Abstract
The effects on cataplexy and daytime sleep of acute and chronic oral administration of CG-3703, a potent TRH analog were assessed in canine narcolepsy. CG-3703 was found to be orally active and to reduce cataplexy (0.25 to 16 mg/kg) and sleep (8 and 16 mg/kg) in a dose-dependent manner. Two-week oral administration of CG-3703 (16 mg/kg) significantly reduced cataplexy and daytime sleep. The anticataplectic effects of CG-3703 were not associated with changes in general behavior, heart rate, blood pressure, rectal temperature, blood chemistry and thyroid function. Although drug tolerance for the effects on cataplexy and sleep were observed during the second week of chronic drug administration, therapeutic efficacy on cataplexy was improved with individual dose adjustment (final dose range: 16 to 28 mg/kg, p.o.). These results suggest that TRH analogs could be a promising new form of treatment for human narcolepsy.
Similar content being viewed by others
Main
Human narcolepsy is a chronic life-long disorder characterized by excessive daytime somnolence (EDS), abnormal manifestations of rapid eye movement (REM) sleep (hypnagogic hallucinations and sleep paralysis), and cataplexy (Aldrich 1992; Guilleminault 1994; Nishino and Mignot 1997). Cataplexy is a sudden loss of muscle tone in response to emotionally-exciting stimuli. It is akin to the muscle atonia that occurs during physiological REM sleep, but it occurs inappropriately during wakefulness (Aldrich 1992; Guilleminault 1994; Nishino and Mignot 1997). The current treatments for narcolepsy require the use of central nervous system (CNS) stimulants for EDS and antidepressants for cataplexy and abnormal REM sleep (Guilleminault 1994; Mitler et al. 1990; Thorpy and Goswami 1990). These treatments, however, are often unsatisfactory due to incomplete therapeutic efficacy, the occurrence of various side effects, and the rapid development of drug tolerance (Guilleminault 1994; Mitler et al. 1990; Thorpy and Goswami 1990). It is therefore necessary to explore more efficacious compounds with different pharmacological profiles for possible use in narcolepsy treatment.
Canine narcolepsy is a naturally-occurring animal model of the human disorder. Like humans, narcoleptic canines exhibit short sleep latency, fragmented sleep patterns, and cataplexy (Kaitin et al. 1986; Nishino and Mignot 1997; Nishino et al. 1998c; Riehl et al. 1998). Narcolepsy in Doberman pinschers and Labrador retrievers is caused by mutations in the gene encoding a receptor (Hcrtr-2) for a novel neuropeptide, the hypocretins (orexins) (Lin et al. 1999). Human and canine narcolepsy share similar pharmacological characteristics (see Nishino and Mignot (1997) for a review). This model is thus an invaluable resource for the study of the pathophysiology and treatment of narcolepsy. To this end, the canine model has been used in numerous pharmacological experiments to dissect the mode of action of various compounds on their effects on wakefulness and cataplexy, and to screen new compounds for use as possible treatments for narcolepsy (see Nishino and Mignot (1997) for a review).
Thyrotropin releasing hormone (TRH) is a tripeptidic hormone (L-pyroglutamyl-L-histidyl-L-prolineamide) originally extracted from the hypothalamus (Boler et al. 1969). It is now known to be distributed widely in the CNS, with receptors reported to exist in structures such as the pituitary, cortex, brainstem, thalamus, hippocampus, amygdala, and spinal cord (see Griffiths and Bennett 1987; Jackson 1982; Metcalf 1982; Sharif 1985; and Winokur et al. 1989 for reviews). Besides its role in stimulating the release of thyroid stimulating hormone (TSH) and prolactin (see Kolesnick and Gershengorn 1985 for a review), TRH has been shown to have various neuromodulating effects that are separate from its hormonal effects; it is known to have CNS stimulant and antidepressant effects, depolarize spinal motoneurons, and have various neurotrophic effects (see Griffiths and Bennett 1987; Jackson 1982; Metcalf 1982; Sharif 1985; and Winokur et al. 1989 for reviews). Because of its CNS stimulant and antidepressant effects, TRH may be an attractive compound to study for possible use as treatment for narcolepsy. However, the clinical application of TRH is greatly limited because it has a short biological half-life (4 to 5 minutes) and limited access to the CNS (see Metcalf 1982 for a review). Therefore, more biologically-stable TRH analogs have been developed for possible clinical application (see Flohé et al. 1983).
We have previously investigated the effects of intravenous administration of various TRH analogs (CG-3703, CG-3509, and TA-0910) on the sleep/wake pattern and on cataplexy in canine narcolepsy and found that the TRH analogs potently increased wake, decreased sleep, and suppressed cataplexy (Nishino et al. 1997). Because narcolepsy is a chronic disorder requiring chronic treatment, and because oral is the preferred route of administration for chronic drug administration in humans, we assessed the effects of acute and 2-week chronic oral administration of CG-3703, one of the most potent TRH analogs, on the sleep/wake patterns and cataplexy of genetically-narcoleptic Dobermans.
MATERIALS AND METHODS
Animals
Six adult narcoleptic Doberman pinschers were used to assess the effects of CG-3703 on cataplexy (2 males, 4 females; mean age ± SD, 2.30 ± 2.07 y). Three narcoleptic (2 males, 1 female; 3.36 ± 2.15 y) and one control (male; 1.82y) Dobermans with surgically-implanted electroencephalogram (EEG), electrooculogram (EOG) and electromyogram (EMG) electrodes were used for the acute administration polygraphic studies. Two surgically-implanted narcoleptic Dobermans (2 males; 3.05 ± 1.17 y) were used for the chronic administration polygraphic studies.
All animals were housed in individual cages (1.0m × 1.8m) at the Stanford Department of Comparative Medicine Research Animal Facility, where temperature (22–24°C), humidity (40%), and the light:dark cycle (12 hours:12 hours) were maintained at constant conditions. All experiments were carried out in strict accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals.
Cataplexy Testing
The effect of CG-3703 (Grünenthal GmBH, Stolberg, Germany) on cataplexy was assessed in each dog using the Food Elicited Cataplexy Test (FECT) (Baker and Dement 1985; Nishino and Mignot 1997; Riehl et al. 1998). In this assay, 12 scoops of canned dog food (1 cm3) are arrayed in sequence on the floor. As food is a potent inducer of cataplexy in narcoleptic dogs, the animal's attempt to eat all the food will typically be interrupted by several cataplectic attacks. The experimenter notes the number and duration of cataplectic attacks that occur while the dog eats all the food. The sum of the duration of each cataplectic episode per FECT (time spent in cataplexy, TSC) is calculated and, along with the number of cataplectic attacks (NA), is used as an index of cataplexy severity.
In the dose-response study, after baseline FECTs, a starting dose of 0.25 mg/kg CG-3703 (mixed with canned dog food) was given orally to each of the animals. The FECT was performed two hours later, followed by administration of a dose of CG-3703 that was 4 times higher than the previous. This procedure was repeated until complete suppression of cataplexy was observed in most animals.
In the time course study, after baseline FECTs, CG-3703 (16 mg/kg) was orally administered to each of the animals. FECTs were then performed at 0.5, 1, 2, 4, 6, 12, and 24 hours after drug administration.
To determine the effects of chronic administration of CG-3703, 16 mg/kg of the drug was administered orally at 9 A.M. daily for 14 consecutive days. FECTs were then performed at 1 P.M. (i.e., four hours after drug administration) every two days, as well as after termination of drug treatment to monitor any withdrawal effects. Heart rate (HR), blood pressure (BP), rectal temperature (RT), and general behavior were monitored following each FECT session. Body weight was monitored once a week.
Polygraphic Recordings
The effects of acute administration of 8 mg/kg and 16 mg/kg CG-3703 on sleep and wakefulness using 6-hour daytime polygraphic recordings were assessed on three implanted narcoleptic animals. For comparison, the effects of CG-3703 on sleep and wakefulness were assessed in one implanted control animal. A detailed description of the surgical procedure for implanting electrodes has previously been described (Nishino et al. 1995). Briefly, after pretreatment with atropine (0.04 mg/kg, s.c.), anesthesia was induced using a mixture of ketamine and diazepam (10 mg/kg and 0.5 mg/kg, i.v.) and maintained using isoflurane inhalant (end-expired isoflurane, 1.8 to 2.1% mixture in air). The animal was placed in a Kopf stereotaxic device, and the skull was exposed. Screw electrodes were implanted in the skull over the right lateral parietal and mid-frontal cortices for recording of the EEG, and in the orbit of the frontal bone for the EOG. Stranded stainless steel wires were inserted into the dorsal neck muscles for the EMG. The animals were allowed at least three weeks to recover from surgery prior to being used for any experiments.
Recordings were performed at least two days apart, beginning immediately after consumption of the food and drug mixture (9 A.M.). A total of six recordings were performed on each animal: two baseline recordings, two low dose recordings (8 mg/kg for narcoleptics and 4 mg/kg for the control animal), and two high dose recordings (16 mg/kg for narcoleptics and 8 mg/kg for the control animal). Each recording session in each series (baseline, low dose, and high dose) was randomized.
To determine the effect of chronic administration of CG-3703 on the vigilance states, the drug (16 mg/kg, p.o.) was administered at 9 A.M. daily for two weeks. Polygraphic recordings (9 A.M. to 3 P.M.) were carried out on days −4, −3, 3, 4, 10, and 11 of drug administration.
All recordings were manually scored in 30-second epochs according to Nishino et al. (Nishino et al. 1995). Briefly, an epoch was scored as wake when the EEG tracings consisted of low-voltage, mixed-frequency waves and the EMG was not inhibited. During this stage, the animals walked, sat, or lay down, and eyes were open. Drowsy was scored when the EEG showed a background of low-voltage, mixed-frequency waves with trains of theta waves (5–7 Hz). During this stage, the animals were usually lying down in prone position with eyes closed. Light sleep was scored when the EEG showed spindles (12–14 Hz) or consisted of less than 20% delta waves (0.5 to 4 Hz) on a background of medium-voltage, mixed frequency waves. Deep sleep was scored when the EEG consisted of a significant amount (>20%) of delta waves. During this stage, the animals lay in prone position or on their side and eyes were closed. Rapid eye movement (REM) sleep was scored when the EEG consisted of low-voltage, mixed-frequency waves with an accompanying decrease in EMG tone. Rapid eye movements were also often observed during this stage. In narcoleptic animals, an additional stage of cataplexy was required. Cataplexy was scored when a sudden drop in EMG tone was observed after at least two consecutive epochs of wake or drowsy.
Blood Chemistry and Hematology
During chronic drug administration, blood was collected after the FECTs (at approximately 1300) once during the baseline session and once after the termination of the drug session to monitor changes in blood chemistry (total protein, albumin, globulin, total bilirubin, serum glutamic-oxaloacetic transaminse (SGOT), serum glutamic-pyruvate transaminase (SGPT), gamma-glutamyltransferase, alkaline phosphatase, cholesterol, blood urea nitrogen, creatinine, creatinine phosphokinase, and glucose), and hematology (hemoglobin, hematocrit, and blood cell counts (platelet, neutrophil, lymphocyte, monocyte, and eosinophil)). The assay was performed at the Stanford University Department of Comparative Medicine Diagnostic Laboratory.
Serum TSH, T3, and T4 Measurements
The time course of action of the effect of acute oral administration of CG-3703 on serum TSH levels was measured in six narcoleptic animals. Blood (5ml) was collected at −0.5, 0, 0.5, 1, 2, 4, and 8 hours after oral administration of 16 mg/kg of CG-3703. After collection, samples were kept at room temperature for 30 minutes then centrifuged at 3000 rpm at 25°C for 15 minutes. Serum was then collected into Eppendorf tubes and frozen at −80°C until the assay was performed. TSH concentrations were measured using Coat-A-Count Canine TSH IRMA (DPC, Los Angeles, CA).
To assess the effects of chronic oral administration of CG-3703 on thyroid function, serum triiodothyronine (T3), free thyroxine (T4), and TSH concentrations were measured. Blood (5 ml) was collected at 1300 on days −6, −1, 4, 9, 13, and 17 during the chronic oral administration cataplexy testing session. After collection, samples were kept at room temperature for 30 minutes then centrifuged at 3000 rpm (25°C) for 15 minutes. Serum was then collected into Eppendorf tubes and frozen at −80°C until the assays were performed. T3 and free T4 concentrations were measured using Clinical Assays™ GammaCoat™ T3125I RIA Kit (Incstar Corporation®, Stillwater, MN) and the Clinical Assays™ GammaCoat™ Free T4 (Direct One-Step) 125I RIA Kit (Incstar Corporation®, Stillwater, MN), respectively. TSH concentrations were measured as with the time course of action of acute administration using Coat-A-Count Canine TSH.
Statistical Analyses
The effects of CG-3703 on cataplexy (NA and TSC), HR, BP, and T3, T4, and TSH concentrations were statistically compared using non-parametric Friedman analysis of variance (ANOVA). The effects of CG-3703 on blood chemistry and hematology parameters were compared using Wilcoxon signed rank test. Changes in the amount of sleep and wakefulness in the narcoleptic dogs were calculated using Kruskal-Wallis one-way ANOVA.
RESULTS
Effects of Acute Administration
Cataplexy
The effects of acute oral administration of CG-3703 are shown in Figure 1. CG-3703 was found to decrease the number and duration of cataplectic attacks in a dose-dependent manner (Figure 1a). A dose of 16 mg/kg, p.o. (cumulative dose: 21.25 mg/kg, p.o.) completely suppressed cataplexy in most animals (Figure 1a). Sixteen mg/kg CG-3703 was therefore administered for the time course study. Both the number and duration of cataplexy decreased with time from 0.5 to 6 hours after drug administration. Cataplexy was completely suppressed between 3 and 6 hours after drug administration. After 6 hours, the severity of cataplexy increased again, and returned to baseline by 24 hours after drug administration.
Effects of acute oral administration of CG-3703. Panel (a) displays the dose response (0.25, 1.0, 4.0, and 16.0 mg/kg p.o.), from which it was determined that a cumulative dose of 21.3mg of CG-3703 completely suppresses cataplexy in most animals (number of attacks, p < .001; time spent in cataplexy, p < .001 by Friedman's ANOVA). Panel (b) displays the number of cataplectic attacks after administration of 16mg/kg of CG-3703. At 3 hours after drug administration, the number and duration of attacks cataplectic were completely suppressed (p < .001, p < .001), returning to baseline levels by 24 hours after drug administration
Daytime sleep and wakefulness
The effect on sleep architecture of acute oral administration of CG-3703 is displayed in Table 1. CG-3703 was found to reduce the amount of REM sleep and deep sleep in narcoleptic animals in a dose-dependent manner (p = .05 and p = .04, respectively, Kruskal-Wallis). There was a tendency to increased amounts of wake, but this was only marginally significant (p = .08). For comparison, the effect of acute oral administration of CG-3703 was also assessed in a control animal. Since a dose of 8 mg/kg produced an intense increase in the amount of wakefulness in this animal (from 60.7% at the baseline to 82.6% at 8 mg/kg), we did not administer the 16 mg/kg dose. We instead administered a dose of 4 mg/kg and found that CG-3703 increased the amount of wake and decreased the amount of sleep in a dose-dependent manner in the control animal. Oral administration of CG-3703 (4 mg/kg for the control animal, 8 mg/kg for the control and narcoleptics, and 16 mg/kg for the narcoleptics) induced moderate shivering in both narcoleptic and control animals. The effects on alertness and the side effects may suggest that the control animal used was more sensitive to CG-3703. However, a larger number of animals, especially control animals, are needed to determine if there is a difference in sensitivity to TRH analogs between narcoleptic and control animals.
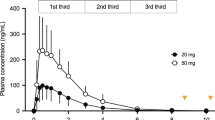
Effect on TSH concentration
Acute oral administration of CG-3703 caused a rapid initial increase in TSH concentrations (+42% from baseline at 30 minutes after drug administration). TSH concentrations subsequently decreased so that at 4 hours TSH concentrations were −65% from baseline. TSH concentrations returned to baseline by 8 hours after drug administration.
Effects of Chronic Administration
Cataplexy
The effect of chronic oral administration of CG-3703 on cataplexy is shown in Figure 2. CG-3703 completely suppressed cataplexy in all animals on the first day of drug treatment, after which animals experienced cataplexy in increasing frequency with each subsequent day (overall reduction in NA and TSC, p < .001 and p < .001, respectively, Friedman ANOVA). Throughout the first week, both NA and TSC remained below baseline. The TSC remained below baseline through the second week of drug administration, but the NA gradually increased so that it was back to baseline by the end of the two-week drug administration period. There was a slight increase from the baseline in both NA and TSC on the first day after cessation of drug administration, but both parameters returned to baseline two days after the end of the drug treatment. There were no significant fluctuations in HR (p = .17) and BP (p = .12) throughout the baseline, drug, and withdrawal periods. A significant fluctuation in RT was observed during the drug administration weeks (p = .01), but these changes did not correlate with the anticataplectic effects of CG-3703.
Effects on Cataplexy of Chronic Oral Administration of 16mg/kg CG-3703 in Six Narcoleptic Dobermans. During two weeks of drug administration, a significant reduction in the number and duration of cataplectic attacks was observed (p < .001 and p < .001, Friedman's ANOVA). The number of attacks returned to baseline levels during the second week of drug administration while the total time spent in cataplexy remained below baseline throughout the drug administration weeks. No significant fluctuations in heart rate (HR, p = .17) and blood pressure (BP, p = .12) were observed. Fluctuations in rectal temperature were statistically significant (RT, p = .01), but these fluctuations did not appear to be related to the anticataplectic effects of the compund (see also legend for Figure 3)
In order to assess whether individual dose adjustment is effective at improving efficacy, as is the case for most currently-used anticataplectic medication (Thorpy and Goswami 1990), we carried out a second chronic drug administration using the same animals. Under this design, we began by administering a starting dose of 16 mg/kg. When the reduction in NA for an animal was less than 25% of its mean NA at the baseline for two consecutive days, the dose of CG-3703 was increased by 4 mg/kg (maximum dose allowed: 32 mg/kg, p.o.; final dose range: 16 to 28 mg/kg). As with the first chronic administration session the NA and TSC were significantly reduced (overall reduction in NA and TSC p < .01 and p < .001, respectively) (Figure 3). However, unlike the fixed-dose chronic oral administration, both the NA and TSC remained below baseline levels throughout the entire two weeks of drug administration (Figure 3). Rebound cataplexy was observed after the end of drug treatment; both NA and TSC returned to baseline by three days after cessation of drug administration. There were no significant changes in HR (p = .90), BP (p = .17), and RT (p = .41).
Effects on Cataplexy of Chronic Oral CG-3703 Administration with Adjusted Dosing in Six Narcoleptic Dobermans. To determine whether dose adjustment would lead to improved efficacy, the dose of CG-3703 (starting dose: 16 mg/kg) was increased by 4 mg/kg when the reduction in cataplexy was less than 25% of baseline for two consecutive days (final dose range: 16 to 28 mg/kg). As with the fixed-dose chronic oral administration session, the number and duration of the cataplectic attacks were significantly reduced (p < .01 and p < .01, Friedman's ANOVA). However, unlike the fixed-dose chronic oral administration, both the number and duration of cataplexy remained below baseline throughout the entire two weeks of drug administration. No significant fluctuations in heart rate (HR, p = .90), blood pressure (BP, p = .17) and rectal temperature (RT, p = .41) were observed
Daytime sleep and wakefulness
During the first week of drug administration (16 mg/kg), there was an increase in the total time spent in wake, whereas the total time spent in sleep was reduced (Figure 4). The reduction in REM sleep and deep sleep were statistically significant (overall reduction in REM sleep and deep sleep p = .03 and p = .05, respectively). During week 2, the increase in wake and decrease in sleep were still observed, but these effects were less pronounced than those observed during week 1 (Figure 4). These results suggest the development of tolerance in the effect on sleep and wakefulness during chronic oral administration of CG-3703, as was the effect seen in cataplexy.
Effects of Chronic Oral Administration of 16mg/kg CG-3703 on Vigilance States in Two Narcoleptic Dobermans. In order to determine the effect of chronic oral administration of CG-3703 on sleep and wakefulness, CG-3703 was administered to two narcoleptic animals for two weeks, and polygraphic recordings were carried out during the baseline (days −4 and −3), first week (days 3 and 4), and second week (days 10 and 11) of drug administration. CG-3703 was observed to increase wake and reduced sleep, particularly deep sleep, during the first week of drug administration. During week 2, the increase in wake and the decrease in sleep are still apparent, but these effects were less pronounced than the effects observed during week 1. The effect on REM sleep and deep sleep were statistically significant (p = .03 and p = .05, Kruskal-Wallis one-way ANOVA)
Blood chemistry and hematology
The results comparing blood chemistry and hematology tests administered to the animals before and after drug treatment using data combined from both the fixed- and adjusted-dose drug administration sessions are displayed in Table 2. A significant increase in albumin and a decrease in cholesterol were observed after drug treatment when compared to baseline (albumin, p = .007; cholesterol, p = .012). It is important to note, however, that all values, including albumin and cholesterol, were within the normal range prior to and after drug treatment.
Thyroid impact
The effects of chronic oral administration of CG-3703 on serum TSH, T3, and free T4 are shown in Figure 5. No significant changes in TSH concentrations were observed during and after drug administration (p = .20). No fluctuations in serum T3 and free T4 concentrations were observed during drug administration (p = .58 and p = .07, respectively). There was a tendency to reduced T3 and free T4 concentrations after cessation of drug treatment, and the reduction in free T4 concentration was statistically significant (p = .06 and p = .02, respectively).
Effects on Serum T3 and Free T4 and TSH Levels of Chronic Oral Administration of CG-3703 in Six Narcoleptic Dobermans. (a) No significant changes in TSH levels was observed during and after drug administration (p = .20). (b) No fluctuations in serum T3 and free T4 levels were observed during the drug administration. However, there was a tendency to reduced T3 and T4 levels after cessation of drug administration, and the effect on T4 levels was statistically significant (p = .06, serum T3 levels and p = .02, serum free T4 levels, Friedman's ANOVA)
DISCUSSION
Narcolepsy is treated with CNS stimulants for EDS and antidepressants for cataplexy and abnormal REM sleep (Guilleminault 1994; Mitler et al. 1990; Thorpy and Goswami 1990). While significant progress has been made in determining the mode of action of currently-used pharmacological compounds, the treatments for narcolepsy are unsatisfactory for many patients due to side effects and incomplete efficacy (see Nishino et al. 1997). It is therefore necessary to explore compounds with improved efficacy and specificity for narcolepsy treatment. Using canine narcolepsy, we demonstrated the anticataplectic and wake-promoting effects of various biologically-stable TRH analogs (CG-3703, CG-3509 and TA-0910) (Nishino et al. 1997). The anticataplectic potency of these compounds in canine narcolepsy (CG-3703 ED50: 0.07 mg/kg, i.v.; CG-3509 ED50: 0.23 mg/kg, i.v.; and TA-0910 ED50: 0.03 mg/kg, i.v.) were comparable to desipramine (ED50: 0.02 mg/kg, i.v.) and clomipramine (ED50: 0.11 mg/kg, i.v.) (Nishino et al. 1993), currently-used anticataplectic compounds for humans. Similarly, the effective dose range of CG-3703 to increase wakefulness (200–400 μg/kg, i.v.) was comparable to d-amphetamine (100–200 μg/kg, i.v.) (Nishino et al. 1998b; Shelton et al. 1995). We therefore propose that TRH analogs may be an attractive alternative treatment for human narcolepsy. In this study, we assessed the effect and side effect profile of chronic administration of CG-3703, one of the most potent TRH analogs for reducing cataplexy and increasing sleep (Nishino et al. 1997) in canine narcolepsy.
CG-3703 is orally active: oral administration (16 mg/kg, p.o.) reproduced the anticataplectic and wake-promoting effects of intravenous administration (400 μg/kg, i.v.). This profile is preferable for the clinical application of TRH analogs, because patients can take the compound on an as-needed basis, as are most currently-used CNS stimulant and anticataplectic medication (see Thorpy and Goswami 1990). The anticataplectic effect of orally administered CG-3703 appeared rapidly (as early as 30 minutes after drug administration), lasted over 12 hours, then returned to baseline by 24 hours (Fig 1). This rapid onset and relatively long duration of action may reflect the increased CNS permeability and longer half-life of CG-3703, as compared to TRH (Flohé et al. 1983). The anticataplectic effect of CG-3703 was apparent during 2-week chronic oral administration in that TSC remained below baseline. Tolerance to the anticataplectic effect was observed, as with other anticataplectic medication (see Thorpy and Goswami 1990); NA gradually increased and returned to baseline on week 2 (Figure 2).
Acute and chronic oral administration of CG-3703 (8 and 16 mg/kg) significantly increased wakefulness and reduced sleep for 6 hours (see Table 1 and Fig 4). Tolerance to the effect on sleep and wakefulness was also observed: the increase in wake and decrease in sleep were less prominent during week 2 than week 1 (Fig 4).
Momiyama et al. reported that 18-week chronic oral administration of the TRH analog CNK-0602A (0.5–1.0 mg/kg/day) reduces tonic convulsions in spontaneously epileptic rats without affecting serum T3 and T4 levels (Momiyama et al. 1996). Similar to our results, these authors observed the development of tolerance to the anti-seizure effects of CNK-0602A at 11 weeks, although the antiepileptic effect lasted throughout the entire drug administration weeks (Momiyama et al. 1996). In our study, we further demonstrated that improved efficacy in cataplexy suppression can be achieved by individually adjusting drug dosages as needed.
No changes in HR, BP, and general behavior were observed during chronic administration. A significant fluctuation in RT during the first, but not the second, chronic oral administration session was observed, but these changes are not likely to be correlated with the anticataplectic effect of CG-3703. Shivering was observed with EMG monitoring during polygraphic recordings (where animals were kept in a small recording room (3 × 3m) with a harness strapped to the body), but not during cataplexy testing when animals moved freely in the larger (3.3 × 7.3m) testing room.
Blood chemistry and hematology results showed that all parameters tested were within the normal range both prior to and after drug treatment. There was, however, a slight, but statistically significant increase in albumin (+3.69% from baseline, from both fixed- and adjusted-dose sessions) and a significant decrease in blood cholesterol levels (−14.82% from baseline, from both fixed- and adjusted-dose sessions) after drug treatment. We did not observe any changes in appetite, body weight, hair coat condition or general behavior during chronic administration that would suggest any changes in thyroid function. Drug was administered daily at 9 A.M., and blood collection for TSH, T3 and free T4 measurement was performed at 1300 (i.e., 4 hours after drug administration). TSH, T3 and T4 concentrations remained unchanged from baseline during drug administration, although it was observed in our dogs that oral administration of CG-3703 caused a rapid initial increase in TSH levels, followed by a decrease at 4 hours, and a return to baseline by 8 hours. Ang et al. (Ang et al. 1995) reported that oral administration of TRH (40 mg) in patients with thyroid carcinoma increased TSH 4 hours after drug administration, but did not alter 131I uptake. In this study, the anticataplectic dose of CG-3703 during chronic oral administration did not alter thyroid function, and is likely to be independent of its effect on the thyroid system (see also Nishino et al. 1997). While there was a tendency to reduced serum free T4 levels after cessation of drug administration, this could be due to the abrupt withdrawal of the drug. Gradual cessation of drug treatment could blunt or eliminate this tendency.
Pharmacological studies in canine narcolepsy indicate that the adrenergic system is important for cataplexy regulation (see Nishino et al. 1994). TRH and its analogs are known to enhance NE turnover, and it is proposed that the antidepressant effect of TRH may be mediated by its NE-enhancing effects (Horst and Spirt 1974). Since antidepressants, especially selective NE uptake inhibitors, have been found to improve cataplexy (see Nishino et al. 1994; Mignot et al. 1993), it is possible that adrenergic enhancement by CG-3703 mediates its anticataplectic effect. However, this effect is not likely to be mediated by uptake inhibition, since Tuomisto reported that TRH has no effect on monoamine uptake (Tuomisto and Männistö1973). In addition to the NE uptake mechanism, we previously demonstrated that presynaptic alpha-2 and postsynaptic alpha-1 receptors are also involved in the pharmacological control of cataplexy: alpha-2 stimulation (e.g., by BHT-9210), and alpha-1 blockade (e.g., by prazosin) significantly aggravate canine cataplexy (see Mignot et al. 1988; Nishino et al. 1994). Heal et al. (1987) reported that both alpha-2 stimulation and alpha-1 blockade counteract TRH-induced locomotor activation, suggesting the possible involvement of both receptor subtypes in the mode of action of TRH-induced locomotor enhancement (Heal et al. 1987). However, TRH and its analogs do not have significant affinity to these receptors (see Metcalf (1982) for a review). Furthermore, we have previously reported that chronic oral administration of yohimbine, an alpha-2 antagonist, significantly reduced NA while TSC increased Nishino et al. 1992). This is in contrast to the anticataplectic effects of CG-3703, where TSC decreased while NA increased. Thus, the anticataplectic effect of CG-3703 may be mediated by enhancement of NE release and subsequent postsynaptic alpha-1 stimulation, and not alpha-2 antagonism, as suggested for the mode of action of locomotor enhancement (see Heal et al. 1987).
Using our canine model, we reported that CNS stimulants act via stimulation of the dopaminergic (DA) system through uptake inhibition, and/or release enhancement (Kanbayashi et al. 1998; Nishino et al. 1998b). The amphetamines and amphetamine-like stimulants increase wake and locomotion by increasing the amount of dopamine in the synapse (see Cirelli et al. 1996; Nishino, et al. 1998b). TRH and TRH analogs are also known to enhance DA transmission in the nucleus accumbens (Heal et al. 1987; Miyamoto et al. 1996), a structure important for locomotor activation (Pijnenburg et al. 1976) and EEG arousal (Nishino et al. 1998a). It is therefore possible that the effect of TRH on sleep and wakefulness is mediated by enhancement of DA turnover, a common mechanism for most CNS stimulants (Nishino et al. 1998b).
It has recently been discovered that narcolepsy in Doberman pinschers is caused by a mutation in the gene encoding a receptor, Hcrtr-2, for a novel neuropeptide, hypocretin (also called orexin) (Lin et al. 1999). The mechanism underlying the involvement of the hypocretin system in the pathophysiology of narcolepsy remains unclear. It is interesting to note, however, that hypocretin-containing neurons are exclusively localized in the lateral hypothalamus (Sakurai et al. 1998; Peyron et al. 1998), an area that is rich in TRH neurons (Kreider et al. 1985). In addition, both hypocretin and TRH receptors are G-protein coupled receptors for neuropeptides, and that the TRH receptor exhibits the second highest (25%) homology (with the Y2 neuropeptide Y receptor having the highest homology) to the hypocretin receptors (Sakurai et al. 1998), suggesting that TRH may play an important role in the pathophysiology of narcolepsy through an unknown specific interaction with the hypocretin system.
TRH has been involved in several clinical trials for various disorders such as depression, amyotrophic lateral sclerosis, and spinocerebellar degeneration, often with disappointing results (Engel et al. 1983; Metcalf 1982; Prange et al. 1972; Sobue et al. 1983), possibly due to lack of a detailed evaluation of the therapeutic effects using validated animal models. The negative results of clinical trials using TRH could therefore be explained by insufficient dosing, inappropriate routes of drug administration, drug tolerance or by the fact that TRH itself has a short half-life and poor access to the CNS (see Metcalf 1982). In the previous (Nishino et al. 1997) and current studies, we systematically explored the effective dose range, route of administration, side effect profile, and development of drug tolerance of TRH and biologically-stable TRH analogs on narcolepsy using a validated animal model. Our results thus demonstrate that TRH analogs, such as CG-3703, could be an attractive new alternative for treating human narcolepsy.
References
Aldrich MS . (1992): Narcolepsy. Neurology 42: 34–43
Ang ES, Teh HS, Sundram FX, Lee KO . (1995): Effect of lithium and oral thyrotrophin-releasing hormone (TRH) on serum thyrotrophin (TSH) and radioiodine uptake in patients with well differentiated thyroid carcinoma. Singapore Med J 36: 606–608
Baker TL, Dement WC . (1985): Canine narcolepsy-cataplexy syndrome: evidence for an inherited monoaminergic-cholinergic imbalance. In McGinty DJ, Drucker-Colin R, Morrison A, Parmeggiani PL (eds), Brain Mechanisms of Sleep. New York, Raven Press, pp 199–233
Boler J, Enzmann F, Folkers K, Bowers CY, Schally AV . (1969): The identity of chemical and hormonal properties of the thyrotropin releasing hormone and pyroglutamyl-histidyl-proline-amide. Biochem Biophys Res Commun 37: 705–710
Cirelli C, Pompeiano M, Tononi G . (1996): Neuronal gene expression in the waking state: a role for the locus coeruleus. Science 274: 1211–1215
Engel WK, Siddique T, Nicoloff J . (1983): Effect on weakness and spasticity in amyotrophic lateral sclerosis of thyrotropin-releasing hormone. Lancet 2: 73–75
Flohé L, Bauer K, Friderichs E, Gunzler W, Hennies H, Herrling S, Lagler F, Otting F, Schwertner E . (1983): Biological effects of degradation-stabilized TRH analogues. In Griffiths E, Bennett G (eds), Thyrotropin-releasing hormone. New York, Raven Press, pp 327–340
Griffiths EC, Bennett GW . (1987): Clinical applications of thyrotropin-releasing hormone. Clin Sci 73: 449–457
Guilleminault C . (1994): Narcolepsy Syndrome. In Kryger MH, Roth T, Dement WC (eds), Principles and Practice of Sleep Medicine, ed. Philadelphia, W. B. Saunders Company, pp 549–561
Heal DJ, Stoodley N, Elliott JM, Marsden CA, Bennet GW, Youdim MBH . (1987): Behavioural and biochemical evidence for the release of noradrenaline in mouse brain by TRH and some of its biologically stable analogues. Neuropharmacology 26: 313–322
Horst WD, Spirt N . (1974): A possible mechanism for the anti-depressant activity of thyrotropin-releasing hormone. Life Sciences 15 (6): 1073–1082
Jackson IMD . (1982): Thyrotropin-releasing hormone. N Engl J Med 306: 145–155
Kaitin KI, Kilduff TS, Dement WC . (1986): Sleep fragmentation in genetically narcoleptic dogs. Sleep 9: 116–119
Kanbayashi T, Honda K, Kodama T, Mignot E, Nishino S . (1998): Increased dopaminergic transmission mediates wake-promoting effects of amphetamine isomers. Soc Neurosci Abstract 23: 954
Kolesnick RN, Gershengorn MC . (1985): Thyrotropin-releasing hormone and the pituitary: new insights into the mechanisms of stimulated secretion and clinical usage. Am J Med 79: 729–739
Kreider MS, Engber TM, Nilaver G, Zimmerman EA, Winokur A . (1985): Immunohistochemical localization of TRH in rat CNS: comparison with RIA studies. Peptides 6: 997–1000
Lin L, Faraco J, Li R, Kadotani H, Rogers W, Lin X, Qiu X, de Jong P, Nishino S, Mignot E . (1999): The sleep disorder canine narcolepsy is caused by a mutation in the hypocretin (orexin) receptor 2 gene. Cell 98: 365–376
Metcalf G . (1982): Regulatory peptides as a source of new drugs: the clinical prospects for analogs of TRH which are resistant to metabolic degradation. Brain Res Rev 4: 389–408
Mignot E, Guilleminault C, Bowersox S, Rappaport A, Dement WC . (1988): Role of central alpha-1 adrenoceptors in canine narcolepsy. J Clin Invest 82: 885–894
Mignot E, Renaud A, Nishino S, Arrigoni J, Guilleminault C, Dement WC . (1993): Canine cataplexy is preferentially controlled by adrenergic mechanisms: evidence using monoamine selective uptake inhibitors and release enhancers. Psychopharmacology 113: 76–82
Mitler MM, Hajdukovic R, Erman M, Koziol JA . (1990): Narcolepsy. J Clin Neurophysiol 7: 93–118
Miyamoto T, Ishihara K, Kimura K, Naoyuki T, Fujita Y, Serikawa T, Sasa M . (1996): Long-term antiepileptic effects of chronic intake of CNK-602A, a thyrotropin-releasing hormone analogue on spontaneously-epileptic rats. Epilepsia 37: 328–331
Momiyama T, Ishihara K, Kimura K, Naoyuki T, Fujita Y, Serikawa T, Sasa M . (1996): Long-term antiepileptic effects of chronic intake of CNK-602A, a thyrotropin-releasing hormone analogue on spontaneously-epileptic rats. Epilepsia 37: 328–331
Nishino S, Arrigoni J, Fruhstorfer B, Shelton J, Dement WC, Mignot E . (1992): Effects of chronic administration of yohimbine (alpha-2 antagonist) on cataplexy and platelet alpha-2 receptors of narcoleptic canines. Sleep Research 21: 66
Nishino S, Arrigoni J, Shelton J, Dement WC, Mignot E . (1993): Desmethyl metabolites of serotonergic uptake inhibitors are more potent for suppressing canine cataplexy than their parent compounds. Sleep 16: 706–712
Nishino S, Arrigoni J, Shelton J, Kanbayashi T, Tafti A, Dement WC, Mignot E . (1997): Effects of thyrotropin-releasing hormone and its analogs on daytime sleepiness and cataplexy in canine narcolepsy. J Neurosci 17: 6401–6408
Nishino S, Honda K, Riehl J, Mignot E . (1998a): Extracellular single unit recordings of dopaminergic output neurons in the nucleus accumbens and globus pallidus in narcoleptic Dobermans. J Sleep Res 7: S2: 187
Nishino S, Mao J, Sampathkumaran R, Shelton J, Mignot E . (1998b): Increased dopaminergic transmission mediates the wake-promoting effects of CNS stimulants. Sleep Research Online 1: 49–61. http://www.sro.org/1998/Nishino/49/
Nishino S, Mignot E . (1997): Pharmacological aspects of human and canine narcolepsy. Prog Neurobiol 52: 27–78
Nishino S, Reid MS, Dement WC, Mignot E . (1994): Neuropharmacology and neurochemistry of canine narcolepsy. Sleep 17: S84–92
Nishino S, Riehl J, Hong J, Kwan M, Honda K, Dement W, Mignot E . (1998c): REM sleep cyclicity is intact in narcoleptic canines. Soc Neurosci Abstract 23: 938
Nishino S, Tafti M, Reid MS, Shelton J, Siegel JM, Dement WC, Mignot E . (1995): Muscle atonia is triggered by cholinergic stimulation of the basal forebrain: implication for the pathophysiology of canine narcolepsy. J Neurosci 15: 4806–4814
Peyron C, Tighe DK, van den Pol AN, de Lecea L, Heller HC, Sutcliffe JG, Kilduff TS . (1998): Neurons containing hypocretin (orexin) project to multiple neuronal systems. J Neurosc 18: 9996–10015
Pijnenburg AJ, Honig WM, Van der Heyden JA, Van Rossum JM . (1976): Effects of chemical stimulation of the mesolimbic dopamine system upon locomotor activity. Eur J Pharmacology 35: 45–58
Prange A, Wilson I, Lara P, Alltop L, Breese G . (1972): Effects of thyrotropin-releasing hormone in depression. Lancet 2: 999–1002
Riehl J, Nishino S, Cederberg R, Dement WC, Mignot E . (1998): Development of cataplexy in genetically narcoleptic Dobermans. Exp Neurol 152: 292–302
Sakurai T, Amemiya A, Ishii M, Matsuzaki I, Chemelli RM, Tanaka H, Williams SC, Richardson JA, Kozlowsky GP, Wilson S, Arch JRS, Buckingham RE, Haynes AC, Carr SA, Annan RS, McNulty DE, Liu W, Terrett JA, Eishourbagy NA, Bergsma DJ, Yanagisawa M . (1998): Orexins and orexin receptors: A family of G protein-coupled receptors that regulate feeding behavior. Cell 92: 573–585
Sharif N . (1985): Diverse roles of thyrotropin-releasing hormone in brain, pituitary and spinal cord function. Trends Pharmacol Sci 6: 119–122
Shelton J, Nishino S, Vaught J, Dement WC, Mignot E . (1995): Comparative effects of modafinil and amphetamine on daytime sleepiness and cataplexy of narcoleptic dogs. Sleep 18: 817–826
Sobue I, Takayanagi T, Nakanishi T, Tsubaki T, Uono M, Kinoshita M, Igata A, Miyazaki M, Yoshida M, Ando K, Maruyama S, Mitsuma T, Nihei N, Sakuma A, Kato K . (1983): Controlled trial of thyrotropin releasing hormone tartrate in ataxia of spinocerebellar degenerations. J Neuro Sci 61: 235–248
Thorpy MJ, Goswami M . (1990): Treatment of narcolepsy. In Thorpy MJ (ed), Handbook of Sleep Disorders, ed. New York, Marcel Dekker, Inc., pp 235–258
Tuomisto J, Männistö P . (1973): Amine uptake and thyrotropin-releasing hormone. Lancet 836
Winokur A, Manaker S, Kreider M . (1989): TRH and TRH receptors in the spinal cord. Ann New York Acad Sci 553: 314–324
Acknowledgements
The authors would like to thank J. Shelton, S. von Richthofen, and the staff of the Department of Comparative Medicine for technical assistance. This work was supported by NS 27710, NS23724 and MH01600.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Riehl, J., Honda, K., Kwan, M. et al. Chronic Oral Administration of CG-3703, a Thyrotropin Releasing Hormone Analog, Increases Wake and Decreases Cataplexy in Canine Narcolepsy. Neuropsychopharmacol 23, 34–45 (2000). https://doi.org/10.1016/S0893-133X(99)00159-1
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1016/S0893-133X(99)00159-1
Keywords
This article is cited by
-
Analysis of thyroid function and related factors in narcolepsy patients
Scientific Reports (2023)