Abstract
Preclinical findings on the role of corticotropin releasing hormone (CRH) in stress and anxiety, on the interaction of CRH and cholecystokinin (CCK) in modulating anxiety, as well as the blunted corticotropin (ACTH) response to CRH in panic disorder suggest that CRH may play a role in panic disorder. To further characterize the role of the hypothalamic-pituitary-adrenocortical (HPA) system in panic disorder, we compared patients with and without CCK tetrapeptide (CCK-4) induced panic attacks. Twenty-four patients with panic disorder were given injections of CCK-4 (25 μg). Panic attacks, psychopathological changes, as well as ACTH and cortisol secretion were recorded. Fifteen of the 24 patients experienced a panic attack after CCK-4. ACTH secretion was significantly higher in the patients with CCK-4-induced panic attacks than in those without such attacks. The patients without CCK-4-induced attacks had a brief but less pronounced increase in ACTH concentrations. Cortisol concentrations were not significantly increased after CCK-4 administration. The increased ACTH concentrations suggest that the activation of the HPA system in CCK-4-induced panic attacks plays a physiological role. CRH may be involved in experimentally-occurring and perhaps in naturally-occurring panic attacks as well.
Similar content being viewed by others
Main
Cholecystokinin tetrapeptide (CCK-4) has been reported to have an enhanced panicogenic effect in panic disorder (Bradwejn et al. 1991). Like sodium lactate- and CO2-induced panic, CCK-4-induced attacks are accompanied by hyperventilation and resemble the pattern of panic symptoms induced by CO2 administration (Bradwejn et al. 1991). In contrast to the “respiratory” panicogens sodium lactate and CO2 (Coplan and Klein 1996), CCK has been further reported to activate the hypothalamic-pituitary-adrenocortical (HPA) system (de Montigny 1989; Koszycki et al. 1996; Kellner et al. 1997). It has been suggested that this effect is primarily pharmacological and unrelated to the experimentally-induced panic (Abelson et al. 1994). However, in healthy control subjects, enhanced corticotropin (ACTH) and cortisol secretion has been linked recently to panic-like symptoms (Koszycki et al. 1998).
To further characterize the role of the HPA system in experimentally-induced panic attacks in patients with panic disorder we compared ACTH and cortisol concentrations in patients with and without CCK-4-induced panic attacks.
METHODS
Twenty-four patients (nine women and fifteen men; mean age = 38.1 years, SD = 10.8) with a diagnosis of panic disorder but without a comorbid axis I disorder, as assessed with the Structured Clinical Interview for DSM-IV (Wittchen et al. 1997) were studied. These subjects had been medication-free for at least 10 days and had undergone thorough medical examination to rule out other illnesses, drug intake, and lifestyles that could interfere with the study. The protocol was approved by the local ethics committee for human experiments. After complete description of the study to the subjects, written informed consent was obtained.
All subjects were studied from 9:00 a.m. to 1:00 p.m. in a supine position in a soundproof room with a single bed (Kellner et al. 1995, 1997; Ströhle et al. 1998b, 1999). Each subject received a bolus injection of 25 μg CCK-4 (Clinalfa, Laufelfingen, Switzerland) dissolved in 10 ml 0.9% saline at 11:00 a.m.. The Acute Panic Inventory (Dillon et al. 1987) was administered at 11:00 a.m. and 11:05 a.m. by a rater blind to the procedure; the maximum intensity during the observation period was noted. For a decision that a panic attack had occurred, an Acute Panic Inventory total score exceeding 20 and an increment of at least 14 points over the preinjection score (Dillon et al. 1987; Ströhle et al. 1998b) was required. According to these criteria, 15 patients experienced a CCK-4-induced panic attack (mean age = 37.4 years, SEM = 2.6) and 9 (mean age = 39.3 years, SEM = 4.1) did not. On an exploratory level, no reasonable group differences were found for the mean age of onset (panickers: 26.8 years; nonpanickers: 27.2 years), severity of panic and agoraphobia (panickers: 23.8; nonpanickers: 23.2) (Bandelow 1995), Hamilton depression scale scores (panickers: 8.5; nonpanickers: 7.3) (Hamilton 1960), Hamilton anxiety scale scores (panickers: 14.0; nonpanickers: 14.3) (Hamilton 1959,) and baseline Acute Panic Inventory scores (panickers: 4.9; nonpanickers: 6.4). The mean maximum Acute Panic Inventory score was 14.4 (SEM = 2.9) in the patients without CCK-4-induced panic attacks and 28.1 (SEM = 1.6) in those with such attacks.
For all patients, blood samples were taken at the time points 11:00 (baseline), 11:05, 11:10, 11:20, and 11:30 a.m. for the determination of the plasma ACTH and cortisol concentrations. ACTH plasma immunoreactivity was measured using a commercially available immunoradiometric assay (Nichols, San Juan Capistrano, CA) with a sensitivity of 4 pg/ml of plasma. Our intra- and interassay coefficients of variation were below 10% at 20 pg/ml. For cortisol a commercial radioimmunoassay kit was employed (ICN Biomedicals Inc, Carson CA) with a sensitivity of 7 ng/ml of plasma. Our intra- and interassay coefficients of variation were below 5% at 40 ng/ml.
For statistical comparison of the ACTH concentrations and the cortisol concentrations between the two groups and the various time points, a two-factorial analysis of variance (ANOVA) with a repeated-measures design was performed. Time was the within-subject factor (five levels) and group, i.e., patients with panic disorder with and without CCK-4-induced attacks, comprised the between-subjects factor (two levels). Main effects and interactions of these factors were tested about significance by multivariate criteria such as Wilks' lambda and its approximated F-value. Variables that contributed significantly to these effects, were identified by univariate F-tests. When significant main effects or interactions were found for a variable, tests with contrasts followed in ANOVA to locate the time points with significant differences in the means of that particular variable. Tests with contrasts at each time point were carried out for testing of the significant group mean differences in ACTH and cortisol concentrations during the observation period. To approach normality and homogeneity in the data, the variables of plasma hormonal concentrations used in the analysis were transformed with the log-transformation (x* = ln[x]) before analysis. Alpha = 0.05 was accepted as a nominal level of significance. To keep the type I error ≤ 0.05, all posteriori tests (univariate F-test and tests with contrasts) were performed at a reduced level of significance (adjusted alpha according to the Bonferroni procedure).
RESULTS
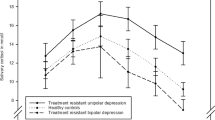
Analysis of variance revealed significant main effects and interactions for ACTH concentrations (Wilks' multivariate tests of significance; effect of group (panic attack occurrence): approximated F = 4.45, df = 1, 22, p = .046; effect of time: approximated F = 8.46, df = 4, 19, p = .001; effect of group x time: approximated F = 2.96, df = 4, 19, p = .046). Tests with contrasts between the various time points within each patient's group revealed that compared to baseline, ACTH concentrations were significantly increased after CCK-4 at 11:05 a.m. and 11:10 a.m. in patients without attacks (tests with contrasts; p < .05) and at 11:05, 11:10, 11:20, and 11:30 a.m. in patients with CCK-4-induced panic attacks (tests with contrasts p < .05). Furthermore, compared to the ACTH concentrations in nonpanickers, those in panickers were significantly higher at 11:05, 11:10, and 11:20 a.m. (tests with contrasts; p < .05).
For the cortisol concentrations, only a nonsignificant trend was observed for time (Wilk's multivariate tests of significance; effect of time: approximated F = 2.73, df = 4, 19, p = .06). No significant effect of panic attack occurrence and no interaction between factors time and panic attack occurrence were found (Figure 1). Thus, both patient groups show some increase in the cortisol concentrations with time, but this increase is not statistically significant compared to baseline. Furthermore, the differences between the two groups are not significant in all the time points, even if patients with attacks have higher concentration values than those without attacks.
DISCUSSION
The major finding of our study is that patients with panic disorder that experienced a CCK-4-induced panic attack had enhanced ACTH concentrations. On the other hand, those without an attack had a brief and less remarkable increase. Cortisol concentrations were not significantly influenced by neither CCK-4 administration nor the occurrence of panic attacks.
In contrast to the “respiratory” panicogens sodium lactate and CO2, CCK-4 induces short-lived panic attacks (Bradwejn et al. 1991; Bradwejn and Koszycki 1991), possibly related to its rapid intravenous administration, producing very transient period of gasping respiratory stimulation and an exaggerated pituitary response with an increased secretion of ACTH. Studies investigating the role of CCK-4 as a panicogen, suggest that this agent seems to be a valid human model, satisfying at least six out of seven proposed criteria for an ideal panicogen (Guttmacher et al. 1983; van Megen et al. 1996b). Criterium seven, i.e., drugs which are clinically ineffective in panic disorder are unable to block CCK-4 induced attacks, has been studied only in healthy volunteers (de Montigny 1989; Bradwejn et al. 1994). Like sodium lactate- and CO2-induced panic, CCK-4-induced attacks are blocked by antipanic treatment with antidepressants (Bradwejn and Koszycki 1994; van Megen et al. 1997; Shlik et al. 1997) or benzodiazepines (de Montigny 1989). Although CCK antagonists have so far failed to be effective in the treatment of panic disorder (Kramer et al. 1995) or benzodiazepine withdrawal induced anxiety (Abelson et al. 1995), CCK-4 induced attacks are a promising strategy to elucidate the neurobiological correlates of panic disorder.
In patients with panic disorder, administration of CCK-4 has been shown to stimulate ACTH, whereas cortisol concentrations remain unaffected (van Megen et al. 1996a; Kellner et al. 1997; Shlik et al. 1997). In healthy subjects, increased ACTH and cortisol secretion after CCK-4 administration (de Montigny 1989; Palmour et al. 1993; Koszycki et al. 1996), and a further enhancement in subjects with panic-like symptoms (Koszycki et al. 1998) have been reported. Our results in patients with panic disorder indicate that CCK-4 has a nonpharmacological effect on the HPA system and suggest a physiological role of the increased ACTH concentrations in patients with CCK-4-induced panic attacks. CRH is the principal secretagogue for ACTH, which is produced in the anterior pituitary. Moreover, CRH has neurotransmitter-like properties outside the hypothalamus (Hayden-Hixson and Nemeroff 1993). CRH-containing neurons innervate noradrenergic centers in the pons (locus coeruleus) and the central nucleus of the amygdala, areas of recognized importance in anxiety and stress response (Gorman et al. 1989; Holsboer et al. 1992; Heit et al. 1997). Furthermore, preclinical data indicate that CRH may play a role in the anxiogenic (Biro et al. 1993) and endocrine (Kamilaris et al. 1992) effects of CCK. However, it should be noted that CCK may activate pituitary ACTH secretion, not only via CRH, but also via other neurohormones such as oxytocin and vasopressin (Carter and Lightman 1987; Verbalis et al. 1986). The described association of CCK-4 induced panic attacks and an exaggerated pituitary ACTH response together with the known behavioral effects of CRH (for review see: Dunn and Berridge 1990; Holsboer et al. 1992; Owens and Nemeroff 1992) are in favor of CRH mediating the panicogenic activity of CCK-4 in patients with panic disorder.
In contrast to healthy control subjects (Koszycki et al. 1998), and in line with previous reports (van Megen et al. 1996a; Kellner et al. 1997; Shlik et al. 1997) our patients with panic disorder seem to lack a clearly enhanced cortisol secretion after CCK-4 administration. However, certain effects on cortisol concentrations may be missed because of the limited time interval studied. Alternative explanations for this discrepancy that should be further investigated are delayed or reduced responsivity of the adrenal cortex to the ACTH stimulus. Furthermore, the anxiolytic peptide atrial natriuretic peptide (ANP) (Ströhle et al. 1997) has been shown to inhibit the stimulated HPA system (Kellner et al. 1992; Ströhle et al. 1998a) and has been suggested to explain the unresponsiveness of the HPA system in lactate-induced panic attacks (Kellner et al. 1995). Although ANP has effects on ACTH and cortisol concentrations, in view of the described increase in the pituitary-adrenocortical ratio (Ströhle et al. 1998a), an exaggerated release of ANP during CCK-4 induced panic attacks may, at least in part, explain the dissociation of ACTH and cortisol concentrations.
It is of interest that pentagastrin, a 5-amino acid synthetic peptide, increases cortisol concentrations both in patients with panic disorder and in healthy control subjects, with the maximum occurring 20 minutes after administration (Abelson et al. 1991, 1994). The lack of an increase in cortisol secretion in patients with CCK-4-induced panic attacks is in line with studies of spontaneous or situational panic attacks (Cameron et al. 1987; Woods et al. 1987) as well as lactate-induced panic attacks (Liebowitz et al. 1985; Levin et al. 1987; Kellner et al. 1995; Ströhle et al. 1998b). However, because ACTH concentrations were not reported in the studies of panic attacks not elicited by pharmacological challenges, the increase seen in patients with panic disorder and CCK-4-induced panic attacks leaves open the question of whether spontaneous or situationally predisposed panic attacks are accompanied by increased ACTH secretion as well.
In summary, our finding of an enhanced ACTH secretion during CCK-4-induced panic attacks in patients with panic disorder suggests that CRH may play a physiological role in these experimentally induced attacks. Together with the blunted ACTH response to CRH in patients suffering from panic disorder (Roy-Byrne et al. 1986; Holsboer et al. 1987), our data give further evidence for a role of CRH in panic disorder and experimentally induced attacks. During panic attacks ACTH secretion may be enhanced despite the lack of clear effects on cortisol concentrations.
References
Abelson JL, Nesse RM, Vinik A . (1991): Stimulation of corticotropin release by pentagastrin in normal subjects and patients with panic disorder. Biol Psychiatry 29: 1220–1223
Abelson JL, Nesse RM, Vinik AI . (1994): Pentagastrin infusions in patients with panic disorder. II. Neuroendocrinology. Biol Psychiatry 36: 84–96
Abelson JL, Curtis GC, Nesse R, Fantone R, Pyke RE, Bammert-Adams J . (1995): The effects of central cholecystokinin receptor blockade on hypothalamic-pituitary-adrenal and symptomatic responses to overnight withdrawal from alprazolam. Biol Psychiatry 37: 56–59
Bandelow B . (1995): Assessing the efficacy of treatments for panic disorder and agoraphobia. II. The panic and agoraphobia scale. Int Clin Psychopharmacol 10: 73–81
Biro E, Sarnyai Z, Penke B, Szabo G, Telegdy G . (1993): Role of endogenous corticotropin-releasing factor in mediation of neuroendocrine and behavioral response to cholecystokinin octapeptide sulfate ester in rats. Neuroendocrinology 57: 340–345
Bradwejn J, Koszycki D . (1991): Comparison of the panicogenic effects of cholecystokinin 30–33 and carbon dioxide in panic disorder. Prog Neuropsychopharmacol Biol Psychiatry 15: 237–239
Bradwejn J, Koszycki D, Shriqui C . (1991): Enhanced sensitivity to cholecystokinin tetrapetide in panic disorder. Arch Gen Psychiatry 48: 603–610
Bradwejn J, Koszycki D . (1994): Imipramine antagonism of the panicogenic effects of cholecystokinin tetrapeptide in panic disorder patients. Am J Psychiatry 151: 261–263
Bradwejn J, Koszycki D, Couëtoux du Tertre A, Paradis M, Bourin M . (1994): Effects of flumazenil on cholecystokinin-tetrapeptide-induced panic attacks in healthy volunteers. Psychopharmacology 114: 257–261
Cameron OG, Lee MA, Curtis GC, McCann DS . (1987): Endocrine and physiological changes during “spontaneous” panic attacks. Psychoneuroendocrinology 12: 321–331
Carter DA, Lightman SL . (1987): A role for the area postrema in mediating cholecystokinin-stimulated oxytocin secretion. Brain Res 435: 327–330
Coplan JD, Klein DF . (1996): Pharmacological probes in panic disorder. In Westenberg HGM, Den Boer JA, Murphy DL (eds), Advances in the Neurobiology of Anxiety Disorders. Chichester, Wiley, pp 173–196
de Montigny C . (1989): Cholecystokinin tetrapeptide induces panic-like attacks in healthy volunteers: Preliminary findings. Arch Gen Psychiatry 46: 511–517
Dillon DJ, Gorman JM, Liebowitz MR, Fyer AJ, Klein DF . (1987): Measurement of lactate-induced panic and anxiety. Psychiatry Res 1987; 20: 97–105
Dunn AJ, Berridge CW . (1990): Physiological and behavioral response to corticotropin-releasing factor administration: Is CRF a mediator of anxiety or stress response? Brain Res Rev 15: 71–100
Gorman JM, Liebowitz MR, Fyer AJ, Stein J . (1989): A neuroanatomical hypothesis for panic disorder. Am J Psychiatry 146: 148–161
Guttmacher LB, Murphy DL, Insel TR . (1983): Pharmacologic models of anxiety. Compr Psychiatry 24: 312–326
Hamilton M . (1960): A rating scale for depression. J Neurol Neurosurg Psychiatry 23: 56–62
Hamilton M . (1959): The assessment of anxiety states by rating. Br J Med Psychol 32: 50–55
Hayden-Hixson DM, Nemeroff CB . (1993): Role(s) of neuropeptides in responding and adaption to stress: A focus on corticotropin-releasing factor and opioid peptides. In Stanford SC, Salmon P (eds), Stress: From Synapse to Syndrome. London, Academic Press, pp 355–391
Heit S, Owens MJ, Plotsky P, Nemeroff CB . (1997): Corticotropin-releasing factor, stress, and depression. Neuroscientist 3: 186–194
Holsboer F, von Bardeleben U, Buller R, Heuser I, Steiger A . (1987): Stimulation response to corticotropin-releasing hormone (CRH) in patients with depression, alcoholism and panic disorder. Horm Metab Res Suppl 16: 80–88
Holsboer F, Spengler D, Heuser I . (1992): The role of corticotropin-releasing hormone in the pathogenesis of Cushing's disease, anorexia nervosa, alcoholism, affective disorders and dementia. Prog Brain Res 93: 385–417
Kamilaris TC, Johnson EO, Calogero AE, Kalogeras KT, Bernardini R, Chousos GP, Gold PW . (1992): Cholecystokinin-octapeptide stimulates hypothalamic-pituitary-adrenal function in rats: Role of corticotropin-releasing hormone. Endocrinology 130: 1764–1774
Kellner M, Wiedemann K, Holsboer F . (1992): ANF inhibits the CRH-stimulated secretion of ACTH and cortisol in man. Life Sci 50: 1835–1842
Kellner M, Herzog L, Yassouridis A, Holsboer F, Wiedemann K . (1995): A possible role of atrial natriuretic hormone in pituitary-adrenocortical unresponsiveness in lactate-induced panic. Am J Psychiatry 152: 1365–1367
Kellner M, Yassouridis A, Jahn H, Wiedemann K . (1997): Influence of clonidine on psychopathological, endocrine and respiratory effects of cholecystokinin tetratpeptide in patients with panic disorder. Psychopharmacology 133: 55–61
Koszycki D, Zabarcko RM, Le Melledo J-M, Young S, Bradwejn J . (1996): Effect of acute tryptophan depletion on behavioral, cardiovascular and hormonal sensitivity to cholecystokinin-tetrapeptide challenge in healthy volunteers. Biol Psychiatry 40: 648–655
Koszycki D, Zacharko RM, Le Melledo J-M, Bradwejn J . (1998): Behavioral, cardiovascular, and neuroendocrine profiles following CCK-4 challenge in healthy volunteers: A comparison of panickers and nonpanickers. Depression Anxiety 8: 1–7
Kramer MS, Cutler NR, Ballenger JC, Patterson WM, Mendels J, Chenault A, Shrivastava R, Matzurah-Wolfe D, Lines C, Reines S . (1995): A placebo-controlles trial of L-365,260, a CCKB antagonist in panic disorder. Biol Psychiatry 37: 462–466
Levin AP, Doran AR, Liebowitz MR, Fyer AJ, Gorman JM, Klein DF, Paul SM . (1987): Pituitary adrenocortical unresponsiveness in lactate-induced panic. Psychiatry Res 21: 23–32
Liebowitz MR, Gorman JM, Fyer AJ, Levitt M, Dillon D, Levy G, Appleby IL, Anderson S, Palij M, Davies SO, Klein DF . (1985): Lactate provocation of panic attacks. II. Biochemical and physiological findings. Arch Gen Psychiatry 42: 709–719
Owens MJ, Nemeroff CB . (1992): The physiology and pharmacology or corticotropin-releasing factor. Pharmacol Rev 43: 425–473
Palmour RM, Bradwejn J, Merani S, Meaney MJ, Koszycki D, Boulenger J-P, Ervin FR . (1993): Neuroendocrine correlates of CCK-4-induced anxiety and panic in normal human volunteers and in vervet monkeys. Neuropsychopharmacology 9: 121S
Roy-Byrne PP, Uhde TW, Post RM, Gallucci W, Chousos GP, Gold PW . (1986): The corticotropin-releasing hormone stimulation test in patients with panic disorder. Am J Psychiatry 143: 896–899
Shlik J, Aluoja A, Vasar V, Vasar E, Podar T, Bradwejn J . (1997): Effects of citalopram treatment on behavioural, cardiovascular and neuroendocrine response to cholecystokinin tetrapeptide challenge in patients with panic disorder. J Psychiatry Neurosci 22: 332–340
Ströhle A, Jahn H, Montkowski A, Liebsch G, Boll E, Landgraf R, Holsboer F, Wiedemann K . (1997): Central and peripheral administration of atriopeptin is anxiolytic in rats. Neuroendocrinology 65: 210–215
Ströhle A, Kellner M, Holsboer F, Wiedemann K . (1998a): Atrial natriuretic hormone decreases endocrine response to a combined dexamethasone corticotropin-releasing hormone test. Biol Psychiatry 43: 371–375
Ströhle A, Kellner M, Yassouridis A, Holsboer F, Wiedemann K . (1998b): Effect of flumazenil in lactate-sensitive patients with panic disorder. Am J Psychiatry 155: 610–612
Ströhle A, Kellner M, Holsboer F, Wiedemann K . (1999): Behavioral, neuroendocrine and cardiovascular response to flumazenil: No evidence for an altered benzodiazepine receptor sensitivity in panic disorder. Biol Psychiatry 45: 321–326
van Megen HJGM, Westenberg HGM, Den Boer JA, Kahn RS . (1996a): The panic inducing properties of the cholecystokinin tetrapeptide CCK-4 in patients with panic disorder. Eur Neuropsychopharmacol 6: 187–194
van Megen HJGM, Westenberg HGM, Den Boer JA, Kahn RS . (1996b): Cholecystokinin in panic disorder. In Westenberg HGM, Den Boer JA, Murphy DL (eds), Advances in the Neurobiology of Anxiety Disorders. Chichester, Wiley, pp 197–227
van Megen HJGM, Westenberg HGM, Den Boer JA, Slaap B, Sheepmakers A . (1997): Effect of the selective serotonin reuptake inhibitor fluvoxamine on CCK-4 induced panic attacks. Psychopharmacology 129: 357–364
Verbalis JG, McCann MJ, McHale CM, Stricker EM . (1986): Oxytocin secretion in response to cholecystokinin and food: Differentiation of nausea from satiety. Science 232: 1417–1419
Wittchen H-U, Wunderlich U, Gruschwitz S, Zaudig M . (1997): SKID-I Strukturiertes Klinisches Interview Für DSM-IV. Göttingen, Hogrefe
Woods SW, Charney DS, McPherson CA, Gradman AH, Heninger GR . (1987): Situational panic attacks. Behavioral, physiologic, and biochemical characterization. Arch Gen Psychiatry 44: 365–375
Acknowledgements
The authors thank Alexander Yassouridis, Ph.D., for statistical advice and Gisela Gajewsky for technical assistance.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Ströhle, A., Holsboer, F. & Rupprecht, R. Increased ACTH Concentrations Associated with Cholecystokinin Tetrapeptide-Induced Panic Attacks in Patients with Panic Disorder. Neuropsychopharmacol 22, 251–256 (2000). https://doi.org/10.1016/S0893-133X(99)00115-3
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1016/S0893-133X(99)00115-3
Keywords
This article is cited by
-
Evaluation of the CCK-4 model as a challenge paradigm in a population of healthy volunteers within a proof-of-concept study
Psychopharmacology (2007)
-
Tryptophan depletion does not modify response to CCK-4 challenge in patients with panic disorder after treatment with citalopram
Psychopharmacology (2006)
-
Effects of Alprazolam on Cholecystokinin-Tetrapeptide-Induced Panic and Hypothalamic–Pituitary–Adrenal-Axis Activity: A Placebo-Controlled Study
Neuropsychopharmacology (2003)
-
Die experimentelle Provokation von Panikattacken als humanexperimentelles Angstmodell
Der Nervenarzt (2003)