive Scale (Y-BOCS) (Goodman et al. 1989a,b), which is sensitive to severity of OCD symptoms. To quantify baseline depressive symptoms, the 21-item Hamilton Depression Rating Scale (HDRS) (Hamilton 1960) was used.
Visual Analogue Scale (VAS) ratings completed by patients were used to evaluate changes in subjective condition using four different items: sad (VAS-SAD), anxious (VAS-ANX), drowsy (VAS-DRO), and disturbed by obsessions and compulsions (VAS-OC). All VAS ratings were scored in millimetres from the left-hand site of a 100-mm line to a perpendicular mark made by subjects at a point corresponding to their state at that time. The score ranged from 0 (“not at all”) to 100 (“most ever”).
Procedure
Each patient participated at three test days, in which they received oral 0.5 mg/kg mCPP (“standard”), 0.25 mg/kg (“low”), or placebo, in a double-blind, controlled, balanced crossover fashion (minimum interval between challenges: 3 days). The mCPP was obtained from Aldrich Chemical Co., Milwaukee, WI.
Patients fasted from 11 p.m. on the night before the day of the procedure. At 8:30 a.m. (t0), after a 30-min adaptation period, vital signs (blood pressure, heart rate, sublingual temperature) and VAS clinical ratings were collected, and subjects received either mCPP or placebo identical capsules. Vital signs and VAS ratings were also collected at 1 (t1), 2 (t2), 3 (t3), and 4 (t4) hours after the ingestion of the capsule. During the experimental procedure patients were not allowed to sleep, eat, or drink (except for water).
Data Analysis
Results from behavioral ratings were analyzed by means of analysis of variance (ANOVA) with repeated measures (Wilkinson et al. 1992). The main effects considered were treatment (“standard” mCPP vs. “low” mCPP vs. placebo) and time (changes over the five time points sampled: t0, t1, t2, t3, t4). The interaction of treatment × time was also considered.
When significant treatment × time interactions were identified, post-hoc paired t-tests were performed to detect between-treatment differences (Wilkinson et al. 1992). The “peak response” to mCPP for each variable was calculated as previously described (Zohar et al. 1988; Goodman et al. 1995) by subtracting the maximum change following placebo or mCPP administration from the corresponding baseline measure. Paired t-tests were then used to compare the between-treatment peak responses to mCPP.
As for obsessive-compulsive symptoms, according to the “peak response” calculation, patients were classified as “worsened” (WOR) and “unchanged” (UNC). If the peak increase of the VAS-OC from baseline was ⩾ 12, corresponding to the ⩾ 1-point increase with the Clinician-Rated Obsessive Compulsive Challenge Scale (Goodman and Price 1990), patients were classified as “worsened”. “Unchanged” patients had VAS-OC peak changes from baseline less than 12.
RESULTS
Characteristics of the Sample
Demographic and clinical characteristics of the sample are summarized in Table 1 .
Adverse Effects and Vital Signs
On the whole, mCPP was well tolerated: both standard and low dose caused a mild drowsiness in six patients; three patients reported a mild nausea during the administration of the standard dose (0.5 mg/kg). One of these three patients reported also a late-onset headache (i.e., about 4 hours after the end of the challenge), an adverse effect already mentioned in the literature (Zohar et al. 1987). On the other hand, the low mCPP dose (0.25 mg/kg) did not cause any significant adverse effect. Blood pressure, heart rate, and sublingual temperature did not show any significant variation during the three challenges.
Behavioral Effects
Obsessive-Compulsive Symptoms
A repeated measures ANOVA performed on VAS-OC ratings revealed a significant treatment × time interaction (F = 2.95; df = 8,88; p = .006). Figure 1 and Table 2 suggest a worsening of OC symptoms after the low dose of mCPP, not after the standard dose. Post-hoc t-test evaluation showed a significant difference between the placebo and the low dose at time t3 (t = −2.33, df = 11, p = .04); no other significant differences were found, including an analysis with sex as a grouping variable (F = 1.17, df = 4.40, p = .34).
Inspection of Figure 1 suggests a baseline difference in VAS-OC score; however, there were no significant differences in baseline behavioral measures among the three test days, as evidenced by the non-significant main effect of treatment (F = 1.07; df = 2,22; p = .36). The main effect of treatment remained non-significant even when ANOVA was covaried for baseline OC score (F = 0.098; df = 2,16; p = .10)
Peak Responses
Paired t-tests on peak responses in VAS scores for OC symptoms showed a significant difference between the low- and standard-dose mCPP (t = 2.45, df = 11, p = .03)
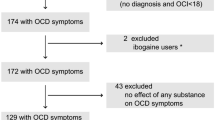
Categorical Approach
Patients were divided in “worsened” and “unchanged” according to the classification mentioned above (see Methods, data analysis). While 50% of patients (6/12) showed a worsening of OC symptoms after the low dose mCPP, only the 8.33% of patients (1/12) showed a worsening after the standard dose. A 2 × 2 chi-square test (low/standard dose × worsened/unchanged) showed a marginally significant difference between the two doses (chi-square = 3.23, df = 1, p = .072).
Anxiety and Mood
A repeated measures ANOVA on VAS-ANX and VAS-SAD ratings did not show any significant treatment × time interaction. Although not significant, Figure 2 and Table 2 suggest an exacerbation of anxiety ratings with the 0.5 mg/kg dose mCPP.
DISCUSSION
The administration of the standard dose (0.5 mg/kg) mCPP did not show any significant effect on OC symptoms, in agreement with the findings of Goodman et al. (1995) and Hott Pian et al. (1998). In comparison with previous reports, our study lacks a healthy control group, but prior studies have not documented obsessogenic responses in normals to mCPP, and our study aims to test the effect of different mCPP doses in patients.
Several factors should be considered in evaluating the absence of response to the standard dose mCPP. The first factor could be the small sample size of this study, leading to the risk of a Type II error. The second could be the environmental condition during the experimental procedure. A study from Khanna (1993) suggests that susceptibility to mCPP is related to both drug and behavioral exposure conditions. For example, the contact with a “contaminated” sphygmomanometer could provoke a behavioral challenge in some patients, interfering with the biological effects of the substance. For such reason, our staff was asked to minimize any behavioral stimulus during the challenge, and patients were questioned about their specific OC symptoms, to minimize non-specific effects of “distress” due to the unusual experimental conditions. Another issue could be the poor sensitivity of the VAS rating scales, which measure only a subjective condition of the distress related to OC symptoms. We are now planning another study employing Clinician-Rated and Patient-Rated Obsessive-Compulsive Challenge Scales (CR-OCCS and PR-OCCS) (Goodman and Price 1990), in order to obtain better comparisons with previous data. Thus, because of the difference between VAS and CR-OCCS, this study is not entirely comparable to previous studies (Hollander et al. 1992; Goodman et al. 1995).
The anxiogenic effect of the standard dose mCPP, even if not statistically significant, is in agreement with the data about the non-specific anxiogenic effect of 0.5 mg/kg (oral) or 0.1 mg/kg (intravenous) mCPP administration in normal controls (Kahn et al. 1990) and in different mental disorders, such as OCD (Goodman et al. 1995) and schizophrenia (Krystal et al. 1993). This apparent discrepancy between the effect of the 0.50 mg/kg dose on anxiety and the 0.25 mg/kg dose on OC symptoms might be attributed to a differential action of different mCPP doses on various receptor subpopulations (Hoyer et al. 1994).
The original aspect of our study is the utilisation of the low-dose mCPP, until now tested only on healthy controls (Kahn et al. 1990). Our data, even though preliminary, show that the low-dose mCPP induces a specific response on OC symptoms, is less anxiogenic and better tolerated than the standard dose. Moreover, the 0.25 mg/kg dose of mCPP points out a possible greater selectivity on some receptor subpopulations. In fact, many 5-HT receptor subpopulations are stimulated, with weak affinity, by mCPP, i.e., 5-HT1A and 5-HT1B as an agonist, and 5-HT1D as an antagonist (Glennon and Dukat 1995). On the other hand, 5-HT2C receptors appear to be stimulated more selectively than other receptors with a lower dose of mCPP (Hoyer et al. 1994). Overall, our data agree with the hypothesis of a hypersensitive serotonergic receptor subpopulation in OCD (Zohar et al. 1987), even though other possibilities, e.g., a deficiency of compensatory mechanisms during 5-HT stimulation, can be considered.
Since the 1960s, serotonin has been repeatedly implicated in the pathophysiology of OCD (Insel et al. 1985; Jenike et al. 1990; Murphy and Pigott 1990; Zohar et al. 1988; Barr et al. 1992). This evidence was largely derived from the data about chronic administration of clomipramine and SSRIs, whose antiobsessive efficacy appears to be critically linked to the effects on the 5-HT system rather than other neurotransmitters (Pigott 1996).
Future studies will be needed to test the serotonin hypothesis of OCD (Barr et al. 1992) on larger samples and with more sensitive and specific rating scales. New drugs, with a more selective serotonergic action, will also be needed to evaluate the possible role of serotonergic receptor subtypes.
References
American Psychiatric Association . (1994): Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC, American Psychiatric Press
Barr LC, Goodman WK, Price LH, McDougle CJ, Charney DS . (1992): The serotonin hypothesis of obsessive compulsive disorder: Implications of pharmacologic challenge studies. J Clin Psychiatry 53(Suppl 4): 17–28
Broocks A, Pigott TA, Hill JL, Canter S, Grady TA, L'Heureux F, Murphy DL . (1998): Acute intravenous administration of ondansetron and mCPP, alone and in combination, in patients with obsessive-compulsive disorder (OCD): Behavioral and biological results. Psychiatry Res 79 (1)): 11–20
Caccia S, Ballabio M, Samanin R, Zanini MG, Garattini S . (1981): mCPP, a central 5-HT agonist, is a metabolite of trazodone. J Pharm Pharmacol 33: 477–478
Charney DS, Woods SW, Goodman WK, Heninger GR . (1987): Serotonin function in anxiety. II. Effects of the serotonin agonist MCPP in panic disorder patients and healthy subjects. Psychopharmacology 92 (1)): 14–24
Curzon G, Kennett GA . (1990): mCPP: A tool for studying behavioral responses associated with 5-HT1c receptors. Trends Pharmacol Sci 11: 181–182
Glennon RA, Dukat M . (1995): Serotonin receptors subtypes. In Bloom FE, Kupfer DJ (eds), Psychopharmacology; The Fourth Generation of Progress. New York, Raven Press, pp 415–429
Goodman WK, McDougle CJ, Price LH, Barr LC, Hills OF, Caplik JF, Charney DS, Heninger GR . (1995): m-chlorophenylpiperazine in patients with obsessive-compulsive disorder: Absence of symptom exacerbation. Biol Psychiatry 38 (3)): 138–149
Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, Heninger GR, Charney DS . (1989a): The Yale-Brown obsessive-compulsive scale. I. Development, use and reliability. Arch Gen Psychiatry 46: 1006–1011
Goodman WK, Price LH, Rasmussen SA, Mazure C, Delgado P, Heninger GR, Charney DS . (1989b): The Yale-Brown obsessive compulsive scale. II. Validity. Arch Gen Psychiatry 46: 1012–1016
Goodman WK, Price LH . (1990): Rating scales for obsessive compulsive disorder. In Jenike MA, Baer L, Minichiello WE (eds), Obsessive Compulsive Disorders: Theory and Management. 2nd ed. Littleton, MA, PSG Publishing Company, pp 154–166
Hamilton M . (1960): A rating scale for depression. J Neurol Neurosurg Psychiatry 23: 56–62
Hollander E, DeCaria CM, Nitescu A, Gully R, Suckow RF, Cooper TB, Gorman JM, Klein DF, Liebowitz MR . (1992): Serotonergic function in obsessive-compulsive disorder: Behavioral and neuroendocrine response to oral m-chlorophenylpiperazine and fenfluramine in patients and healthy volunteers. Arch Gen Psychiatry 49: 21–28
Hott Pian KL, Westenberg HG, den Boer JA, de Bruin WI, van Rijk PP . (1998): Effects of meta-chlorophenylpiperazine on cerebral blood flow in obsessive-compulsive disorder and controls. Biol Psychiatry 44 (5)): 367–370
Hoyer D, Clarke DE, Fozard JR, Hartig PR, Martin GR, Mylecharane EJ, Saxena PR, Humphrey PPA . (1994): International union of pharmacology classification of receptors for 5-hydroxitryptamine (serotonin). Pharmacological reviews. Am Soc Pharmacol Exp Therap 46 (2)): 157–193
Insel TR, Mueller EA, Alterman I, Linnoila M, Murphy DL . (1985): Obsessive compulsive disorder and serotonin: Is there a connection? Biol Psychiatry 20 (11)): 1174–1188
Jenike MA, Hyman S, Baer L, Holland A, Minichiello WE, Buttolph L, Summergrad P, Seymour R, Ricciardi J . (1990): A controlled trial of fluvoxamine in obsessive compulsive disorder: Implications for a serotoninergic theory. Am J Psychiatry 147 (9)): 1209–1215
Kahn RS, Wetzler S . (1991): m-chlorophenylpiperazine as a probe of serotonin function. Biol Psychiatry 30: 1139–1166
Kahn RS, Wetzler S, Asnis GM, Kling MA, Suckow RF, van Praag HM . (1990): Effects of m-chlorophenylpiperazine in normal subjects: A dose-response study. Psychopharmacology 100: 339–344
Khanna S . (1993): Serotonergic Challenges in Obsessive Compulsive Disorder. First International Obsessive Compulsive Disorder Conference. Capri, Italy; March 12–13.
Krystal JH, Seibyl JP, Price LH, Woods SW, Heninger GR, Aghajanian GK, Charney DS . (1993): m-chlorophenylpiperazine effects in neuroleptic-free schizophrenic patients. Evidence implicating serotonergic systems in the positive symptoms of schizophrenia. Arch Gen Psychiatry 50 (8)): 624–635
Marcus S, Buke S, McEvoy L, Zeena T, Robins L . (1990): NIMH Diagnostic Interview Schedule. Data Entry and Verification. Version 1.0. St. Louis, Washington University School of Medicine
Murphy DL, Pigott TA . (1990): A comparative examination of a role for serotonin in obsessive compulsive disorder, panic disorder and anxiety. J Clin Psychiatry 51(Suppl 4): 53–58
Pigott TA . (1996): OCD: Where the serotonin selectivity story begins. J Clin Psychiatry 57(Suppl 6): 11–20
Pigott TA, Zohar J, Hill JL, Bernstein SE, Grover GN, Zohar-Kadouch RC, Murphy DL . (1991): Metergoline blocks the behavioral and neuroendocrine effects of orally administered m-chlorophenylpiperazine in patients with obsessive-compulsive disorder. Biol Psychiatry 29: 418–426
Robins LD, Helzer TE, Cottler L . (1989): NIMH Diagnostic Interview Schedule. Version III-R (DIS III-R). St Louis, Washington University School of Medicine
Wilkinson L, Hill MA, Vang E . (1992): SYSTAT: Statistics. Version 5.2. Evanston, IL, SYSTAT, Inc
Zohar J, Mueller A, Insel TR, Zohar-Kadouch RC, Murphy DL . (1987): Serotonergic responsivity in obsessive-compulsive disorder. Comparison of patients and healthy controls. Arch Gen Psychiatry 44: 946–951
Zohar J, Insel TR, Zohar-Kadouch RC, Hill JL, Murphy DL . (1988): Serotonergic responsivity in obsessive-compulsive disorder. Effects of chronic clomipramine treatment. Arch Gen Psychiatry 45: 167–172
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Erzegovesi, S., Martucci, L., Henin, M. et al. Low versus Standard Dose mCPP Challenge in Obsessive-Compulsive Patients. Neuropsychopharmacol 24, 31–36 (2001). https://doi.org/10.1016/S0893-133X(00)00178-0
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1016/S0893-133X(00)00178-0