Abstract
The binding of [125I]p-iodoclonidine to alpha-2, and/or [125I]iodopindolol to beta-1 and beta-2 adrenoceptors was measured in right prefrontal cortex (Brodmann's area 10) and right hippocampus from subjects with DSM-III-R diagnoses of major depression (n = 15) or schizophrenia (n = 8) as well as from control subjects (n = 20). No significant differences between study groups were observed in binding to alpha-2 adrenoceptors in any of the six layers of prefrontal cortex or in any of the hippocampal fields. Likewise, there were no significant differences in beta-1 or beta-2 adrenoceptor binding in any of the hippocampal fields between control and major depressive subjects. In contrast, binding to beta-1 adrenoceptors, but not beta-2 adrenoceptors, was significantly lower (−13 to −27%) in most hippocampal fields of schizophrenic subjects as compared to control subjects or to major depressives. Alterations in beta-1 adrenoceptor binding in the hippocampus of schizophrenics provide further evidence for a role of central noradrenergic neurons in the neurochemical pathology of schizophrenia.
Similar content being viewed by others
Main
The central noradrenergic system serves a global function of neural modulation, controlling vigilance, attention, and the sleep–wake cycle and contributing to learning and memory processes. This system is also robustly activated by stress (Aston-Jones et al. 1991). Disruptions of attention, memory, and sleep are behavioral characteristics of major depression. Therefore, we could hypothesize that abnormal noradrenergic function could be responsible, at least in part, for these symptoms. The putative role that stress plays in depressive disorders and the ability of long-term stress to deplete norepinephrine lends credence to the hypothesis that there is pathological involvement of the central noradrenergic system in depression (Prange 1964; Schildkraut 1965; Ordway et al. 1994b; Klimek et al. 1997).
Studies designed to examine the noradrenergic hypothesis of affective disorders have been diverse and sometimes inconsistent (Prange 1964; Schildkraut 1965; Waldmeier 1981; Lake et al. 1982; De Paermentier et al. 1990; Ferrier and Perry, 1992; Meana et al. 1992; Gonzalez et al. 1994). Nevertheless, the majority of such reports support the idea that there is an abnormality of central catecholaminergic transmission in major depression (Prange 1964; Schildkraut 1965; Waldmeier 1981; Lake et al. 1982; Meana et al. 1992; Callado et al. 1998). Recently, Ordway et al. (1994a) reported elevated levels of tyrosine hydroxylase, the rate-limiting enzyme in the biosynthesis of norepinephrine, in the locus coeruleus, a major region of noradrenergic neuronal cell bodies, from victims of suicide. This finding has been confirmed in subjects diagnosed with major depression relative to psychiatrically normal control subjects (Zhu et al. 1995). Tyrosine hydroxylase in the locus coeruleus is also up-regulated in response to depletion of norepinephrine in rats (Melia et al. 1992) and in response to repeated stress (Melia and Duman 1991; Melia et al. 1992). Furthermore, Klimek et al. (1997) reported decreased binding of [3H]nisoxetine to norepinephrine transporters in the locus coeruleus in major depression. This latter finding may also reflect a norepinephrine deficiency, given that these transporters down-regulate in rats following treatment with norepinephrine-depleting drugs (Lee et al. 1983). Thus, up-regulation of tyrosine hydroxylase and down-regulation of the norepinephrine transporter observed in postmortem studies are findings consistent with the hypothesis of a synaptic deficiency of norepinephrine in major depression.
Efferents of the locus coeruleus constitute two major ascending fiber systems; the dorsal noradrenergic bundle and the rostral limb of the dorsal periventricular pathway, that innervate subcortical limbic regions, such as the hippocampus, as well as most of the cerebral cortex. If a deficiency of norepinephrine exists in the locus coeruleus in major depression, then we would speculate that receptors for norepinephrine in projection areas of the locus coeruleus might be up-regulated in response. Numerous researchers have investigated the possibility of altered noradrenergic receptor densities in cortical areas over the past two decades, and the results have been inconclusive (Mann et al. 1986; Meana and Garcia-Sevilla 1987; Biegon and Israeli 1988; Arango et al. 1990; De Paermentier et al. 1990; Meana et al. 1992; Arango et al. 1993; Gonzalez et al. 1994; Callado et al. 1998). However, few of these studies have utilized tissue from subjects with confirmed diagnoses of major depression at the time of death, and fewer still have utilized control subjects who were confirmed as having no psychiatric illness prior to death.
In addition to a group of major depressives, we measured in the present study noradrenergic receptors in the hippocampus from subjects with another major psychiatric disorder; that is, schizophrenia. Schizophrenia was of particular interest, given evidence implicating a potential role of norepinephrine in the pathophysiology of this disorder. A disruption of the activity of the noradrenergic dorsal bundle from locus coeruleus to the forebrain limbic system could be a possible contributor to the schizophrenic disturbance (see Hornykiewicz 1986; Weinberger et al. 1983), given that activity of the dorsal bundle of the locus coeruleus normally serves to screen the incoming sensory stimuli, filtering out and discarding information irrelevant to the task at hand (Archer et al. 1982; Mason 1981). Evidence that norepinephrine regulates dopamine-induced behaviors in laboratory animals (Mason 1981; Plaznik et al. 1982) provides a potential link of norepinephrine to dopaminergic dysfunction in schizophrenia. Interestingly, elevated norepinephrine output has been observed in schizophrenic patients (Lake et al. 1980; Sternberg et al. 1981; Hornykiewicz 1982, 1986; Van Kammen and Antelman 1984).
In this study, we measured alpha-2, beta-1, and beta-2 adrenoceptors autoradiographically in the prefrontal cortex and/or hippocampal formation from subjects with Axis I diagnoses of major depression or schizophrenia relative to control subjects who had no Axis I diagnoses (confirmed by psychiatric autopsy) and control subjects with no reported history of psychiatric illness and no psychiatric medications. Most of the psychiatric subjects in this study died as a result of suicide; whereas, control subjects died of natural or accidental causes.
MATERIALS AND METHODS
Tissue Material
Human brains were obtained from subjects at the time of autopsy at the Medical Examiner's Office of Cuyahoga County, Ohio, in accordance with an approved Institutional Review Board protocol. Subjects were coded to protect their identities. Causes of death were determined by the coroner. All subjects were refrigerated before autopsy once arriving at the coroner's office. Information on the lifetime and current (within last month) psychiatric status of all psychiatric subjects and most control subjects (see below) was obtained in structured clinical interviews by a trained interviewer with the next of kin. The interview used was the Schedule for Affective Disorders and Schizophrenia: Lifetime version (SADS-L, Endicott and Spitzer 1978) supplemented by questions from the Diagnostic Interview Schedule (DIS-III-R) (Robbins et al. 1989) to make diagnoses compatible with the Diagnostic and Statistical Manual of Mental Disorders (DSM-III-R, American Psychiatric Association 1987). The SADS has obtained adequate validity when comparing the patient report to that of an informant (Andreasen et al. 1977). Recently, Kelly and Mann (1996) have validated the use of psychological autopsy by demonstrating good agreement between informant-based retrospective psychological assessment of deceased subjects and chart diagnoses generated by clinicians treating the same subjects before death. They reported a 91% agreement between DSM-III-R diagnoses made antemortem by treating clinicians and informant-based diagnoses made postmortem. Evaluation of drug and alcohol abuse and dependency was assessed using the DIS-III-R. Axis I diagnoses were made by a psychiatrist (H.Y.M.) and a clinical psychologist (J.C.O.), based on data gathered from the structured interview and, when available, hospital and doctor's records. No psychiatric information could be obtained for nine of the 20 control subjects. Although there was no evidence in the coroner's records of any history of psychiatric or neurological disease or prescription medications for psychiatric illnesses in these nine control subjects, the lack of psychiatric illness could not be verified through structured interviews.
Brain tissues were collected from 15 subjects diagnosed of major depression, eight subjects with schizophrenia (summary of subject information is outlined in Table 1) and 20 control subjects. The age of subjects ranged from 23 to 83 years, and demographic comparisons for all three groups of subjects is given in Table 2. The age of control subjects was 52 ± 4 (mean ± SEM) year, major depressives 54 ± 5 year, and schizophrenics 40 ± 3 year. Postmortem delay was 19 ± 1 h for control subjects, 15 ± 2 h for major depressives, and 16 ± 3 h for schizophrenics. Among the 15 subjects diagnosed of major depression, two were diagnosed with co-morbid alcohol dependence, two were smokers (smoking more than 1 pack/day), and one had cocaine dependence. One major depressive had been diagnosed with Parkinson's disease. Among eight schizophrenics, one had a co-morbid diagnosis of inhalant dependence, one of anorexia nervosa, and one was a smoker. Subjects in the control group consisted of six females and 14 males, and the causes of death in this group were: cardiovascular failure (n = 13), gunshot (n = 1), pulmonary embolism (n = 1), aneurism (n = 2), pancreatitis (n = 1), thrombophlebitis (n = 1), and bicycle accident (n = 1). Eleven control subjects were assessed retrospectively through structured interviews and had no Axis I diagnosis (DSM-III-R). One of these control subjects had a history of an episode of adjustment disorder with depressed mood 5 months before death. The remaining nine control subjects had no evidence of psychiatric history or history of psychiatric medication, according to the coroner's records.
A toxicology screen of blood, bile, and urine from all subjects was performed by the county coroner's office. Qualitative and quantitative assays were used to detect the following compounds or classes of compounds: ethanol, barbiturates, benzodiazepines, sympathomimetic drugs, and antidepressant and antipsychotic drugs and their metabolites. In the course of collecting tissue for these studies, all subjects with evidence of antidepressant drugs, other psychotherapeutic drugs, or other psychoactive compounds in the toxicology screen were not included in the study. Toxicology results of major depressive subjects and schizophrenics are shown in Table 1. The toxicology screen of control subjects revealed the following: one subject had alcohol (0.07%) in the blood, two had chlorpheniramine, one had ephedrine, and four had lidocaine. Records collected did indicate antidepressant drug prescriptions within the last month for two of the subjects with major depression and antipsychotic drugs for four of the subjects with schizophrenia.
Dissection
At the time of autopsy, brain tissue was dissected into small blocks. Particular care was taken in the freezing process to maintain gross morphology. Tissues containing right prefrontal cortex (Brodmann's area 10) and right hippocampus, respectively, were placed on hard cardboard, then dipped in isopentane (−50°C) for 5 seconds. Tissues were placed on dry ice for 10 min and then stored at −82°C. The location of Brodmann's area 10 was confirmed cytoarchitectonically (Rajkowska and Goldman-Rakic 1995 a, b; Rajkowska et al. 1998). Hippocampal fields (Figure 1 ) were outlined based on morphological criteria (Duvernoy 1988). Frozen blocks of prefrontal cortex and the right hippocampus were mounted on a specimen chuck of a cryostat microtome (Leica, Cryocut 1800, Reichert-Jung), and tissue sections (20-μm thick) were cut at −16°C and thaw-mounted onto gelatin-coated microscope slides. Sections were dried under refrigeration and then stored at −82°C until assay. Adjacent sections (40-μm thick) were cut for morphometry, dried at room temperature, and then stained with cresyl violet.
Structure of the human hippocampus in coronal section (according to (Duvernoy 1988). This template was used to align hippocampal fields in cresyl violet-stained sections with autoradiograms of the binding of radioligands. 1 = CA1, 2 = CA2, 3 = CA3, 4 = CA4 (fields of cornu ammonis); 5 = C1R (stratum radiatum of cornu ammonis); 6 = C1M (stratum moleculare of cornu ammonis); 7 = MOL (stratum moleculare of detate gyrus); 8 = GRN (stratum granulosum); 9 = POL (polymorphic layer); 10 = FIM (fimbria). Inner and outer layers of the molecular layer (IM and OM) are not shown.
Quantitative Autoradiography
Quantitative autoradiography of the binding of p-[125I]-iodoclonidine ([125I]PIC) to alpha-2 adrenoceptors was performed according to a previously published method (Ordway et al. 1994b). Briefly, duplicate sections were preincubated in Tris-Mg buffer (170 mM Tris, 10 mM MgCl2, pH 7.6) at 23°C for 60 min. Sections were then transferred into slide mailers containing 6 ml of Tris-Mg buffer plus 300 pM of [125I]PIC (2,200 Ci/mmol; New England Nuclear, Wilmington, DE) and incubated for 90 min followed by a 10-min wash in ice-cold Tris buffer. Nonspecific binding of [125I]PIC was defined in the presence of 10 μM l-norepinephrine. The use of norepinephrine to define nonspecific binding eliminated the influence of imidazoline sites in the calculation of specific binding to alpha-2 adrenoceptors.
The binding of [125I]iodopindolol ([125I]IPIN) to beta-1 and beta-2 adrenoceptors was performed, as previously described (Ordway et al. 1988). Duplicate sections were incubated in Tris buffer (Tris 20 mM; NaCl 135 mM, pH 7.4) containing 250 pM of [125I]IPIN for 120 min at 22°C in the presence of the beta-2 antagonist, ICI 118,551 (50 nM) or the beta-1 antagonist, ICI 89,406 (70 nM), respectively. Sections were then washed in ice-cold buffer for 60 min. The nonspecific binding of [125I]IPIN was determined in the presence of l-isoproterenol (100 μM). Dry sections and brain mash calibrated standards (American Radiolabeled Chemicals, Inc., St. Louis, MO) were apposed to [3H]Ultrofilm (Leica Instruments, GmbH) and exposed in X-ray cassettes at room temperature for 20 h. Films were processed with GBX developer and fixer (Eastman Kodak, Rochester, NY) at 17°C. After autoradiography, the same sections were stained lightly with cresyl violet for the anatomical identification. All autoradiograms were analyzed by simultaneously overlaying the image of the autoradiogram with the image of the same Nissl stained section. Densitometric measurements of autoradiograms were made using the Microcomputer Controlled Imaging Device (MCID M2, Imaging Research Inc., St. Catherines, Ontario, Canada).
Statistics
Binding data were analyzed by analysis of variance (ANOVA) for repeated measures (several brain regions in each subject). Planned comparisons were made using contrast analyses. Linear regression analyses were used to compute correlations between binding and age or postmortem interval (GraphPad Prism Ver. 1.0, GraphPad Software Inc., San Diego, CA). Data are reported as the means ± the standard error of the mean.
Abbreviations
CA1, CA2, CA3, CA4 = fields of the cornu ammonis of the hippocampus; C1R = stratum radiatum of cornu ammonis; C1M = stratum moleculare of cornu ammonis; MOL = stratum moleculare of dentate gyrus (IM = inner; OM = outer part of molecular layer); GRN = stratum granulosum; POL = polymorphic layer; FIM = fimbria.
RESULTS
Autoradiography of Alpha-2 Adrenoceptors
The binding of [125I]PIC to alpha-2 adrenoceptors was measured within 11 fields of the hippocampus from 20 control subjects, 14 subjects with a diagnosis of major depression and eight with a diagnosis of schizophrenia, as well as in each of six layers of prefrontal cortex from 13 control subjects and 13 major depressives.
Binding of [125I]PIC to alpha-2 adrenoceptors in hippocampal fields showed a distinct laminar pattern in MOL (Figure 1), with binding in IM much greater than OM (Figure 2 ). The highest binding of [125I]PIC to alpha-2 adrenoceptors within the hippocampus was observed in the C1M and IM, and the lowest binding was in the CA2, CA1, and C1R regions. Specific binding was nearly absent in the FIM (Figure 2). By overlaying the autoradiograms with their respective Nissl-stained sections, the other laminae that did not appear as dense autoradiographic bands could also be identified.
The specific binding of [125I]PIC in hippocampal fields from control, major depressive and schizophrenic subjects revealed identical laminar patterns of alpha-2 adrenoceptor distributions. Furthermore, no significant differences in [125I]PIC binding densities were observed in any of the hippocampal fields between the study groups of control subjects and subjects having a diagnosis of major depression or schizophrenia (Figure 2).
In the prefrontal cortex (Brodmann's area 10), the distribution of [125I]PIC binding to alpha-2 adrenoceptors was not uniform among six cortical layers (Figure 3 ). The highest binding of [125I]PIC to alpha-2 adrenoceptors was observed in layers III and IV. Similar to that observed in the hippocampus, there were no significant differences in [125I]PIC binding to alpha-2 adrenoceptors between subject groups (Figure 3).
Although control and major depressive subjects were matched by age, postmortem delay, and gender as closely as possible before experimentation, we found no significant correlation in either study group between age or postmortem delay and the binding of [125I]PIC to alpha-2 adrenoceptors in any of the 11 subregions of hippocampus or in any of the six layers of the cerebral cortex (data not shown).
Autoradiography of Beta-1 and Beta-2 Adrenoceptors in the Hippocampus
Autoradiograms of [125I]IPIN binding to beta-1 and beta-2 adrenoceptors showed distinct laminar distribution throughout the hippocampal formation (Figures 4 – 5 6 ). However, in contrast to [125I]PIC binding to alpha-2 adrenoceptors, IM and OM of the MOL were not distinguishable. The highest amount of [125I]IPIN binding to beta-1 adrenoceptors was observed in CA1, C1R, C1M, and MOL subfields of the hippocampus (Figures 4 and 5).
There were no significant differences in the binding of [125I]IPIN to beta-1 adrenoceptors in any of the subfields of the hippocampus comparing major depressive subjects to control subjects. However, there was significantly lower [125I]IPIN binding to beta-1 adrenoceptors in several fields of the hippocampus in schizophrenic subjects as compared to control subjects and to major depressive subjects (Figures 4 and 5). The largest differences between schizophrenic and control subjects in [125I]IPIN binding to beta-1 adrenoceptors occurred in the C1R sector (−27%; p < .001), with slightly smaller differences occurring in CA1 (−22%; p < .01), POL (−20%; p < .05), GRN (−19%; p < .01), MOL (−19%; p < .01), and C1M (−19%; p < .05). The smallest, but statistically significant, decrease in binding was observed in CA4 (−15%; p < .05) and CA3 (−16%; p < .05; Figure 5). In the FIM, the binding of [125I]IPIN to beta-1 adrenoceptors was the lowest and was not significantly different between subjects of different study groups (Figure 5). Although records collected did indicate antipsychotic drug prescriptions within the last month before death for four schizophrenic subjects, levels of beta-1 adrenoceptor binding in these subjects were not different from that in the other four schizophrenic subjects (data not shown).
Suicide was the cause of death for most of the subjects diagnosed with major depression and schizophrenia. Therefore, the binding of [125I]IPIN to beta-1 adrenoceptors in the subfields of the hippocampus of suicides (including major depressive and schizophrenic subjects; n = 16) was compared to that of control subjects (n = 19) and no significant differences were observed (data not shown).
The specific binding of [125I]IPIN to beta-2 adrenoceptors was about three times higher than its binding to beta-1 adrenoceptors in the same hippocampal subregion and showed a different pattern of laminar distribution than the beta-1 adrenoceptor distribution. Highest binding of [125I]IPIN to beta-2 adrenoceptors was observed in C1M, POL, GRN, MOL of the hippocampus (Figure 6). There were no significant differences in binding to beta-2 adrenoceptors between the three groups of subjects for any of the subregions of the hippocampus (Figure 6). Despite the lack of statistical significance, amounts of [125I]IPIN to beta-2 adrenoceptors were consistently lower in all hippocampal subregions of the schizophrenic subjects relative to control and major depressive subjects.
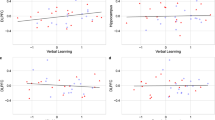
Similarly to the studies of alpha-2 adrenoceptors, the control, schizophrenic, and major depressive subjects were matched by age, postmortem delay, and gender as closely as possible before experimentation, we found no significant correlation in either study group between age or postmortem delay and the binding of [125I]IPIN to neither beta-1 nor beta-2 adrenoceptors in any of the 11 fields of hippocampus (data not shown).
DISCUSSION
Noradrenergic receptors in the brain of laboratory animals are up- or down-regulated in response to decreases or increases, respectively, in synaptic norepinephrine (Bylund 1979; Waldmeier 1981; Bylund 1988; Barturen and Garcia-Sevilla 1992; Kovachich et al. 1993). The plasticity of noradrenergic receptor density has led a number of investigators to measure noradrenergic receptors in postmortem tissues from psychiatrically ill subjects in an attempt ascertain the premortem neurochemical status of noradrenergic transmission. After almost two decades of research, there is no consensus among researchers with regard to whether noradrenergic receptors are not changed, up- or down-regulated in psychiatric disease (Crow et al. 1984; Meana et al. 1992; Arango et al. 1993; Gonzalez et al. 1994; Ordway et al. 1994b; Callado et al. 1998). There are many possible explanations for the lack of consensus, but primary among them are the heterogeneity in psychiatric illnesses of subjects within study groups and lack of precise anatomical location of measurements (Rajkowska 1997). The present study was designed to reduce variability in the sample population and to address more directly the role of the noradrenergic system in major depression and schizophrenia by: (1) using tissues from individuals for whom a rigorous evaluation of psychiatric status was performed for both control and psychiatric cases; (2) applying strict exclusion criteria to reduce or eliminate the contribution of neuropathology and recent antidepressant drug treatment; (3) confirming anatomical designations using cytorarchitectonic criteria; and (4) careful pairing and simultaneous processing of tissues from control and psychiatric subjects. Our findings confirm the findings of some, but not all, researchers demonstrating no differences in levels of binding to alpha-2 or beta adrenergic receptors in cortical or subcortical brain regions in subjects with major depression as compared to psychiatrically normal control subjects. Unexpectedly, reduced binding to beta-1 adrenergic receptors in the hippocampus of schizophrenic subjects suggests that greater attention should be paid to the study of the noradrenergic system in this illness.
Alpha-2 Adrenoceptors
Our data reveal no differences in the amount of [125I]-PIC binding to alpha-2 adrenoceptors measured in regions of the hippocampal formation or in any of cerebral cortical layers when comparing subjects with diagnoses of major depression or of schizophrenia to psychiatrically normal controls. Moreover, no change was observed in the binding of alpha-2 adrenoceptor antagonists; [3H]RX 781094 in the frontal cortex (Ferrier et al. 1986; Callado et al. 1998) or [3H]rauwolscine in the hippocampus and occipital cortex (Crow et al. 1984) of subjects diagnosed with major depression in comparison to the control cases. Because most of the major depressives in the present study were victims of suicide, these data are concordant with the observations of Arango et al. (1993), who found no difference in binding of the related alpha-2 adrenoceptor agonist, [3H]p-aminoclonidine, to alpha-2 adrenoceptors in the prefrontal cortex of victims of suicide relative to the normal controls. In contrast, another group of researchers (Gonzalez et al. 1994; Callado et al. 1998) have demonstrated a higher number of binding sites for [3H]UK 14304 and for [3H]clonidine (Callado et al. 1998), agonists at alpha-2 adrenoceptors, in the hippocampus and frontal cortex (Brodmann's area 8 and 9) of depressed suicide victims compared to controls who were free of medical diagnosis and treatment. The discrepancies between our data and those of Garcia-Sevilla group (Gonzalez et al. 1994; Callado et al. 1998) could be explained by different anatomical localizations studied within prefrontal cortex. Brodmann's area 10 (studied in the present paper) could be clearly distinguished from more posteriorly located areas 8 and 9 by a distinct cytoarchitectonic and myeloarchitectonic pattern of cortical composition (Rajkowska and Goldman-Rakic 1995a, 1995b). Although Arango and co-workers (1993) did not report the psychiatric status of the suicide victims, they did not observe any changes in binding to alpha-2 adrenoceptors in the anterior part of Brodmann's area 9. Because the most anterior part of area 9 (studied by Arango et al. 1993) has some cytoarchitectonic features similar to those of area 10 (present study; Rajkowska and co-workers, unpublished observations), it is possible that the same cytoarchitectonic region was analyzed in both studies.
Another discrepancy between the studies of the Garcia-Sevilla group (Gonzalez et al. 1994; Callado et al. 1998, Arango et al. (1993), and the present investigation was the length of the postmortem delay for the tissue specimens. The average postmortem delays for the present study were 15 ± 2 h for major depressives. The postmortem delays for the study by Arango et al. (1993) was 15 ±1 h for suicide subjects. The postmortem delays for psychiatric cases by the Garcia-Sevilla group were more than twice as long as Arango et al.(1993) and the present study. For example, Gonzalez et al. (1994) reported postmortem delays of 36 ± 16 h for depressed suicides, and Callado et al. (1998) reported postmortem delays of 39 ± 6 h for depressed suicides. Interestingly, the only other report of elevated agonist ([3H]UK 14304) binding to alpha-2 adrenoceptors in human frontal cortex was by Meana et al. (1992), who also utilized tissues that had an average postmortem delay of approximately 30 hours for depressed suicides. None of the studies cited above, including the present investigation, demonstrated a significant effect of postmortem delay on levels of binding to alpha-2 adrenoceptors. However, it should be kept in mind that one variable in studies utilizing tissues from depressed suicide victims is the environmental conditions surrounding the death. Because suicide is rarely performed in a public setting, the victim is often found hours after the suicide. Hence, it is conceivable that variability in the environmental conditions surrounding the victim during this time, before the cadaver is refrigerated, could produce highly variable effects on postmortem decay that could make difficult the demonstration of statistically significant correlations between postmortem delay and binding. Carefully controlled experiments designed to mimic environmental conditions occurring in the postmortem interval are difficult, but are warranted to rule out the possibility that long delays “unmask” radioligand binding to alpha-2 adrenoceptors.
There are three subtypes of alpha-2 adrenoceptors in the brain (Bylund 1985; Bylund 1988; Lomasney et al. 1990; Harrison et al. 1991; Nicholas et al. 1993). The presynaptic alpha-2 adrenoceptor on noradrenergic neurons; that is, the autoreceptor, seems to be the alpha-2A adrenoceptor (De Vos et al. 1992; Nicholas et al. 1993). However, this subtype of adrenoceptor also occurs postsynaptically on a number of catecholaminergic and noncatecholaminergic neurons, as well as on glia in many brain regions, including the prefrontal cortex (Aoki et al. 1994). Most of the alpha-2 adrenoceptors in a projection area such as frontal cortex are post-, rather than presynaptic (autoreceptors), because lesioning noradrenergic neuronal fibers in the rat brain does not decrease binding of [3H]clonidine (U'Prichard et al. 1979; Dausse et al. 1982; Gross et al. 1985) or [3H]rauwolscine (Ordway 1995) to alpha-2 adrenoceptors in the cerebral cortex. Thus, it is likely that the synaptic location of alpha-2 adrenoceptors labeled in the present study was predominately postsynaptic. Furthermore, it is likely that the alpha-2A adrenoceptor is the predominate subtype labeled in the present study, because this subtype is the predominate alpha-2 adrenoceptor in the human frontal cortex (De Vos et al. 1992; Ordway et al. 1993; Callado et al. 1998), and [125I]PIC binds this subtype preferentially (Gerhardt et al. 1990; Ordway et al. 1993; Ordway et al. 1994b).
Beta Adrenoceptors
The binding of [125I]IPIN to beta-1 and beta-2 adrenoceptors in the hippocampus of major depressive subjects was not significantly different from that of normal control subjects. These data are concordant with another study (De Paermentier et al. 1990) that demonstrated no differences in beta-1 and beta-2 adrenoceptor densities, using the radioligand, [3H]CGP 12177, in the hippocampus of control subjects and depressed suicide victims. In contrast, Crow and co-workers (1984) observed a decrease in the binding of [3H]dihydroalprenolol to beta adrenoceptors (beta-1 plus beta-2) in the hippocampus of depressed subjects as compared to control cases. In this latter study, the nonspecific binding of [3H]dihydroalprenolol was determined with propranolol. In addition to beta adrenoceptors, both propranolol and [3H]dihydroalprenolol label serotonin receptors. According to the studies of Riva and Creese (1989), there is no concentration of propranolol that could satisfactorily be used to displace [3H]dihydroalprenolol specifically from beta adrenoceptors. Hence, it is difficult to know whether lower binding in the hippocampus of depressive subjects observed by Crow and co-workers (1984) is a decrease in beta adrenergic or serotonin receptors.
The binding of [125I]IPIN to beta-1 adrenoceptors was approximately threefold lower than binding to beta-2 adrenoceptors. Furthermore, the pattern of distribution of beta-1 adrenoceptors throughout the hippocampus was distinctly different from that of beta-2 adrenoceptors. The high concentration of beta-2 adrenoceptors, relative to beta-1 adrenoceptors, in the human hippocampus is in marked contrast to the relative densities of these receptors in the rat hippocampus (Rainbow et al. 1984). Joyce et al. (1992) have also demonstrated a high density of beta-2 adrenoceptors relative to beta-1 adrenoceptors in the human hippocampus.
Of major interest in the present study is the demonstration of lower [125I]IPIN binding to beta-1 adrenoceptors in the hippocampus from schizophrenic subjects relative to subjects with major depression or psychiatrically normal control subjects. To the best of our knowledge, this is the first demonstration of reduced radioligand binding to beta-1 adrenoceptors in hippocampal formation of schizophrenics. Joyce and co-workers (1992), using the same radioligand and displacing agents, reported no statistically significant differences in beta-1 or beta-2 adrenoceptor binding in the hippocampus between control and schizophrenic subjects. Joyce and co-workers (1992) studied the field of the cornu ammonis in both left and right hippocampi. Examination of their data from the right hippocampus shows 25% lower binding to beta-1 adrenoceptors in schizophrenic subjects as compared to control subjects. Although this difference did not reach statistical significance (Joyce et al. 1992), it is comparable to the magnitude of reductions observed in the present study in which all hippocampi were obtained from the right hemisphere, and in which discrete fields of the cornu ammonis were measured.
Reduced binding of [125I]IPIN to hippocampal beta-1 adrenoceptors may reflect receptor down-regulation secondary to enhanced noradrenergic transmission or may be a result of a general degenerative process in schizophrenia. The postulate of noradrenergic overactivity in schizophrenia is supported by a number of observations. For example, hippocampal beta-1 adrenoceptors down-regulate in rats following pharmacological treatments that elevate synaptic norepinephrine (Sulser et al. 1984; Ordway et al. 1991). Elevated concentrations of norepinephrine have been detected postmortem in limbic forebrain (Farley et al. 1978; Bird et al. 1979; Hornykiewicz 1986) in schizophrenic subjects as compared to control subjects. An elevation of norepinephrine in the cerebrospinal fluid of schizophrenics compared to controls has also been reported (Gomes et al. 1980; Lake et al. 1980; Sternberg et al. 1981; Van Kammen et al. 1989). Interestingly, measures of noradrenergic activity seem to be good indicators and/or predictors of the state of disease and its outcome (Hornykiewicz 1982, 1986; Van Kammen and Kelley 1991).
A reduction in beta-1 adrenoceptor binding secondary to neuronal cell loss is possible given numerous postmortem and neuroimaging studies revealing hippocampal atrophy in schizophrenic subjects (Bogerts et al. 1985; Falkai and Bogerts 1986; Falkai et al. 1988; Benes et al. 1991). Cell loss (Falkai and Bogerts 1986) and/or reduced neuronal sizes (Benes et al. 1991) in the hippocampus of schizophrenics has also been reported. However, reduced density of beta-1 adrenoceptors simply attributable to cell loss seems unlikely, because binding to alpha-2 adrenoceptors, another predominately postsynaptic noradrenergic receptor (see Ordway 1995), was not different in the same hippocampi of schizophrenics compared to control subjects. In fact, there was a tendency for higher, rather than lower, [125I]PIC binding to alpha-2 adrenoceptors in several hippocampal fields.
A malfunction of two brain mechanisms controlled by norepinephrine could contribute to psychotic behavior. One of those could be a defect in the noradrenergically controlled attentional (stimulus filtering) mechanisms of the locus coeruleus noradrenergic dorsal bundle that innervates the limbic forebrain area and the hippocampus. The second mechanism could be an alteration in the noradrenergic control of brain dopaminergic systems that generate motivational responses (see Hornykiewicz 1986). Our data support the hypothesis of noradrenergic overactivity in schizophrenia that leads to a down-regulation of beta-1 adrenoceptors in the hippocampus, and indicate that alterations in central noradrenergic transmission may contribute to the neurochemical pathology of schizophrenia.
CONCLUSIONS
There is compelling evidence of a biological abnormality of central noradrenergic neurons in major depression and suicide, characterized by elevated levels of tyrosine hydroxylase (Zhu et al. 1995), elevated radioligand binding to alpha-2 adrenoceptors (Ordway et al. 1994b), and reduced density of norepinephrine transporters (Klimek et al. 1997) in the noradrenergic locus coeruleus. Reduced levels of norepinephrine transporters, up-regulation of tyrosine hydroxylase, and up-regulation of alpha-2 adrenoceptors are neurobiological changes observed after depletion of norepinephrine in the rat (Bylund and Martinez 1980; Lee et al. 1983; Bylund 1988; Melia et al. 1992). Therefore, postmortem findings suggest that major depression is characterized, at least in part, by a reduced availability of norepinephrine at the synapse. We would expect that noradrenergic receptors in projection areas of the locus coeruleus (e.g., hippocampus) would also be up-regulated in major depression or suicide. However, no significant differences in binding to alpha-2, beta-1, or beta-2 adrenoceptors were observed in the frontal cortex and/or hippocampus from major depressives, suggesting that alterations in noradrenergic neurochemistry in depression are neuroanatomically specific. Previous studies demonstrating alterations in protein levels in noradrenergic cells of origin may reflect neurochemical changes in subpopulations of cells having discrete projections. The present findings do not exclude the possibility that alpha-2, beta-1, or beta-2 adrenoceptors could be functionally abnormal; thatis, changes in second messenger systems or the affinity of norepinephrine for these receptors may be altered in depression. The demonstration of reduced beta-1 adrenoceptor binding in the hippocampus of schizophrenic subjects relative to normal control and major depressive subjects provides further evidence for a role of norepinephrine in the biology of schizophrenia and distinguishes noradrenergic pathology in schizophrenia from that in major depression.
References
American Psychiatric Association . (1987): Diagnostic and Statistical Manual of Mental Disorders, Revised. Washington, DC, American Psychiatric Association
Andreasen NC, Endicott J, Spitzer RL, Winokur G . (1977): The family history method using diagnostic criteria. Reliability and validity. Arch Gen Psychiat 34: 1229–1235
Aoki C, Go CG, Venkatesan C, Kurose H . (1994): Perikaryal and synaptic localization of α2-adrenergic receptor-like immunoreactivity. Brain Res 650: 181–204
Arango V, Ernsberger P, Marzuk PM, Chen JS, Tierney H, Stanley M, Reis DJ, Mann JJ . (1990): Autoradiographic demonstration of increased serotonin 5-HT2 and Beta-adrenergic receptor binding sites in the brain of suicide victims. Arch Gen Psychiat 47: 1038–1047
Arango V, Ernsberger P, Sved AF, Mann JJ . (1993): Quantitative autoradiography of α1 and α2 adrenergic receptors in the cerebral cortex of controls and suicide victims. Brain Res 630: 271–282
Archer T, Cotic T, Järbe TUC . (1982): Attenuation of the context effect and lack of unconditioned stimulus-pre-exposure effect in the taste-aversion learning following treatment with DPP4, the selective noradrenaline neurotoxin. Behav Neural Biol 35: 159–173
Aston-Jones G, Shipley MT, Chouvet G, Ennis M, van Bockstaele E, Pierbone V, Shiekhattar R, Akaoka H, Drolet G, Astier B, Charlety P, Valentino RJ, Williams JT . (1991): Afferent regulation of locus coeruleus neurons: Anatomy, physiology, and pharmacology. Prog Brain Res 88: 47–75
Barturen F, Garcia-Sevilla JA . (1992): Long-term treatment with desipramine increases the turnover of α2-adrenoceptors in the rat brain. Mol Pharmacol 42: 846–855
Benes FM, Sorensen I, Bird ED . (1991): Reduced neruonal size in posterior hippocampus of schizophrenic patients. Schizophr Bull 17: 597–608
Biegon A, Israeli M . (1988): Regionally selective increases in β-adrenergic receptor density in the brains of suicide victims. Brain Res 442: 199–203
Bird OE, Spokes EG, Iversen LL . (1979): Brain norepinephrine and dopamine in schizophrenia. Science 204: 456
Bogerts B, Meertz E, Schoenfeldt-Bausch R . (1985): Basal ganglia and limbic system pathology in schizophrenia: Morphometric study of brain volume shrinkage. Arch Gen Psychiat 42: 784–791
Bylund DB . (1979): Regulation of central adrenergic receptors. Adv Exper Med Biol 116: 133–162
Bylund DB . (1985): Heterogeneity of alpha-2 adrenergic receptors. Pharmacol Biochem Behav 22: 835–843
Bylund DB . (1988): Subtypes of alpha 2-adrenoceptors: Pharmacological and molecular biological evidence converge. Trends Pharmacol Sci 9: 356–361
Bylund DB, Martinez JR . (1980): Alpha 2-adrenergic receptors appear in rat salivary glands after reserpine treatment. Nature 285: 229–230
Callado LF, Meana JJ, Grijalba B, Pazos A, Sastre M, Garcia-Sevilla JA . (1998): Selective increase of α2A-adrenoceptor agonist binding sites in brains of depressed suicide victims. J Neurochem 70: 1114–1123
Crow TJ, Cross AJ, Cooper SJ, Deakin JFW, Ferrier IN, Johnson JA, Joseph MH, Owen F, Poulter M, Lofthouse R, Corsellis JAN, Chambers DR, Blessed G, Perry EK, Perry RH, Tomlinson BE . (1984): Neurotransmitter receptors and monoamine metabolites in the brains of patients with Alzheimer-type dementia and depression, and suicides. Neuropharmacology 23: 1561–1569
Dausse JP, Le Quan-Bui KH, Meyer P . (1982): Alpha 1- and alpha 2-adrenoceptors in rat cerebral cortex: Effects of neonatal treatment with 6-hydroxydopamine. Eur J Pharmacol 78: 15–20
De Paermentier F, Cheetham SC, Crompton MR, Katona CL, Horton RW . (1990): Brain beta-adrenoceptor binding sites in antidepressant-free depressed suicide victims. Brain Res 525: 71–77
De Vos H, Vaquelin G, De Keyser J, De Backer J-P, Van Liefde I . (1992): Regional distribution of α2A- and α2B-adrenoceptor subtypes in postmortem human brain. J Neurochem 58: 1555–1560
Duvernoy HM . (1988): The Human Hippocampus. Munich, J. F. Bergmann Verlag
Endicott J, Spitzer RL . (1978): A diagnostic interview: The schedule for affective disorders and schizophrenia. Arch Gen Psychiat 35: 837–844
Falkai P, Bogerts B, Rozumek M . (1988): Limbic pathology in schizophrenia: The entorhinal region—A morphometric study. Biol Psychiat 24: 515–521
Falkai P, Bogerts B . (1986): Cell loss in the hippocampus of schizophrenics. Eur Arch Psychiat Neurol Sci 236: 154–161
Farley IJ, Price KS, McCullough E, Deck JHN, Hordynski W, Hornykiewicz O . (1978): Norepinephrine in chronic paranoid schizophremia: Above-normal levels in limbic forebrain. Science 200: 456–457
Ferrier IN, McKeith IG, Cross AJ, Perry EK, Candy JM, Perry RH . (1986): Postmortem neurochemical studies in depression. Ann N Y Acad Sci 487: 128–142
Ferrier IN, Perry EK . (1992): Postmortem studies in affective disorder. Psychological Med 22: 835–838
Gerhardt MA, Wade SM, Neubig RR . (1990): p-[125I]Iodoclonidine is a partial agonist at the α2-adrenergic receptor. Mol Pharmacol 38: 214–221
Gomes UCR, Shanley BC, Potgieter L, Roux JT . (1980): Noradrenergic overactivity in chronic schizophrenia: Evidence based on cerebrospinal fluid noradrenaline and cyclic nucleotide concentrations. Brit J Psychiat 137: 346–351
Gonzalez AM, Pascual J, Meana JJ, Barturen F, del Arco C, Pazos A, Garcia-Sevila JA . (1994): Autoradiographic demonstration of increased α2-adrenoceptor agonist binding sites in the hippocampus and frontal cortex of depressed suicide victims. J Neurochem 63: 256–265
Gross G, Gothert M, Glapa U, Engel G, Schumann HJ . (1985): Lesioning of serotoninergic and noradrenergic nerve fibers of the rat brain does not decrease binding of 3H-clonidine and 3H-rauwolscine to cortical membranes. Naunyn-Schmiedeberg's Arch Pharmacol 328: 229–235
Harrison JK, D'Angelo DD, Zeng DW, Lynch KR . (1991): Pharmacological characterization of rat alpha 2-adrenergic receptors. Mol Pharmacol 40: 407–412
Hornykiewicz O . (1982): Brain catecholamines in schizophrenia—A good case for noradrenaline. Nature 299: 484–485
Hornykiewicz O . (1986): Brain Noradrenaline and Schizophrenia. In van Ree JM, Matthysse SW (eds), Progress in Brain Research. Vienna, Elsevier, pp 29–39
Joyce JN, Lexow N, Kim SJ, Artymyshyn R, Senzon S, Lawrence D, Cassanova MF, Kleinman JE, Bird ED, Winokur A . (1992): Distribution of beta-adrenergic receptor subtypes in human postmortem brain: Alterations in limbic regions of schizophrenics. Synapse 10: 228–246
Kelly TM, Mann JJ . (1996): Validity of DSM-III-R diagnosis by psychological autopsy: A comparison with clinician antemortem diagnosis. Acta Psychiat Scand 94: 337–343
Klimek V, Stockmeier CA, Overholser JC, Meltzer HY, Kalka S, Dilley G, Ordway GA . (1997): Reduced levels of norepinephrine transporters in the locus coeruleus in major depression. J Neurosci 17: 8451–8458
Kovachich GB, Frazer A, Aronson CE . (1993): Effect of chronic administration of antidepressants on alpha 2-adrenoceptors in the locus coeruleus and its projection fields in rat brain determined by quantitative autoradiography. Neuropsychopharmacology 8: 57–65
Lake CR, Sternberg DE, vanKammen DP, Ballenger JC, Ziegler MG, Post RM, Kopin IJ, Bunney WE . (1980): Schizophrenia: Elevated cerebrospinal fluid norepinephrine. Science 207: 331–333
Lake CR, Pickar D, Ziegler MG, Lipper S, Slater S, Murphy DL . (1982): High plasma norepinephrine levels in patients with major affective disorder. Am J Psychiat 139: 1315–1318
Lee C-M, Javitch JA, Snyder SH . (1983): Recognition sites for norepinephrine uptake: Regulation by neurotransmitter. Science 220: 626–629
Lomasney JW, Lorenz W, Allen LF, King K, Regan JW, Yang-Feng TL, Caron MG, Lefkowitz RJ . (1990): Expansion of the alpha 2-adrenergic receptor family: Cloning and characterization of a human alpha 2-adrenergic receptor subtype, the gene for which is located on chromosome 2. Proc Natl Acad Sci USA 87: 5094–5098
Mann JJ, Stanley M, McBride PA, McEwen BS . (1986): Increased serotonin2 and β-adrenergic receptor binding in the frontal cortices of suicide victims. Arch Gen Psychiat 43: 954–959
Mason ST . (1981): Noradrenaline in the brain: Progress in theories of behavioral function. Prog Neurobiol 16: 263–303
Meana JJ, Barturen F, Garcia-Sevilla JA . (1992): Alpha 2-adrenoceptors in the brain of suicide victims: Increased receptor density associated with major depression. Biol Psychiat 31: 471–490
Meana JJ, Garcia-Sevilla JA . (1987): Increased α2-adrenoceptor density in the frontal cortex of depressed suicide victims. J Neural Transm 70: 377–381
Melia KR, Rasmussen K, Terwilliger RZ, Haycock JW, Nestler EJ, Duman RS . (1992): Coordinate regulation of the cyclic AMP system with firing rate and expression of tyrosine hydroxylase in the rat locus coeruleus: Effects of chronic stress and drug treatments. J Neurochem 58: 494–502
Melia KR, Duman RS . (1991): Involvement of corticotropin-releasing factor in chronic stress regulation of the brain noradrenergic system. Proc Natl Acad Sci USA 88: 8382–8386
Nicholas AP, Pieribone V, Hokfelt T . (1993): Distributions of mRNAs for alpha-2 adrenergic receptor subtypes in rat brain: An in situ hybridization study. J Comp Neurol 328: 575–594
Ordway GA . (1995): Effect of noradrenergic lesions on subtypes of α2-adrenoceptors in rat brain. J Neurochem 64: 1118–11261
Ordway GA, Gambarana C, Frazer A . (1988): Quantitative autoradiography of central beta adrenoceptor subtypes: Comparison of the effects of chronic treatment with desipramine or centrally administered l-isoproterenol. J Pharmacol Exp Ther 247: 379–389
Ordway GA, Gambarana C, Tejani-Butt SM, Areso P, Hauptmann M, Frazer A . (1991): Preferential reduction of binding of 125I-iodopindolol to beta-1 adrenoceptors in the amygdala of rat after antidepressant treatments. J Pharmacol Exp Ther 257: 681–690
Ordway GA, Jaconetta SM, Halaris AE . (1993): Characterization of subtypes of alpha-2 adrenoceptors in the human brain. J Pharmacol Exp Ther 264: 967–976
Ordway GA, Smith KS, Haycock JW . (1994a): Elevated tyrosine hydroxylase in the locus coeruleus of suicide victims. J Neurochem 62: 680–685
Ordway GA, Widdowson PS, Smith KS, Halaris A . (1994b): Agonist binding to α2-adrenoceptors is elevated in the locus coeruleus from victims of suicide. J Neurochem 63: 617–624
Ordway GA . (1995): Effect of noradrenergic lesions on subtypes of α2-adrenoceptors in rat brain. J Neurochem 64: 1118–1126
Plaznik A, Pucilowski O, Kostowski W, Bidzinski A, Hauptmann M . (1982): Rotational behavior produced by unilateral ventral noradrenergic bundle lesions: Evidence for a noradrenergic–dopaminergic interaction in the brain. Pharmacol Biochem Behav 17: 619–622
Prange AJ, Jr . (1964): The pharmacology and biochemistry of depression. Dis Nerv Syst 25: 217–221
Rainbow TC, Parsons B, Wolfe BB . (1984): Quantitative autoradiography of β1- and β2-adrenergic receptors in rat cerebellum and cerebral cortex. Proc Natl Acad Sci USA 81: 1585–1589
Rajkowska G . (1997): Morphometric methods for studying the prefrontal cortex in suicide victims and psychiatric patients. In Stoff DM, Mann JJ (eds), The Neurobiology of Suicide. From the Bench to the Clinic. New York, New York Acad Sci 836: 253–268
Rajkowska G, de Vos K, Pool CW, Roland PE, Zilles K, Uylings H . (1998): 3-D Cytoarchitectonic parcellation of human orbitofrontal cortex. Correlation with postmortem MRI. Soc Neurosci Abstr 24: Abstract.
Rajkowska G, Goldman-Rakic PS . (1995a): Cytoarchitectonic definition of prefrontal areas in the normal human cortex: I. Remapping of areas 9 and 46 using quantitative criteria. Cerebral Cortex 5: 307–322
Rajkowska G, Goldman-Rakic PS . (1995b): Cytoarchitectonic definition of prefrontal areas in the normal human cortex: II. Variability in locations of areas 9 and 46 and relationship to the Talairach coordinate system. Cerebr Cortex 5: 323–337
Riva MA, Creese I . (1989): Reevaluation of the regulation of β-adrenergic receptor binding by desipramine treatment. Mol Pharmacol 36: 211–218
Robbins L, Cottler L, Keating S . (1989): NIMH Diagnostic Interview Schedule. Version III. Revised (DIS-III-R). St. Louis, MO: Washington University Department of Psychiatry
Schildkraut JJ . (1965): The catecholamine hypothesis of affective disorders: A review of supporting evidence. Am J Psychiat 122: 509–522
Sternberg DE, Van Kammen DP, Lake CR, Ballenger JC, Marder SR, Bunney WE, Jr . (1981): The effect of pimozide on CSF norepinephrine in schizophrenia. Am J Psychiat 138: 1045–1050
Sulser F, Gillespie DD, Manier DH . (1984): Physiological mechanism and significance of changes in the regulation of beta adenoceptors by antidepressants. Clin Neuropharmacol 7: 304–305
U'Prichard DC, Bechtel WD, Rouot BM, Snyder SH . (1979): Multiple apparent alpha-noradrenergic receptor binding sites in rat brain: Effect of 6-hydroxydopamine. Mol Pharmacol 16: 47–60
Van Kammen DP, Peters J, van Kammen WB, Nugent A, Goetz KL, Yao J, Linnoila M . (1989): CSF norepinephrine in schizophrenia is elevated prior to relapse after haloperidol withdrawal. Biol Psychiat 26: 176–188
Van Kammen DP, Antelman S . (1984): Impaired noradrenergic transmission in schizophrenia? Life Sci 34: 1403–1413
Van Kammen DP, Kelley M . (1991): Dopamine and norepinephrine activity in schizophrenia. An integrative perspective. Schizophr Res 4: 173–191
Waldmeier PC . (1981): Noradrenergic transmission in depression: Under- or overfunction? Pharmacopsychiatria 14: 3–9
Weinberger DR, Wagner RL, Wyatt RJ . (1983): Neuropathological studies of schizophrenia: A selective review. Schizophr Bull 9: 193–212
Zhu M-Y, Haycock JW, Klimek V, Luker SN, Stockmeier CA, Dilley G, Meltzer HY, Overholser JC, Ordway GA . (1995): Elevation of tyrosine hydroxylase in the locus coeruleus of subjects with major depression. Soc Neurosci Abs 21: 194 abstract.
Acknowledgements
This research was supported by National Institutes of Health Grants MH46692 (G.A.O), MH45488 (C.A.S.), MH55872 (G.R.), a Young Investigator Award from the National Alliance for Research on Schizophrenia and Depression (V.K.), and a grant from the American Foundation for Suicide Prevention (V.K.). The support of Dr. Elizabeth Balraj and the staff of the Cuyahoga County Coroner's Office (Cleveland, OH) are appreciated.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Klimek, V., Rajkowska, G., Luker, S. et al. Brain Noradrenergic Receptors in Major Depression and Schizophrenia. Neuropsychopharmacol 21, 69–81 (1999). https://doi.org/10.1016/S0893-133X(98)00134-1
Received:
Revised:
Accepted:
Issue Date:
DOI: https://doi.org/10.1016/S0893-133X(98)00134-1
Keywords
This article is cited by
-
Biomarkers in the cerebrospinal fluid of patients with psychotic disorders compared to healthy controls: a systematic review and meta-analysis
Molecular Psychiatry (2023)
-
Evaluation of the role of monoaminergic and nonmonoaminergic systems in the psychotropic effects of morin in mice: an interaction study with receptor blockers
Nutrire (2021)
-
Modulation of Monoaminergic Systems by Antidepressants in the Frontal Cortex of Rats After Chronic Mild Stress Exposure
Molecular Neurobiology (2019)
-
Differential modulation of alpha-1 adrenoceptor subtypes by antidepressants in the rat brain
Journal of Neural Transmission (2010)
-
Targeting the Hippocampal Mossy Fiber Synapse for the Treatment of Psychiatric Disorders
Molecular Neurobiology (2009)