Abstract
Using in vivo single-unit recording in rats, we compared the effects of continuous cocaine infusion via minipump or single daily injections (both 40 mg/kg/d × 14 days, SC) on the activity of putative dopamine (DA) neurons in the substantia nigra pars compacta (SNC) and ventral tegmental area (VTA). On days 1–5 after cocaine withdrawal, animals were further treated with single daily injections of DA agonists. On withdrawal day 7 continuous cocaine caused a reduction in spontaneously active neurons in the SNC and reduced bursting in the VTA. In contrast, intermittent cocaine resulted in an increase in the number of active neurons in the VTA. These changes were all reversed by apomorphine or quinpirole given during the first 5 withdrawal days. The D1 antagonist SCH 39166 did not antagonize the effects of apomorphine in either region. The role of D2 receptors in modulating baseline DA activity during intermediate cocaine withdrawal is discussed.
Similar content being viewed by others
Main
The two opposite behavioral outcomes in animal models of chronic cocaine or amphetamine abuse are sensitization and tolerance, which are induced by intermittent injection or continuous infusion, respectively (Inada et al. 1992; King et al. 1992; Lau et al. 1991; Post and Rose 1976; Reith et al. 1987). Behavioral sensitization has been hypothesized as a model of the increasing reinforcing effects of cocaine in humans, especially during the early stages of abuse (Kilbey and Ellinwood 1977; Post and Contel 1983; Robinson and Berridge 1993; Mendrek et al. 1998; Kalivas 1995). Tolerance, on the other hand, may provide an animal model for elucidating time-dependent loss of mental and physical energy associated with stimulant withdrawal after multi-day high-dose, compulsive binges (Gawin and Ellinwood 1988; Weiss et al. 1995).
The two dosing regimens for the above stimulants are also associated with distinctive electrophysiological changes in the potency of dopamine (DA) agonists in inhibiting activity of DA neurons in the substantia nigra zona compacta (SNC, which projects primarily to the dorsal striatum) and ventral tegmental area (VTA, which projects to the ventral striatum and prefrontal cortex). In the SNC, for example, while both continuous infusion and intermittent injections lead to a reduced sensitivity of single DA neurons to DA agonists shortly after withdrawal (Kamata and Rebec 1984; Ellinwood and Lee 1983; Lee and Ellinwood 1989), the mechanisms underlying this subsensitivity are different (Pitts et al. 1989, 1993; Lee et al. 1997). For intermittent injections (which lead to phasically high levels of cocaine) an enabling by a D1-dependent mechanism appears to play a key role in the agonist subsensitivity (Pitts et al. 1989, 1993; Lee et al. 1997), whereas a direct change in D2 autoreceptor sensitivity might underlie the subsensitivity following continuous infusion (Lee et al. 1997). In contrast to the SNC, the findings in the VTA are most consistent with autoreceptor subsensitivity (Henry et al. 1989; Lee et al. 1997; White et al. 1995) and normosensitivity (Lee et al. 1997) 1 day after withdrawal from intermittent and continuous regimens, respectively. The differential effects of chronic cocaine treatments on the VTA and SNC may be reflective of their different afferent connections as well as differences in their respective DA receptor populations.
Following a longer withdrawal period (e.g., 7 days), intermittent injections are generally associated with normosensitivity of the SNC and VTA DA neurons to DA agonists (Henry et al. 1989; White et al. 1995; Lee et al. 1997). Continuous infusion is also associated with a normosensitivity of the VTA DA neurons following 7-day withdrawal. However, as we have demonstrated previously, the SNC DA neurons become supersensitive to apomorphine (Ellinwood and Lee 1983; Lee and Ellinwood 1989; Zhang et al. 1992) or quinpirole (Gao et al. 1998) in vivo as well as DA in vitro (Lee et al. 1993). We have proposed that this sensitivity increase in the continuous pretreatment group may represent somatodendritic DA autoreceptor supersensitivity.
Altered somatodendritic DA autoreceptor sensitivity may be manifested by changes in the number of spontaneously active SNC or VTA DA neurons under baseline conditions. With respect to stimulant-induced changes, the VTA autoreceptor subsensitivity after a 1–2-day withdrawal from intermittent injections (Henry et al. 1989; White et al. 1995; Lee et al. 1997) has been associated with an increased number of spontaneously active DA neurons (Henry et al. 1989; White et al. 1995). Conversely, the SNC autoreceptor supersensitivity on day 7 of withdrawal from continuous infusion is associated with a corresponding decrease in the number of active neurons (Gao et al. 1998). Similar decreases in the spontaneous activity may be also observed under other conditions leading to autoreceptor supersensitivity (Bunney and Grace 1978; Gallager et al. 1978). In addition to the number of spontaneously active DA neurons, overall baseline DA neurotransmission may be determined by changes in the bursting pattern of neuronal activity (Gonon 1988). Our recent study (Gao et al. 1998) demonstrates that continuous cocaine infusion reduces VTA bursting 7 days after withdrawal, a finding that, along with SNC autoreceptor supersensitivity, might provide a partial basis for various symptomatology observed in compulsive stimulant abusers in the intermediate (5–10-day) withdrawal phase, a period of high recidivism.
The above changes in the spontaneous activity of DA neurons, regardless of cocaine pretreament or cell body regions, can be normalized by an acute dose of sulpiride (Gao et al. 1998), findings consistent with alterations in D2-dependent mechanism(s). The present experiment was designed to further explore the D2-dependent mechanisms by means of daily injections of apomorphine (D1/D2 agonist), quinpirole (selective D2 agonist), or apomorphine + SCH 39166 (selective D1 antagonist) between withdrawal days 1–5. On day 7 of withdrawal (i.e., 2 days after D1/D2 agonist treatment), we determined the number of spontaneously active DA neurons and their bursting pattern in the SNC and VTA. Our hypothesis was that stimulation of D2 receptors during the early withdrawal phase could negate their changes in sensitivity by day 7, and thus normalize midbrain DA cell firing. In addition to possible underlying mechanisms, the clinical relevance of the findings are discussed.
METHODS
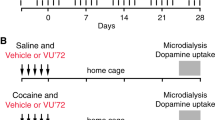
Animals and Pretreatment
Male Sprague-Dawley rats (Charles-River, Raleigh, NC), weighing 300–350 g at the time of recording, were used throughout. Animals were housed two per cage under a 12/12 hour light/dark cycle and food and water were available ad libitum. Following a minimum of 7 days of acclimatization, rats were pretreated for 14 days with one of the three pretreatment regimens: (1) saline injections (2 ml/kg, SC), (2) cocaine injections (40 mg/kg hydrochloride salt, SC, once a day, injected in 2 ml/kg volume), or (3) continuous cocaine infusion (40 mg/kg/d, SC). Implantation and explantation procedures for osmotic minipumps (model 2ML2, Alza Corp., Palo Alto, CA) have been previously described (Joyner et al. 1993). Briefly, rats were anesthetized with methoxyflurane and a small incision was made on the back of skin (the incision site infiltrated with lidocaine), and the subcutaneous connective tissue was separated, forming a pocket. Single minipumps with modified flow modulators were inserted into this pocket and the wound closed with surgical clips. The pumps were removed 2 weeks later using a similar surgical procedure. For intermittent injections, the injection site was rotated daily throughout the 14-day period in order to reduce skin inflammation associated with cocaine injection. Between withdrawal days 1 and 5, rats in each pretreatment groups were injected with single daily subcutaneous injections of one of the following: (1) 2 ml/kg saline, (2) 100 μg/kg apomorphine, (3) 0.5 mg/kg SCH 39166 followed 30 minutes later by 100 μg/kg apomorphine, (4) 30 μg/kg quinpirole, or (5) 100 μg/kg quinpirole. The low doses of apomorphine and quinpirole were chosen for selective stimulation of DA autoreceptors, which are generally agreed to be more sensitive to agonists than the postsynaptic receptors (Nickolson 1981; Skirboll et al. 1979; Jeziorski and White 1989; Lee and Ellinwood 1989). Similar “low-dose” strategies have been previously used to examine effects of repeated autoreceptor stimulation on DA functions (e.g., Mereu et al. 1987; Jeziorski and White 1989).
Single-Unit Procedure
Seven days after cocaine withdrawal (i.e., 2 days after the last D1/D2 drug injections), rats were anesthetized with chloral hydrate (400 mg/kg, IP) and their jugular vein catheterized for anesthetic supplements. The animals were mounted on Kopf stereotaxic apparatus. The skull was exposed and a small burr hole was drilled in the area overlying either the SNC or VTA. Body temperature of the rats was maintained at 36–38°C using a temperature control pad.
Extracellular single-unit recordings were made using glass-coated tungsten electrodes (Frederick Haer, Brunswick, ME; impedance 10 MΩ at 1000 Hz). The number of spontaneously active SNC or VTA neurons exhibiting electrophysiological characteristic of DA neurons was counted by lowering the electrode from 6.5 to 8.5 mm below the brain surface (Chiodo and Bunney 1983; Gao et al. 1998). Nine electrode tracks, each separated by 0.2 mm were passed at predetermined coordinates (3.1–3.5 mm anterior to lambda, 1.5–1.9 and 0.4–0.8 mm lateral to the midline for SNC and VTA, respectively). The sequence of the electrode tracks was kept constant from animal to animal, and a new electrode was used for each animal. In addition to the number of spontaneously active neurons, the baseline firing rate and bursting pattern of each neuron were determined based on the analysis of 500 consecutive spikes.
Putative DA neurons were identified by previously established criteria (Bunney et al. 1973): (1) a long action potential (>2.5 ms) with a distinct “notch” in the initial rising phase; (2) slow, burst or regular firing pattern (up to 9 spikes/s); and (3) low-pitched sound on an audio monitor. The bursting pattern of individual neurons was determined as previously described (Grace and Bunney 1984). A burst onset was defined as an occurrence of two spikes with an interspike interval of less than or equal to 80 ms, thereafter an interval greater than 160 ms denoted a burst termination. For each neuron, we determined: (1) average number of spikes per burst; (2) total number of bursts; and (3) percentage of the 500 collected spikes that occur within bursts.
The last recording site was electrolytically lesioned by passing a 10-μA current through the recording electrode for 30 seconds. The animals were then perfused transcardially with 0.9% saline followed by 10% formalin under an overdose of chloral hydrate. Serial 50-μm sections of the brain were stained with Cresyl violet, and the location of recorded neurons extrapolated from the position of the lesion site (i.e., the last recorded neuron).
Drugs
(-)Cocaine, (-)quinpirole and R(-)apomorphine (HCl salts) were obtained from RBI (Natick, MA). SCH 39166 was a gift from Dr. Allen Barnett, Schering-Plough (Kenilworth, NJ). Drugs were dissolved in distilled water or sterile saline, and freshly prepared daily.
Data Analysis
The number of spontaneously active SNC and VTA DA neurons were compared using a one-way analysis of variance (ANOVA; saline, intermittent injections and continuous infusion, each group with post-cocaine injections with saline, apomorphine, apomorphine + SCH 39916, or low/high dose quinpirole). For the baseline firing rates and bursting indices, a single set of values for each animal was first derived by averaging results from individual neurons; these values were subsequently used to compare pretreatment groups by a one-way ANOVA as before. Post-hoc comparisons of individual means were accomplished using Dunnett's test with the saline/saline group as control. For all tests, p < 0.05 was considered statistically significant; all data are presented as mean ± SEM.
RESULTS
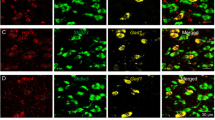
All recordings were taken on withdrawal day 7 and neurons exhibited electrophysiological characteristics typical of putative DA neurons. Furthermore, these neurons were found, as estimated from the lesion at the last recording site, 6.5 to 8.5 mm below the surface of the brain, and between 2.96 and 3.70 mm anterior to the interaural line (Paxinos and Watson 1986). Correct medio-lateral positioning of the SNC and VTA sampling tracks were also verified histologically (1.4–2.1 mm and 0.4–1.2 mm lateral, respectively).
Effects of Day 1–5 Treatment on the Number of Spontaneously Active Neurons
There was an effect of treatment (saline, intermittent, or continuous cocaine) on the number of spontaneously active DA neurons in the SNC (F[14,122] = 7.870, p < .001; Figure 1A ). Following a 7-day withdrawal, continuous infusion and intermittent injections of cocaine led to reduced and normal number of DA neurons in the SNC, respectively. Post-cocaine injections of the mixed DA agonist apomorphine (100 μg/kg, SC) reversed the reduced number of active SNC DA neurons in the continuous infusion group. When co-administered with apomorphine, SCH 39166 (0.5 mg/kg, SC), a selective D1 antagonist, did not affect the apomorphine-induced reversal, thus precluding a D1 mechanism and suggesting a likely involvement of D2 receptors in the apomorphine effect. Consistent with this hypothesis, daily injections of a selective D2 agonist (quinpirole) during the early withdrawal period reversed the day 7 reduction in the number of active SNC DA neurons. The quinpirole effect was dose-dependent as 100 μg/kg, but not 30 μg/kg, was able to show this reversal. In contrast to their effects in the continuous infusion group, these DA agents had minimal effect in the SNC for either the saline or intermittent cocaine injection groups.
Effects of post-cocaine DA agonists given on withdrawal days 1–5 on the number of spontaneously active putative DA neurons per electrode track in the SNC (A) and VTA (B). Saline (2 ml/kg); Apo, apomorphine (100 μg/kg); Apo + SCH, apomorphine (100 μg/kg) + SCH 39166 (0.5 mg/kg); and Quin-Lo and -Hi, quinpirole (30 μg/kg and 100 μg/kg, respectively). Number of animals (Control/Infusion/Injection): Saline = 13/18/11; Apo = 5/7/7; Apo + SCH = 6/6/8; Quin-Lo = 7/6/7; and Quin-Hi = 6/8/8 for the SNC; 14/18/12, 6/6/8, 6/6/7, 7/7/7, and 6/7/7, respectively, for the VTA. *p < 0.05 and **p < .01, compared to Control/Saline group (patterned bar), Dunnett's test.
There was also an effect of treatment on the number of spontaneously active DA neurons in the VTA (F[14,123] = 7.270, p < .001; Figure 1B). In contrast to the SNC, continuous cocaine infusion induced minimal change in the number of active VTA neurons following 7-day withdrawal. However, intermittent injections led to an increase in this index, and this increase was reversed by five daily injections of low-dose apomorphine during withdrawal. Indeed, the apomorphine injections not only normalized the number of active neurons but in fact decreased it below the levels observed in the saline or continuous infusion group. Co-administration of SCH 39166 again failed to alter the effect of apomorphine on the VTA spontaneous activity. Also consistent with an involvement of a D2-dependent mechanism was the finding that the intermittent group injected with the higher dose of quinpirole (100 μg/kg, SC) exhibited a reduced number of spontaneously active DA neurons compared to the control and infusion groups. The quinpirole effect was dose-dependent as the lower dose of 30 μg/kg only returned firing to control levels of the spontaneous activity. Apomorphine, either alone or in combination with SCH 39166, and quinpirole did not exert significant effects on the number of active VTA DA neurons in either the saline or continuous cocaine infusion groups.
Effects of Day 1–5 Treatment on Burst Pattern
Neither continuous infusion nor intermittent injections of cocaine altered the bursting pattern of the SNC DA neurons on day 7 of withdrawal (Figure 2 ). Furthermore, apomorphine, apomorphine + SCH 39166, and both doses of quinpirole, when injected between cocaine withdrawal days 1 and 5, exerted no clear, consistent effects on day 7 SNC bursting in any of the groups. The effect of treatment on the total number of bursts (F[14,121] = 0.404, p > .16; Figure 2A), the percentage of spikes in bursts (F[14,121] = 0.894, p > .56; Figure 2B) and the mean number of spikes per burst (F[14,121] = 0.852, p > .61; Figure 2C) were all nonsignificant.
Effects of post-cocaine DA agonists given on withdrawal days 1–5 on day 7 bursting activity in putative SNC DA neurons. (A) Total number of bursts; (B) mean number of spikes per burst; and (C) percentage of recorded spikes that occurred in bursts. No significant treatment effects were observed for any of the indices. See Figure 1 legend for group identification labels and number of animals.
Significant group differences were, however, observed in the VTA (Figure 3 ) for the total number of bursts (F[14,115] = 3.108, p < .001; Figure 3A) and the percentage of spikes found in bursts (F[14,115] = 2.047), p < .022; Figure 3C) but not for the mean number of spikes per burst (F[14,115] = 1.325, p > .20; Figure 3B). Continuous cocaine infusion reduced bursting in the VTA DA neurons on day 7 of withdrawal; post-cocaine injections between days 1 and 5 of withdrawal reversed this bursting reduction. SCH 39166, when co-administered with apomorphine, did not block the reversing/preventing effect of apomorphine in the continuous infusion group. Similarly, quinpirole, at 100 but not 30 μg/kg, prevented the reduced bursting in the continuous cocaine infusion group. The three drugs had no significant effects on the saline or intermittent cocaine injection group (see Figure 3).
Effects of post-cocaine DA agonists given on withdrawal days 1–5 on day 7 bursting activity in putative VTA DA neurons. (A) total number of bursts; (B) mean number of spikes per brust; and (C) percentage of recorded spikes that occurred in bursts. See Figure 1 legend for group identification labels and number of animals. *p < 0.05, **p < .01, compared to Control/Saline group (patterned bar), Dunnett's test.
Effect of Day 1–5 Treatment on Baseline Firing Rates
Daily injections of apomorphine, apomorphine + SCH39166 or quinpirole on withdrawal days 1 to 5 had no effect on day 7 spontaneous firing rates of SNC (F[14,121] = 0.736, p > .73) or VTA (F[14,97] = 0.506, p > .92) DA neurons in any of the experimental groups. All groups in both the SNC and VTA exhibited mean firing rates of approximately four spikes per second.
DISCUSSION
The present study confirms our previous findings that intermittent and continuous cocaine pretreatment regimens induce distinct changes in the baseline activity of the SNC and VTA DA neurons (Gao et al. 1998). Thus, on day 7 of withdrawal from continuous cocaine infusion, we found reduced number of spontaneously active DA neurons in the SNC and reduced bursting in the VTA. Withdrawal from intermittent injections, on the other hand, was associated with increased numbers of spontaneously active DA neurons in the VTA with no other detectable changes in either the SNC or VTA. The present study has extended these previous findings by showing that D2 agonists administered on withdrawal days 1–5 can reverse the day-7 changes in the activity of midbrain DA neurons. Taken together with our previous finding that acute sulpiride could also reverse these changes (Gao et al. 1998), we suggest that D2 mechanisms play an important role in cocaine-induced alterations in the spontaneous activity of DA neurons during the first week of withdrawal.
Changes Following Continuous Cocaine Infusion
In the SNC, stimulation of DA receptors with “autoreceptor-selective” doses of apomorphine or quinpirole (Nickolson 1981; Skirboll et al. 1979; Jeziorski and White 1989; Lee and Ellinwood 1989) between withdrawal days 1 and 5 reverses the reductions in the number of active DA neurons. Furthermore, the normalization of spontaneous firing activity seen with apomorphine is not inhibited by the co-administration of the D1 antagonist SCH 39166. These findings suggest that the apomorphine-induced normalization is mediated by a D2- but not a D1-dependent mechanism; the simplest explanation might be that stimulation of DA autoreceptors during the time of their dynamic sensitivity increase (i.e., day 1 subsensitivity evolving into day 7 supersensitivity; Ellinwood and Lee 1983; Zhang et al. 1992; Gao et al. 1998), prevents the supersensitivity development via competing desensitization. It is interesting to note that distinct changes in autoreceptor sensitivity and number of spontaneously firing neurons are not associated with a change in bursting pattern. These findings are consistent with previous data demonstrating that bursting activity in SNC DA neurons may be more directly related to mono- or poly-synaptic excitatory afferent inputs (e.g., subthalamic nucleus, pedunculopontine nucleus, prefrontal cortex, vide infra) rather than DA autoreceptor sensitivity per se (for a review, see Overton and Clark 1997).
In the VTA, continuous cocaine infusion had no effect on the number of spontaneously active DA neurons on withdrawal day 7 but selectively decreased bursting of these neurons (Gao et al. 1998; the present study). Considering neither the sensitivity to DA agonists nor the number of spontaneously active neurons (Lee and Ellinwood 1989; Gao et al. 1998; the present study) are changed in VTA neurons, a possible role of direct somatodendritic autoreceptor sensitivity changes in this baseline bursting change appears unlikely. We have therefore postulated that the decreased VTA bursting might be mediated by changes in either terminal D2 autoreceptors or postsynaptic D2 receptors in another nucleus which may trans-synaptically regulate the activity levels of afferent pathways to the VTA (Gao et al. 1998). Several studies have shown that stimulation and cooling of the prefrontal cortex increases and abolishes the burst firings in the VTA, respectively (Charlety et al. 1991; Gariano and Groves 1988; Svensson and Tung 1989; see Overton and Clark 1997, for review). In addition to direct D2 changes within the prefrontal cortex, those in DA heteroceptors in the VTA (albeit largely of the D1 class), which modulate local release of both glutamate (Kalivas and Duffy 1998) and GABA (Cameron and Williams 1993), could also alter VTA bursting activity (for a review, see Overton and Clark 1997). Via a yet-to-be-determined mechanism, repeated administration of low doses of D2 agonists might, reverse the day 7 bursting changes by “normalizing” the prefrontal excitatory influence on VTA DA neurons.
Changes Following Intermittent Cocaine Injections
Under our experimental conditions, 7-day withdrawal from intermittent cocaine injections has no effect on SNC DA neurons but leads to a selective increase in the number of spontaneously active DA neurons in the VTA without alterations in their bursting pattern or quinpirole sensitivity (Gao et al. 1998; the present study). These changes are readily reversed by an acute injection of sulpiride (a D2-selective antagonist; Gao et al. 1998). The present study demonstrates that five daily post-cocaine injections of low doses of apomorphine or quinpirole not only normalize the altered number of VTA neurons, as acute sulpiride does, but also reduces it below the levels observed in controls. The apomorphine-induced reversal is not antagonized by SCH 39166 and, again, the quinpirole effect is dose-dependent, suggesting a D2 mechanism of action of this early withdrawal treatment. Beyond an involvement of a D2 mechanism, the exact mechanism underlying the normalization “overshoot” (i.e., significant decrease compared to controls) is not clear. It is also noted that, in contrast to our findings (Gao et al. 1998; the present study), Ackerman and White (1992) have reported decreased spontaneous activity of VTA neurons after 10–14-day withdrawal from intermittent cocaine injections (10 mg/kg IP twice daily × 14 days). We have previously suggested that these discrepancies between the two laboratories might be secondary to differences in cocaine doses or withdrawal duration (Gao et al. 1998). Resolution of the above issues awaits further characterization of the time-course and localization of baseline DA unit activity alterations following cocaine withdrawal.
The precise mechanisms for all significant reversals effected by the post-cocaine D2 treatment in the present study need to be further explored. On the other hand, the finding that the same agonists exert minimal effects in control animals suggests that the modifications associated with the 5-day treatments are likely to interact with specific changes induced by cocaine pretreatments. Therefore, detailed characterization of changes observable during the first week of withdrawal (e.g., days 1–7) from cocaine pretreatment may facilitate elucidation of the mechanistic bases for the D2 efficacy. Using single-unit recording and voltammetry techniques (e.g., Lee et al. 1998), we are currently determining the full time-course and localization of brain areas that might be critical for the various baseline DA unit-activity alterations following cocaine withdrawal. With respect to the lack of post-cocaine treatment effects on control animals, other investigators have also found that multiple injections of “autoreceptor-selective” doses of apomorphine apparently fails to down-regulate D2 receptors in normal animals, a finding that has been attributed to the existence of spare autoreceptors (Mereu et al. 1987; Jeziorski and White 1989).
In accordance with the generally accepted view (Bunney and Grace 1978; for additional references, see Dai and Tepper 1998), we have interpreted the present changes in the number of DA neurons per track as reflecting those in the number of neurons spontaneously generating action potentials (i.e., some neurons are normally silent). On the other hand, Dai and Tepper (1998) have recently suggested that virtually all SNC DA neurons (>98%) are spontaneously active, even in anesthetized animals. According to these investigators, changes in the number of active neurons per track following D2 blockade are secondary to such factors as increased firing rates or decreased electrotonic lengths of recorded neurons, which would spuriously increase the likelihood of finding slow-firing neurons or those that are distant from the recording electrode. Possible implication of this report for the present results is not yet clear. It is, however, pointed out that the baseline firing rates were not altered in any pretreatment groups in the present study. Most importantly, regardless of whether or not the prevalent viewpoint needs to be revised, the main conclusion of the present study remains valid. That is, because it is highly unlikely that the above “spurious” factors would differentially affect different pretreatment groups, continuous and intermittent administration of cocaine lead to characteristic alterations in the baseline activity. Moreover, acute D2 antagonism by sulpiride (Gao et al. 1998) or 5-day D2 stimulation can specifically reverse these changes. Direct antidromic stimulation of DA neurons during 9-track population sampling (Dai and Tepper 1998) from cocaine-pretreated animals might provide a further clarification.
Clinical Relevance
Cocaine or other stimulant abuse in its most severe form is characterized by a binging pattern of administration (first described by Kramer et al. 1967), in which high doses of the drug (often high enough to be lethal in naive individuals) are either injected or smoked over multiple days (Gawin and Ellinwood 1988; Gawin et al. 1994). During these runs, high, sustained drug levels are often maintained for, with adequate supply, 18–24 h/d. Behaviorally, compulsive cocaine “bingers” often exhibit simultaneous sensitization and tolerance to different effects of the drug (e.g., stereotyped thought pattern/paranoia and cocaine “high,” respectively); these “deficits” subside with differential time courses during abstinence/withdrawal (for reviews, see Gawin et al. 1994; Gold et al. 1992). We have recently suggested (Lee et al. 1997) that examination of sensitization or tolerance in animals without the other may provide inadequate information on critical mechanisms associated with compulsive cocaine (stimulant) abuse. Thus, our approach of directly comparing and contrasting two opposing dosing regimens under identical experimental conditions are aimed at facilitating identification of such mechanisms.
The withdrawal from stimulant binges are associated with sustained anergia and dysphoria over a period of 7–10 days (Gawin and Ellinwood 1988). We have hypothesized (Gao et al. 1998) that the reduced number of spontaneously active DA neurons in the SNC and reduced bursting in the VTA following continuous infusion might partially underlie symptoms associated with the intermediate withdrawal phase following compulsive cocaine binges (e.g., loss of physical/mental energy, anhedonia, etc.). These symptoms may contribute to the high rate of recidivism associated with such abuse (Gawin and Ellinwood 1988). The first week of withdrawal might therefore provide a time window, during which a short-term treatment with selective D2 agonists might reverse the reduced DA baseline activity and thus offer potential treatment for the intermediate withdrawal phase symptoms. Such efficacy is, in turn, expected to aid in achieving a long-term cocaine abstinence. Indeed, the DA agonist bromocriptine has been reported to be efficacious in treating this anergic, intermediate withdrawal phase (Giannini et al. 1989). It should be noted, however, that these D2 agonists could be counter-productive when introduced in later phases of withdrawal, as they may serve as discriminative (cocaine-like) stimuli that trigger renewed compulsive use (Kleber 1995). Indeed, Self et al. (1996) have shown that D2-like agonists can trigger relapse behavior in a rat model of cocaine seeking. These investigators have also reported that D1-like agonists, given prior to cocaine priming, could block the cocaine-seeking behavior. This efficacy of D1 manipulation is in contrast to the inability of SCH 39166 to modify chronic apomorphine effects in the present study. However, it should be noted that the D1 blockade of cocaine priming is an “immediate” (within hours) effect of acute injections. We, on the other hand, have examined a “delayed” modulation (2 days after the last inection) following chronic injections (5 days).
SUMMARY
The present study extends our previous work which showed that D2 receptors are likely to be involved in the altered number of spontaneously active neurons and their bursting pattern 7 days after intermittent cocaine injections and continuous infusion. Thus, these day-7 changes can be reversed by an acute blockade of D2 receptors on day 7, on one hand (Gao et al. 1998), and chronic stimulation (e.g., desensitization) of D2 receptors between days 1 and 5, on the other (the present study). Direct comparison and contrast of intermittent and continuous cocaine pretreatments in animals might provide an experimental means for identifying a set of alterations that can be manipulated for formulating specific therapeutic strategies for compulsive cocaine abuse. We also suggest that the overall planning of individual therapeutic strategies may be further facilitated by addressing the dynamic nature of the stimulant withdrawal phases and associated mechanisms. Achieving a long-term abstinence in repeated, compulsive cocaine abusers may require careful evaluation of their abuse history and current withdrawal status. In addition, appropriate adjustment in therapeutic agents and regimens (e.g., short-term treatment with low-dose D2 agonist with supplemental D1 agonist as needed to combat cocaine craving) may facilitate long-term abstinence from compulsive cocaine abuse.
References
Ackerman JM, White FJ . (1992): Decreased activity of rat A10 dopamine neurons following withdrawal from repeated cocaine. Eur J Pharmacol 218: 171–173
Bunney BS, Aghajanian GK, Roth RH . (1973): Comparison of effects of L-DOPA, amphetamine and apomorphine on firing rate of rat dopaminergic neurons. Nature 245: 123–125
Bunney BS, Grace AA . (1978): Acute and chronic haloperidol treatment: Comparison of effects on nigral dopaminergic cell activity. Life Sci 23: 1715–1727
Cameron DL, Williams JT . (1993): Dopamine D1 receptors facilitate transmitter release. Nature 366: 344–347
Charlety PJ, Grenhoff J, Chergui K, De la Chapelle B, Buda M, Svensson TH, Chouvet G . (1991): Burst firing of mesencephalic dopamine neurons is inhibited by somatodendritic application of kynurenate. Acta Phys Scand 142: 105–112
Chiodo LA, Bunney BS . (1983): Typical and atypical neuroleptics: Differential effects of chronic administration on the activity of A9 and A10 midbrain dopaminergic neurons. J Neurosci 3: 1607–1619
Dai M, Tepper JM . (1998): Do silent dopaminergic neurons exist in rat substantia nigra in vivo? Neuroscience 85: 1089–1099
Ellinwood EH Jr, Lee TH . (1983): Effect of continuous systematic infusion of d-amphetamine on the sensitivity of nigral dopamine cells to apomorphine inhibition of firing rate. Brain Res 273: 379–383
Gallager DW, Pert A, Bunney WE Jr . (1978): Haloperidol-induced presynaptic dopamine supersensitivity is blocked by chronic lithium. Nature 273: 309–312
Gao WY, Lee TH, King GR, Ellinwood EH . (1998): Alterations in baseline activity and quinpirole sensitivity in putative dopamine neurons in the substantia nigra and ventral tegmental area after withdrawal from cocaine pretreatment. Neuropsychopharmacology 18: 222–232
Gariano RF, Groves PM . (1988): Burst firing induced in midbrain dopamine neurons by stimulation of the medial prefrontal and anterior cingulate cortices. Brain Res 462: 194–198
Gawin FH, Ellinwood EH Jr . (1988): Cocaine and other stimulants: Actions, abuse and treatments. N Engl J Med 318: 1173–1182
Gawin FH, Khalsa H, Ellinwood EH Jr . (1994): Stimulants. In Galanter M, Kleber HD (eds), Textbook of Substance Abuse. Washington, D.C., American Psychiatric Press, pp 111–139
Giannini AJ, Folts DJ, Feather JN, Sullivan BS . (1989): Bromocriptine and amantadine in cocaine detoxification. Psychiatry Res 29: 11–16
Gold MS, Miller S, Jonas JN . (1992): Cocaine (and crack): Neurobiology. In Lowinson JH, Ruiz P, Millman RB, Langrod JG (eds), Substance Abuse: A Comprehensive Textbook. Baltimore, MD, Williams and Wilkins, pp 222–235
Gonon FG . (1988): Nonlinear relationship between impulse flow and dopamine released by rat midbrain dopaminergic neurons as studied by in vivo electrochemistry. Neuroscience 24: 19–28
Grace AA, Bunney BS . (1984): The control of firing pattern in nigra dopamine neurons: Burst firing. J Neurosci 4: 2877–2890
Henry DJ, Greene MA, White FJ . (1989): Electrophysiological effect of cocaine in the mesoaccumbens dopamine system: Repeated administration. J Pharmacol Exp Ther 251: 833–839
Inada T, Polk K, Purser C, Hume A, Hoskins B, Ho IK, Rockhold RW . (1992): Behavioral and neurochemical effects of continuous infusion of cocaine in rats. Neuropharmacology 31: 701–708
Jeziorski M, White FJ . (1989): Dopamine agonists at repeated “autoreceptor selective” doses: Effects upon the sensitivity of A10 dopamine neurons. Synapse 4: 267–280
Joyner C, King GR, Lee TH, Ellinwood EH Jr . (1993): A technique for the continuous infusion of high doses of cocaine by osmotic minipump. Pharmacol Biochem Behav 44: 971–973
Kalivas PW . (1995): Neural basis of behavioral sensitization to cocaine. In Hammer RP Jr (ed), The Neurobiology of Cocaine: Cellular and Molecular Mechanisms. Boca Raton, FL, CRC Press, pp 81–98
Kalivas PW, Duffy P . (1998): Repeated cocaine administration alters extracellular glutamate in the ventral tegmental area. J Neurochem 70: 1497–1502
Kamata K, Rebec GV . (1984): Nigral dopaminergic neurons: Differential sensitivity to apomorphine following long-term treatment with low and high doses of amphetamine. Brain Res 321: 147–150
Kilbey MM, Ellinwood EH Jr . (1977): Administration of stimulant drugs: Response modification. In Ellinwood EH Jr, Kilbey MM (eds), Advances in Behavioral Biology: Cocaine and Other Stimulants. New York, Plenum Press, pp 409–429
King GR, Joyner C, Lee TH, Kuhn C, Ellinwood EH Jr . (1992): Intermittent and continuous cocaine administration: Residual behavioral states during withdrawal. Pharmacol Biochem Behav 43: 243–248
Kleber HD . (1995): Pharmacology, current and potential for the treatment of cocaine dependence. Clin Neuropharmacol 18[Suppl 1]:s96–s109
Kramer JC, Fischman VS, Littlefield DC . (1967): Amphetamine abuse: Pattern and effects of high doses taken intravenously. JAMA 201: 305
Lau CE, Imam A, Fang M, Falk JL . (1991): Acute effects of cocaine on spontaneous and discriminative motor functions: Relation to route of administration and pharmacokinetics. J Pharmacol Exper Ther 257: 444–456
Lee TH, Ellinwood EH Jr . (1989): Time-dependent changes in the sensitivity of dopamine neurons to low doses of apomorphine following amphetamine infusion. Brain Res 483: 17–29
Lee TH, Ellinwood EH, Zhang H . (1993): In vitro extracellular recording from nigra dopamine neurons following continuous d-amphetamine infusion. Eur J Pharmacol 232: 125–129
Lee TH, Gao W-Y, Ellinwood EH . (1997): Differential effects of SCH 23390 on the apomorphine subsensitivity in the substantia nigra and ventral tegmental area 1 day following withdrawal from continuous or intermittent cocaine pretreatment. Brain Res 744: 293–301
Lee TH, Gee KR, Ellinwood EH, Seidler FJ . (1998): Altered cocaine potency in the nucleus accumbens following 7 day withdrawal from intermittent but not continuous treatment: Voltammetric assessment of dopamine uptake in the rat. Psychopharmacology 137: 303–310
Mendrek A, Blaha CD, Phillips AG . (1998): Pre-exposure of rats to amphetamine sensitizes self-administration of this drug under a progressive ratio schedule. Psychopharmacology 135: 416–422
Mereu G, Hu X-T, Wang RY, Westfall TC, Gessa GL . (1987): Failure of subchronic lisuride to modify A10 dopamine autoreceptor's sensitivity. Brain Res 408: 210–214
Nickolson VJ . (1981): Detailed analysis of the effects of apomorphine and d-amphetamine on spontaneous locomotor behaviour in rats as measured in a TV-based, automated open-field system. Eur J Pharm 72: 45–56
Overton PG, Clark D . (1997): Burst firing in midbrain dopaminergic neurons. Brain Res Rev 25: 312–334
Paxinos G, Watson C . (1986): The Rat Brain in Stereotaxic Coordinates, 2nd ed. San Diego, Academic Press
Pitts DK, Freeman AS, Kelland MD, Chiodo LA . (1989): Repeated amphetamine, reduced dopamine neuronal responsiveness to apomorphine but not quinpirole. Eur J Pharmacol 162: 167–171
Pitts DK, Kelland MD, Freeman AS, Chiodo LA . (1993): Repeated amphetamine administration: Role of forebrain in reduced responsiveness of nigrostriatal dopamine neurons to dopamine agonists. J Pharmacol Exp Ther 264: 616–621
Post RM, Contel NR . (1983): Human and animal studies of cocaine: Implications for development of behavioral pathology. In Creese I (ed), Stimulants: Neurochemical, Behavioral, and Clinical Perspectives. New York, Raven Press, pp 169–203
Post RM, Rose H . (1976): Increasing effects of repetitive cocaine administration in the rat. Nature 260: 731–732
Reith MEA, Benuck M, Lajtha A . (1987): Cocaine disposition in the brain after continuous or intermittent treatment and locomotor stimulation in mice. J Pharmacol Exp Ther 243: 281–287
Robinson TE, Berridge KC . (1993): The neural basis of drug craving: An incentive-sensitization theory of addiction. Brain Res Rev 18: 247–291
Self DW, Barnhart WJ, Lehman DA, Nestler EJ . (1996): Opposite modulation of cocaine-seeking behavior by D1- and D2-like dopamine receptor agonists. Science 271: 1586–1589
Skirboll LR, Grace AA, Bunney BS . (1979): Dopamine auto- and postsynaptic receptors: Electrophysiological evidence for differential sensitivity to dopamine agonists. Science 206: 80–82
Svensson TH, Tung C-S . (1989): Local cooling of prefrontal cortex induces pacemaker-like firing of dopamine neurons in rat ventral tegmental area in vivo. Acta Physiol Scand 136: 135–136
Weiss F, Parsons LH, Markou A . (1995): Neurochemistry of cocaine withdrawal. In Hammer RP Jr (ed), The Neurobiology of Cocaine: Cellular and Molecular Mechanisms. Boca Raton, FL, CRC Press, pp 163–181
White FJ, Hu X-T, Henry DJ, Zhang X-F . (1995): Neurophysiological alterations in the mesocorticolimbic dopamine system with repeated cocaine administration. In Hammer RP Jr (ed), The Neurobiology of Cocaine: Cellular and Molecular Mechanisms. Boca Raton, FL, CRC Press, pp 99–119
Zhang H, Lee TH, Ellinwood EH Jr . (1992): The progressive changes of neuronal activities of the nigral dopaminergic neurons upon withdrawal from continuous infusion of cocaine. Brain Res 594: 315–318
Acknowledgements
Supported by National Institute on Drug Abuse (DA-06519 to THL and DA-10327 to EHE) and Duke Small Grant Program. We thank Dr. Allen Barnett for a gift of SCH 39166 and Zhiping Xiong and Scott Douglas for technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, T., Gao, WY., Davidson, C. et al. Altered Activity of Midbrain Dopamine Neurons Following 7-Day Withdrawal from Chronic Cocaine Abuse is Normalized by D2 Receptor Stimulation During the Early Withdrawal Phase. Neuropsychopharmacol 21, 127–136 (1999). https://doi.org/10.1016/S0893-133X(99)00011-1
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1016/S0893-133X(99)00011-1
Keywords
This article is cited by
-
Dopamine and addiction: what have we learned from 40 years of research
Journal of Neural Transmission (2019)
-
Animal models and treatments for addiction and depression co-morbidity
Neurotoxicity Research (2007)