Abstract
The negative physical and affective aspects of opioid abstinence contribute to the prolongation of substance abuse. Withdrawal treatment is successful only in a subset of subjects, yet little is known about the neurobiological causes of these individual differences. Here, we compare the somatic and motivational components of opioid withdrawal in animals with high reactivity (HR) vs low reactivity (LR) to novelty, a phenotype associated with differential vulnerability to drug abuse. During withdrawal, HR relative to LR showed increased teeth chattering and eye twitching episodes, somatic signs associated with adrenergic modulation. Given the role of noradrenergic circuitry of the extended amygdala in opioid withdrawal, we examined adrenergic receptor gene expression in the bed nucleus of stria terminalis (BST) and central nucleus of the amygdala. Relative to LR, HR rats exhibit a selective increase in β1 adrenergic receptor expression in lateral and medial BST. To uncover the functional relevance of this difference, we microinjected betaxolol, a selective β1 receptor antagonist, into dorsal BST and assessed somatic and affective responses during withdrawal. Betaxolol microinjection dose-dependently decreased teeth chattering episodes in HR to levels observed in LR animals. Moreover, the antagonist blocked conditioned place aversion, a measure of negative affect associated with withdrawal, in HR but not in LR animals. Our results reveal for the first time that reactivity to novelty predicts somatic and affective aspects of opiate dependence, and that β1 receptors in BST are implicated in opiate withdrawal but only in novelty-seeking individuals.
Similar content being viewed by others
INTRODUCTION
Opiate abuse leads to the development of physical and psychological dependence and, upon drug cessation, produces a withdrawal syndrome characterized by motor, autonomic, and affective symptoms (Gutstein and Akil, 2001; De Vries and Shippenberg, 2002). Even though management of withdrawal symptoms cannot be considered a treatment itself for opiate dependence, it is often the first step for long-term treatment. Indeed, a dominant current hypothesis is that anxiety and negative affect associated with withdrawal contribute to the addict's drive to continue to abuse drugs (Aston-Jones and Harris, 2004). Several pharmacotherapeutic approaches are currently in use for the treatment of opiate withdrawal but none of them is effective in more than a percentage of patients. Medication regimens that use orally active opioid agonists such as methadone to control withdrawal symptoms achieve abstinence in only 40% of the patients (Senay et al, 1977). Rapid detoxification protocols that precipitate withdrawal with an opioid antagonist while withdrawal symptoms are managed with adjuvant medications achieve higher rate of success, but a subset of patients fails to complete detoxification (O'Connor et al, 1997). Because of individual differences in response to treatments, prevention of opiate abuse and success in achieving complete detoxification in a population of patients as broad as possible require a mechanistic understanding not only of the basic neurobiology of withdrawal, but also of the biology of individual differences in its physiological and affective symptoms.
There is ample evidence that the noradrenergic system is activated during opioid withdrawal and contributes to its symptoms. Intravenous injection of yohimbine, an α2 adrenergic receptor antagonist that inhibits autoreceptors and increases noradrenergic transmission, elicits withdrawal symptoms and elevates craving for opiates in methadone-maintained patients (Stine et al, 2002). Conversely, α2 adrenergic receptor agonists such as clonidine and lofexidine are used to control opioid withdrawal symptoms (for review see Gowing et al, 2002).
Animal models have focused attention on the role of the adrenergic system of the extended amygdala in opiate withdrawal. Thus, β adrenergic antagonists injected in bed nucleus of stria terminalis (BST) block somatic signs of opiate withdrawal (Aston-Jones et al, 1999; Delfs et al, 2000). Conditioned place aversion (CPA) associated with opiate withdrawal is attenuated by a combination of two classes of β adrenergic antagonists microinjected into central nucleus of the amygdala (CeA) (Watanabe et al, 2003) and blocked by their injection into BST (Aston-Jones et al, 1999; Delfs et al, 2000).
However, no animal models have elucidated the neurobiological causes of differences in opioid withdrawal and treatment responses, or the role of the adrenergic system in these differences. Here, we rely on a model of individual differences in vulnerability to drug addiction predicted by a test of novelty-seeking behavior (Piazza et al, 1989; Kabbaj et al, 2001, 2002). Animals that exhibit a high locomotor response to novelty (HR) show higher morphine-induced psychomotor activity (Deroche et al, 1993) and greater levels of morphine self-administration (Ambrosio et al, 1995) than rats with low locomotion (LR). But do these two groups exhibit differences in opioid withdrawal, and can we uncover the neurobiological bases of these differences?
This series of studies describes significant differences in some somatic signs of opioid withdrawal in HR vs LR rats, demonstrates differential levels of β1 adrenergic receptor expression in BST, and uses microinjection of the antagonist betaxolol to implicate this specific receptor subtype in the somatic and affective aspects of opiate withdrawal.
This is the first demonstration of the role of the β1 receptor subtype in opiate withdrawal and the first evidence that novelty seeking, a variable associated with early stages of drug-taking behavior, is also predictive of differences in opiate withdrawal.
MATERIALS AND METHODS
Animals
A total of 234 adult male Sprague–Dawley rats (Charles River Laboratories, Wilmington, MA, USA), weighing approximately 225–250 g upon arrival, were used. Animals were housed three per cage in a room adjacent to the testing room, and maintained on a 12/12 h light/dark cycle (lights on at 0700 hours). Rats were acclimated to the animal quarters for 1 week before any experimental procedure. Experiments were conducted between 1300 and 1700 hours, during the light portion of the cycle. Food and water were available ad libitum. Animals were treated in accordance with National Institutes of Health guidelines on laboratory animal use and care.
Experiment I: Measurement of Somatic Responses to Spontaneous Morphine Withdrawal
Locomotor activity test
After 7 days of habituation to the housing conditions, 24 rats were tested for locomotor activity during a 60 min exposure to the mild stress of a novel environment. Each rat was placed in a 43L × 21.5 W × 24.5 H (in cm) clear acrylic activity monitor and locomotor activity was monitored by means of two banks of photocells connected to a microprocessor. Rats that exhibited locomotor counts in the highest third of the sample were classified as HR (n=8), whereas rats that exhibited locomotor counts in the lowest third of the sample were classified as LR (n=8).
Induction of physical dependence and spontaneous morphine withdrawal
The morphine regimen used to induce dependence was a slightly modified version of the protocol previously used by Cicero et al (2002). Morphine (morphine sulfate, Mayne Pharma, Paramus, NJ) was injected intraperitoneally (i.p.) twice daily at approximately 0000 and 1200 hours. The morphine dose per injection was progressively increased from 5 to 40 mg/kg over a period of 14 days. Beginning 24 h after the last injection, and continuing at daily intervals for 6 days, animals were placed in testing chambers (24 cm diameter × 50 cm height), and occurrences of teeth chattering, wet dog shakes, paw tremors, genital grooming, and writhing were recorded for a 30 min period on each day. Animals' body weight was also monitored during the whole experiment. A global withdrawal score was calculated according to a slightly modified rating scale described by Blasig et al (1973). For counted signs: a score of 2 was allocated if there were one or two wet dog shakes and a score of 4 if there were three or more wet dog shakes; a score of 2 was allocated for each writhing episode; and finally, a score of 1 was allocated for each 1% loss in body weight. For checked signs: a score of 2 was allocated to the presence of teeth chattering and a score of 3 to the presence of genital grooming and paw tremors.
Experiment II: Measurement of Somatic Responses to Naltrexone-Precipitated Morphine Withdrawal
This experiment was designed to compare somatic responses to naltrexone (NTX)-precipitated morphine withdrawal in HR vs LR animals. Rapid detoxification by combination of clonidine and NTX has been successful as an alternative to more classical detoxification protocols (for review see Kosten and O'Connor, 2003). Comparison of somatic responses in HR vs LR animals during spontaneous and NTX-precipitated withdrawal could provide insight into the reasons for biological variability in the responsiveness to different detoxification protocols. Moreover, precipitated withdrawal triggers a more profound and quantifiable abstinence syndrome that allows the analysis of more somatic signs, including eye twitching and jumping behaviors.
Twenty-one rats were habituated to the housing conditions and screened for their locomotor activity as above, generating HR (n=7) and LR (n=7) groups.
One week after the locomotor activity test, HR and LR rats were deeply anesthetized using a 2% V/V mix of isofluorane and oxygen, and implanted subcutaneously in the lower back with two 75-mg morphine pellets (NIDA, Rockville, MD).
Measurement of somatic responses to withdrawal
On day 6 after the surgery, HR and LR animals received an i.p. injection of 1 mg/kg NTX (Delfs et al, 2000) (Sigma, St Louis, MO) and, immediately after the injection, were placed in testing chambers. Instances of teeth chattering, eye twitching, escape jumps, wet dog shakes, paw tremors, genital grooming, and writhing were counted for 30 min, and a global withdrawal score was calculated as above.
Experiment III: Measurement of Place Aversion
In this experiment, we compared withdrawal-induced place aversion in HR vs LR animals.
The place aversion conditioning apparatus consisted of a 80L × 40W × 45H (in cm) box divided equally into two compartments. The first compartment had a smooth clear Plexiglas floor and spots on the walls. The second compartment had a rough metallic floor and black stripes on the walls.
Following the habituation period, 66 rats were tested for locomotor activity and sorted according to their locomotion score as above. One week after the locomotor activity test, HR (n=22) and LR (n=22) animals were implanted subcutaneously in the lower back with two 75 mg morphine pellets to induce morphine dependence also as above.
Preconditioning phase
The protocol for testing of place aversion was similar to the one previously used by Delfs et al (2000). On the fifth day after pellet implantation, each rat was placed in the place aversion apparatus and allowed to explore both compartments of the box for 20 min. The amount of time spent on each side was recorded, and any rat showing a strong preference for either side (more than 85% of the session time) was eliminated from the study. Five rats had to be eliminated for this reason. After preconditioning, HR and LR animals were randomly assigned to one of the following treatment groups: NTX 1, 0.5, or 0.1 mg/kg. The dose of 1 mg/kg is the highest dose found in literature for systemic administration of NTX to induce withdrawal in morphine-dependent rats and it produces a severe withdrawal syndrome (Reti and Baraban, 2003; Aston-Jones et al, 1999; Delfs et al, 2000). Therefore, higher doses were not tested. The experimental design yielded six groups: HR-1 mg/kgNTX, LR-1 mg/kgNTX, HR-0.5 mg/kgNTX, LR-0.5 mg/kgNTX, HR-0.1 mg/kgNTX, and LR-0.1 mg/kgNTX (n=5–8 per group).
Conditioning phase
On the day after preconditioning, HR and LR rats were injected i.p. with either saline or NTX, and immediately confined to one side of the box by means of an opaque Plexiglas divider for 30 min. The next day, animals given NTX on the first day of the conditioning phase were given saline and confined to the opposite side, and vice versa. Equal numbers of animals in each group were assigned to be given NTX in the two different sides. Further, animals within each group were counterbalanced so that half of the animals received the NTX injection on the first day of the conditioning phase and the other half on the second day.
Test phase
Twenty-four hours after day 2 of the conditioning phase, HR and LR animals were given free access to both compartments and the amount of time spent on each side was recorded for 20 min. The difference in the time spent in the NTX-paired compartment during the testing phase vs the preconditioning phase served as an index of place aversion.
Experiment IV: Measurement of mRNA Levels for Adrenergic Receptors in HR vs LR Animals
One week following the locomotor activity test, six HR and six LR animals were euthanized by rapid decapitation, their brain immediately removed, frozen in isopentane cooled to −30 to −40°C, and stored at −80°C.
In situ hybridization for BST and CEA
Presence of mRNA signal has previously been shown for α1a, α1b, α2a, α2c, β1, and β2 adrenergic receptors in BST, and α1a, α1b, and α2a adrenergic receptors in CeA (Nicholas et al, 1993a, 1993b; Pieribone et al, 1994; Scheinin et al, 1994; Day et al, 1997; Domyancic and Morilak, 1997). We compared mRNA levels for these receptors in HR vs LR animals.
The in situ hybridization method used in this study is described in detail by Isgor et al (2003). Briefly, tissue was sectioned at −20°C at a thickness of 12 μm, mounted onto poly(L-lysine)-coated slides, and stored at −80°C until use. Before probe hybridization, tissue was fixed in 4% paraformaldehyde at room temperature, rinsed with aqueous buffers, and dehydrated with graded alcohols. Riboprobes were synthesized with incorporation of 35S-UTP and 35S-CTP and hybridized to tissue overnight at 55°C. Sections were then washed with increasing stringency, dehydrated with graded alcohols, air-dried, and exposed to film. Exposure time was chosen to maximize signal. Sections were then dipped in liquid film emulsion and stored in light-tight boxes. Exposure time was chosen to maximize the detection of radioactive grains, and after sufficient time was elapsed, sections were developed, dehydrated, and coverslipped in a xylene-based mounting medium (Permount, Fisher Scientific, Fair Lawn, NJ).
Riboprobes were synthesized from cDNA fragments generously donated by Dr DM Perez for the α1a adrenergic receptor, by Dr RJ Lefkowitz for the α1b adrenergic receptor, by Dr SM Lanier for the α2a and α2c adrenergic receptors, and by Dr H Shimomura for the β1 adrenergic receptor. A cDNA fragment for the β2 adrenergic receptor was generated in our lab. Signal for β2 mRNA levels detected using the probe was consistent with previously published data (Nicholas et al, 1993a), and the sense probe showed no detectable signal in the brain.
Six tissue sections for each probe were selected for BST (bregma 0.2 to −0.92 mm) and CeA (bregma −1.6 to −2.8 mm) from each animal. Digital images of the brain sections were captured from X-ray films in the linear range of the gray levels using a CCD camera (TM-745, Pulnix, USA). Integrated optical density for adrenergic receptors mRNA was determined for each section using the Micro Computer Imaging Device (Ontario, Canada) image analysis system. For each animal, data from multiple sections were averaged to obtain a representative value (mean integrated density).
In situ hybridization for β1 mRNA levels in the lateral, medial, and ventral BST
Significant differences in β1 mRNA levels were detected between HR and LR animals in BST. In order to better identify the specific region of the BST in which HR and LR animals differed in β1 receptors expression, the BST was further divided into three subregions: a lateral subdivision (BSTl) consisting of the BST lateral division dorsal, intermediate, juxtacapsular, and posterior parts; a medial subdivision (BSTm) containing the BST medial division anterior and posterior parts; and a ventral subdivision (BSTv) consisting of the lateral and medial division ventral parts as defined in the Paxinos and Watson rat brain atlas (Paxinos and Watson, 1998) (see Figure 1). Image analysis was conducted as above.
In situ hybridization for β1 mRNA levels in the CA1 subregion of the hippocampus, the cingulated cortex, and the medial habenula
Finally, to investigate the specificity of the difference found, we compared β1 mRNA levels in HR vs LR animals in the CA1 subregion of the hippocampus (bregma −2.3 to −3.6 mm), the cingulated cortex (Cin Cx; bregma 0.7 to −0.4 mm), and the medial habenula (MHA; bregma −3.14 to −4.3 mm), brain regions that show high β1 mRNA levels and are activated during morphine withdrawal (Kimes et al, 1990; Frenois et al, 2002). Again, six tissue sections for each brain region were selected, and data from multiple sections were averaged to obtain a representative value for each rat.
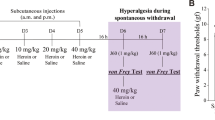
Experiment V: Effects of the Microinjection of the β1 Antagonist Betaxolol in the Dorsal BST on Behavioral Symptoms and Aversiveness Induced by Morphine Withdrawal in HR vs LR Animals
This experiment was designed to investigate whether bilateral microinjection of the selective β1 antagonist betaxolol into dorsal BST would differentially affect somatic symptoms of withdrawal and aversion scores in HR vs LR animals.
Surgery
One week after 105 rats were sorted according to their locomotor activity, HR (n=35) and LR (n=35) rats were anesthetized using isoflurane and implanted subcutaneously with two 75-mg morphine pellets. Rats were then placed in a stereotaxic frame with the incisor bar set at −3.3 mm. Guide cannulae (Plastics One Inc., VA, USA) were implanted bilaterally, so as to position the tips 1.5 mm above the dorsal BST (coordinates from bregma: AP−0.4 mm, ML±3.3 mm, DV−5.2 mm, approached at a 15° angle laterally). The guide cannulae were anchored to the skull with four jeweler's screws and acrylic dental cement, and fitted with obdurators (Plastics One Inc.) to maintain patency. Behavioral testing began 5 days after surgery.
CPA and opiate withdrawal behavioral scoring
The preconditioning phase was conducted as in experiment III. Thirteen animals spent more than 85% of the session time in one side of the box and were eliminated from the study. At the end of preconditioning, animals were randomly assigned to one of the following groups: vehicle (VEH), betaxolol low dose (BLD), or betaxolol high dose (BHD). During the conditioning days of the test, rats in the VEH groups received a bilateral microinjection of 0.3 μl of saline into the dorsal BST, rats in the BLD groups received a bilateral microinjection of 0.2 nmol of betaxolol/0.3 μl of saline, and rats in the BHD groups received a bilateral microinjection of 1 nmol of betaxolol/0.3 μl of saline. Injections were made using a Hamilton syringe mounted on a syringe pump (Harvard Apparatus, MA, USA) at a rate of 0.3 μl/min, 5 min before the animals received their i.p. injection of either saline or 1 mg/kg NTX. The injectors were left in place an additional 3 min at the end of the microinjection. During withdrawal, occurrences of teeth chattering, wet dog shakes, escape jumps, paw tremors, genital grooming, and writhing were scored for each rat.
Testing for CPA was conducted as described under experiment III.
Histology
At the end of the 20 min place aversion test, the animals were euthanized via rapid decapitation. Brains were harvested, frozen in isopentane (−30 to −40°C), and stored at −80°C. Placements of the microinjection cannulae tracks were verified histologically. Brains were sectioned coronally on a cryostat (section thickness=20 μm) throughout the BST. Slide-mounted sections were then stained with Cresyl Violet for cannulae placement determinations.
Statistical Analysis
Data for withdrawal symptoms in experiment I were analyzed using a two-way analysis of variance (ANOVA) with repeated measures. The factors of variation were group (HR or LR; between subjects) and observation session (days 1–6; within subjects). When a significant difference between groups was observed, Newman–Keuls test for post hoc comparisons was used in order to determine differences in each session.
Data for withdrawal symptoms in experiment II, and for experiment IV were analyzed using Student's unpaired t-test. As multiple t-tests were performed on the same animals, a Bonferroni correction for multiple t-tests was applied.
Results from experiment III were analyzed using a two-way ANOVA. The factors of variation were group (HR or LR) and NTX dose (1, 0.5, or 0.1 mg/kg).
Data from experiment V were analyzed using Student's unpaired t-test to compare HR and LR animals in the same drug treatment group.
For global withdrawal score data in experiments I and II, the assumption of normality was violated. As there is no equivalent non-parametric test of two-way ANOVA with repeated measures, data for global withdrawal score in experiment I were analyzed using the procedure of Conover (1999): two-way ANOVA with repeated measures was performed on error values as well as ranks. If the two procedures gave nearly identical results, the parametric analysis was considered to be valid. Data for global withdrawal score in experiment II were analyzed using Mann–Whitney U-test.
RESULTS
Experiment I: Measurement of Somatic Responses to Spontaneous Morphine Withdrawal
Statistical comparison of global withdrawal score for somatic responses to spontaneous withdrawal in HR vs LR animals revealed very similar results for error values and ranks, with a significant time effect (F1,5=25.204, p<0.01 and F1,5=24.87, p<0.01 for error values and ranks, respectively), and no significant group effect or time × group interaction effect (see Figure 2a). However, it is critical to analyze individual withdrawal signs, as they are mediated by different neuronal circuits.
Somatic signs during spontaneous withdrawal in HR and LR animals. Data are from six daily 30 min observation sessions, starting at 24 h after the last morphine injection. (a) Global withdrawal score in HR and LR animals in the 6 days following cessation of chronic morphine injections. (b) Teeth chattering episodes in HR and LR animals following cessation of twice daily injections of morphine. Values are mean±SEM (n=7–8 animals per group). *p<0.05. ANOVA for repeated measures followed by Newman–Keuls test for post hoc comparisons.
The most prominent sign of spontaneous morphine withdrawal was teeth chattering, followed by wet dog shakes, genital grooming, paw tremors, and writhing as the least frequent behavior observed.
Statistical analyses revealed a significant time × group interaction effect for teeth chattering episodes (F5,65=2.414, p<0.05). Subsequent post hoc analyses indicated that HR animals had a significantly higher number of teeth chattering episodes than LR animals on day 1 of the spontaneous withdrawal, with no difference between the two groups in the following 5 days (see Figure 2b). A significant time effect, with no significant group effect or time × group interaction effect, was observed for wet dog shakes (F1,5=14.283, p<0.01), genital grooming (F1,5=2.641, p<0.05), and paw tremors (F1,5=4.686, p<0.01) episodes. No statistically significant effects were present for writhing (data not shown). Finally, analysis of animals' body weight changes during withdrawal revealed a significant effect of time (F1,5=67.43, p<0.01) with no significant group effect or time × group interaction effect.
Experiment II: Measurement of Somatic Responses to NTX-Precipitated Morphine Withdrawal
Here again, comparison of the global score for withdrawal-induced somatic responses in HR vs LR animals did not show statistical difference between the two groups of animals (data not shown).
The most prominent signs of NTX-precipitated withdrawal were eye twitching and teeth chattering, followed by wet dog shakes, escape jumps, paw tremors, genital grooming, and writhing as the least frequent behavior observed (see Figure 3).
Somatic signs during precipitated withdrawal in HR and LR animals. ET, eye twitching; TC, teeth chattering; WDS, wet dog shakes; JMP, escape jumps; PT, paw tremors; GG, genital grooming; WR, writhing. All data are mean±SEM (n=6–7 animals per group). *p<0.05. Student's t-test followed by Bonferroni correction for multiple t-tests.
Statistical analysis revealed significantly higher number of eye twitching and teeth chattering episodes in HR than in LR animals during NTX-precipitated withdrawal (t=3.453, p<0.05 and t=3.502, p<0.05 after Bonferroni correction, respectively). By contrast, no significant differences were present between the two groups of animals in the number of wet dog shakes, escape jumps, paw tremors, genital grooming, and writhing episodes (see Figure 3).
Experiment III: Measurement of Place Aversion
During the preconditioning phase of the test, animals did not show any significant preference for either compartment of the place aversion box, with an average time spent in the compartment with Plexiglas floor of 584±27 SEM seconds and an average time spent in the compartment with metallic floor of 616±27 SEM seconds. After conditioning, both HR and LR animals showed aversion to the side paired with NTX. This effect was dose-dependent with higher aversion scores in the animals injected with the highest dose of NTX, although this trend failed to reach significance owing to variability (F2,33=1.124, p>0.33). Importantly, aversion scores in HR and LR animals were nearly identical, and ANOVA indicated no significant effects for the HR–LR dimension (F1, 33=0.04, p>0.83), nor any significant group × treatment interaction (F2, 33=0.005, p>0.99) (see Table 1).
Experiment IV: Quantification of mRNA Levels for Adrenergic Receptors in the BST and CeA of HR and LR Animals
When adrenergic receptor mRNA levels in the BST and CeA of HR vs LR rats were compared, statistical analysis showed that HR animals have significantly higher β1 adrenergic receptor mRNA levels in the BST than in LR animals (t=4.337, p<0.01 after Bonferroni correction). No other significant differences were found in BST or CeA (see Figure 4).
Adrenergic receptors mRNA levels in the BST and CeA of HR and LR animals as measured by in situ hybridization. (a) Integrated optical density for α1a, α1b, α2a, α2c, β1, and β2 adrenergic receptors mRNA levels in the BST in HR vs LR animals. (b) Integrated optical density for α1a, α1b, and α2a adrenergic receptors mRNA levels in the CeA in HR vs LR animals. (c) Representative coronal sections showing mRNA signal for β1 (top) and β2 (bottom) adrenergic receptors in the BST of HR and LR animals as measured by in situ hybridization. AC, anterior commissure. All values are mean±SEM (n=6 animals per group). **p<0.01. Student's t-test followed by Bonferroni correction for multiple t-tests.
Dark-field autoradiographs of the BST after in situ hybridization for the β1 adrenergic receptor showed widespread labeling throughout the BST, with slightly higher signal in the posterior portion of the nucleus (see Figure 5).
Dark-field autoradiographs of silver grains representing labeling with β1 probe in the BST at coronal planes 0.2 mm anterior, and 0.26, 0.4, and 0.92 posterior to bregma. Signal is present throughout the BST, and it is slightly stronger in the posterior section of the nucleus. 3v, third ventricle; ac, anterior commissure; j, BST juxtacapsular; la, BST lateral anterior; ld, BST lateral dorsal; li, BST lateral intermediate; lp, BST lateral posterior; lv, BST lateral ventral; ma, BST medial anterior; mv, BST medial ventral; pi, BST medial posterointermediate; pl, BST medial posterolateral; pm, BST medial posteromedial (Paxinos and Watson, 1998). Scale bar=500 μm.
When β1 mRNA levels were compared in HR vs LR animals in the lateral, medial, and ventral subdivision of the BST, statistical analysis revealed significantly higher β1 mRNA levels in HR than in LR animals in the BSTl (t=6.052, p<0.01 after Bonferroni correction) and BSTm (t=3.841, p<0.01 after Bonferroni correction) but not BSTv (see Table 2).
Finally, subsequent comparison of β1 adrenergic receptor mRNA levels in CA1, Cin Cx, and MHA in HR vs LR animals showed no significant differences between the two groups of animals in any of the brain regions (see Figure 6).
β1 adrenergic receptors mRNA levels in the CA1, Cin Cx, and MHA of HR and LR animals as measured by in situ hybridization. (a) Representative coronal sections showing mRNA signal for the β1 adrenergic receptor in the CA1 subregion of the hippocampus (top), the Cin Cx (middle), and the MHA (bottom) in HR and LR animals as measured by in situ hybridization. Scale bar=1 mm. (b) Integrated optical density for β1 adrenergic receptors mRNA levels in the CA1, Cin Cx, and MHA of HR vs LR animals. All values are mean±SEM (n=6 animals per group). Student's t-test.
Experiment V: Effects of the Microinjection of the β1 Selective Antagonist Betaxolol in the Dorsal BST on Somatic Symptoms and Place Aversion Induced by Morphine Withdrawal in HR vs LR Animals
Statistical comparisons for behavioral symptoms during NTX-induced withdrawal in HR vs LR animals revealed a significantly higher number of teeth chattering episodes in HR-VEH than LR-VEH animals (t=2.271, p<0.05); bilateral microinjection of betaxolol into dorsal BST dose-dependently reduced the difference between HR and LR animals to a nonsignificant level (see Figure 7a). No significant effects were present for the other behavioral symptoms scored (data not shown).
Effects of bilateral microinjection of the β1 selective antagonist betaxolol into the dorsal BST on opioid withdrawal. (a) Effects of bilateral microinjection of betaxolol on teeth chattering episodes. (b) Effects of bilateral microinjection of betaxolol on CPA. Values are mean±SEM (n=5–9 animals per group). *p<0.05 compared to HR animals in the same treatment group. Student's t-test.
In the place aversion test, statistical analyses of aversion score during NTX-induced withdrawal showed no significant difference in HR-VEH vs LR-VEH animals. Bilateral microinjection of betaxolol into dorsal BST dose-dependently blocked aversion in HR animals. As a consequence, aversion score was significantly lower in HR-BHD than LR-BHD animals (t=2.275, p<0.05; see Figure 7b).
Both successful placements and misplacements of cannulae tips are illustrated in Figure 8. Eleven animals were eliminated from all analyses because of histology. Eight animals were eliminated because of damage to the lateral ventricle during drug microinjection, two animals because of single cannula misplacement, and one because of double cannula misplacement. Of the animals eliminated, three animals were in the HR-BHD group. In two of these animals, cannula tips were properly positioned in the BST, but the lateral ventricle was damaged; results from these rats were similar to those of animals in the HR-BHD group with proper cannulae placement. The other animal had both cannula tips located in the caudate putamen, dorsal to the BST; results from this rat were similar to those from rats in the HR-VEH group with proper cannulae placement. Results from the other eight animals eliminated were, as expected, similar to those of vehicle-microinjected animals in the same group.
DISCUSSION
This series of studies demonstrated that (a) greater novelty-seeking behavior predicts an increase in some somatic signs of opioid withdrawal, particularly teeth chattering and, during precipitated withdrawal, eye twitching episodes; (b) relative to LR, HR animals exhibit higher β1 receptor mRNA levels in the medial and lateral BST. This differential expression is molecularly selective, as expression levels of other types of adrenergic receptors were equivalent between HR and LR rats. It is also regionally selective, as β1 receptor expression was comparable between HR and LR in all other brain regions tested; (c) the HR–LR β1 receptor difference is functionally significant in controlling somatic symptoms, as a selective β1 receptor antagonist, betaxolol, microinjected into the dorsal BST decreased teeth chattering episodes in HR to levels observed in LR animals; (d) this differential expression is also functionally significant in mediating the affective aspects of opiate withdrawal, as betaxolol was significantly more effective in reversing place aversion in the HR animals.
The number of teeth chattering episodes was higher in HR animals during both spontaneous and NTX-precipitated withdrawal, indicating that the route of morphine administration (i.p. or pellets), or the use of NTX to precipitate withdrawal, is not responsible for this behavioral difference. By contrast, eye twitching, a less robust abstinence measure, was difficult to observe reliably under spontaneous withdrawal. It was quantifiable under precipitated withdrawal, where it was significantly higher in HR animals. These observations are consistent with the previous finding that these two somatic abstinence signs are modulated in the BST (Delfs et al, 2000).
Microinjection of the selective β1 receptor antagonist betaxolol into dorsal BST eliminated the difference in withdrawal-induced teeth chattering episodes between HR and LR animals, demonstrating that β1 receptors in this part of the BST are critical in mediating individual differences in this sign. The HR–LR difference in teeth chattering disappears 48 h after spontaneous withdrawal, suggesting that adaptive changes occur during that period. Interestingly, the number of brain α2 adrenergic receptors progressively increases during morphine withdrawal (Smith et al, 1989; Gabilondo and Garcia-Sevilla, 1995). This compensatory increase could inhibit withdrawal-induced norepinephrine (NE) release in the BST and dampen its behavioral consequences. Moreover, a possible downregulation of postsynaptic β1 receptors in the dorsal BST owing to the sustained increase in NE release during withdrawal could contribute to eliminate the differences in teeth chattering episodes in HR vs LR animals seen on the first day of spontaneous withdrawal.
Importantly, we demonstrated the impact of the selective β1 receptor antagonist betaxolol on the motivational aspects of opiate withdrawal. Although HR and LR rats did not differ in their aversion scores under any NTX doses tested, microinjection of betaxolol into dorsal BST was more effective in reversing place aversion in HR than LR animals. It is conceivable that higher doses of betaxolol would become effective in LR rats; however, 1 nmol is the highest dose that selectively blocks β1 receptor without compromising receptor selectivity (Aston-Jones et al, 1999; Cecchi et al, 2002; Leri et al, 2002).
How is it that HR and LR rats have similar place aversion scores and yet have such a differential sensitivity to betaxolol? And how can betaxolol pretreatment cause a profound reduction in place aversion in HR rats even though it blocks only a subset of their somatic signs?
It is likely that HR and LR animals activate somewhat different circuits involved in opiate withdrawal, both for somatic and affective responses. Distinct circuits are indeed responsible for somatic and aversive signs of opioid withdrawal (Mucha, 1987; Delfs et al, 2000; Frenois et al, 2002). Some brain structures, including extended amygadala, basolateral amygadala, lateral septum, and hippocampal CA1, express c-fos mRNA during withdrawal aversion in the absence of somatic signs. Other structures, including dopaminergic and noradrenergic nuclei, motor striatal areas, hypothalamus, and periaqueductal gray, are recruited when a full withdrawal syndrome is observed (Frenois et al, 2002). The fact that place aversion can be significantly blocked when only some components of the somatic syndrome are inhibited supports the view that unique neural mechanisms encode the affective response to abstinence. Our findings underscore the fact that this affective response is differentially mediated in two groups of animals that have differing vulnerabilities to drug self-administration, and identify β1 receptor as a molecular mediator of this affective difference.
Are there other differences in the noradrenergic system that may participate in this differential responsiveness to opiate abstinence? Retrograde tract-tracing studies in morphine-dependent rats after NTX-precipitated opiate withdrawal show that noradrenergic cells stimulated by opioid withdrawal and projecting to the BST are prominently located in the nucleus tractus solitarius (NTS) (Aston-Jones et al, 1999). As a consequence of the noradrenergic system activation, NE extracellular levels in the BST are elevated during withdrawal (Fuentealba et al, 2000) and produce an activation of the dorsolateral and ventral parts of the BST that is blockable by β antagonists (Aston-Jones et al, 1999; Gracy et al, 2001). We studied basal expression of several catecholamine-related molecules in the locus coeruleus and NTS of HR and LR animals (in preparation). No differences in tyrosine hydroxylase (TH), dopamine β-hydroxylase, α2a presynaptic adrenergic receptor, or NE transporter mRNA levels were observed in locus coeruleus. In NTS, only TH mRNA was differentially expressed, and was higher in LR animals. As NTS projects to the BST and is activated during withdrawal, and as increased TH expression may result in increased NE levels, this could cause the downregulation in β1 receptor seen in LR animals. Further studies are needed to analyze the differential regulation of this system in conjunction with differences in opiate abstinence.
What is the likely mechanism whereby a difference in β1 receptor expression leads to HR–LR differences in abstinence? Neurons from the dorsolateral BST, likely inhibitory, heavily innervate the ventral BST (Dong et al, 2001), which in turn sends excitatory projections to dopamine (DA) neurons in the ventral tegmental area (Georges and Aston-Jones, 2002; Dumont and Williams, 2004). Thus, β1 receptors would inhibit accumbal DA activity indirectly, contributing to the decrease in DA release associated with withdrawal (Acquas et al, 1991; Pothos et al, 1991; Rossetti et al, 1992; Diana et al, 1995; Stella et al, 2003). Because of their differential expression, β1 receptors would play a larger role in HR than LR animals.
It is conceivable that β1 adrenergic receptors in the dorsal BST could regulate withdrawal-induced aversiveness through the CeA, as this structure receives heavy innervation from the dorsolateral BST (Dong et al, 2001), and is implicated in the affective response to opiate withdrawal (Gracy et al, 2001; Watanabe et al, 2002, 2003). However, electrical stimulation of the CeA fails to affect DA release in the nucleus accumbens (Howland et al, 2002), making BST regulation of affective aspects of withdrawal through CeA less likely. It is more likely that the CeA mediates the β1 adrenergic modulation of somatic withdrawal signs. Indeed, the CeA receives a range of sensory information from ascending and descending inputs (Swanson and Petrovich, 1998), and projects heavily to autonomic centers including the dorsal motor nucleus of the vagus, NTS, parabrachial nucleus, and trigeminal pre-motor neurons (Hopkins and Holstege, 1978; Yasui et al, 2004)—circuits that mediate the somatic signs of opioid withdrawal.
Within the BST, is β adrenergic control over the affective and somatic aspects of withdrawal mediated by the same neuronal populations? The BST contains multiple peptide populations coexpressed in GABAergic neurons, with the clearest separation between corticotropin-releasing factor (CRF)-expressing and enkephalin-expressing populations (Day et al, 1999). Microinjection of β antagonists into BST blocks anxiety-like behavior in the elevated plus-maze, and reduces stress-induced reinstatement of drug-seeking behavior (Cecchi et al, 2002; Leri et al, 2002). These effects are likely exerted through noradrenergic regulation of CRF-containing cells (Hornby and Piekut, 1989; Phelix et al, 1994; Lee and Davis, 1997; Erb and Stewart, 1999). It is therefore reasonable to suggest that BST CRF neurons would mediate the affective aspects of opiate withdrawal. By contrast, NE regulation of somatic signs is likely mediated by enkephalin-positive neurons within the BST. Enkephalin, but not CRF, neurons display a c-fos response after precipitated withdrawal (Veinante et al, 2003; Hamlin et al, 2004). Importantly, microinjection of a CRF antagonist into BST does not affect the severity or somatic signs of opiate withdrawal (McNally and Akil, 2002). It is therefore likely that somatic aspects of opioid withdrawal on the one hand and affective component on the other are modulated via distinct, NE-sensitive circuits within the BST.
The sustained negative affect associated with drug abstinence is worthy of careful study as it may cause relapse. Whether β1 receptors in one or more neuronal populations within the BST participate in individual differences in the long-term affective consequences of withdrawal remains to be investigated.
Conclusions
The present study provides novel evidence of a link between β1 adrenergic receptors in the dorsal BST and individual differences in opioid withdrawal. This suggests that a focus on β1 adrenergic drugs might be valuable in treatment of human opiate addicts. Our work further suggests that the novelty-seeking dimension, previously associated with initial drug-seeking behavior, is also related to differences in opiate withdrawal. The homologous dimension in humans, sensation-seeking behavior, has been widely studied and related to various personality traits and propensity for substance abuse (Zuckerman and Neeb, 1979; Cloninger, 1987). The examination of this variable in relation to the symptoms and treatment response during heroin withdrawal would be of great interest. The study of individual differences in opioid withdrawal in rats represents a new animal model for understanding the neural mechanisms underlying differences in human withdrawal and the propensity for continued substance abuse in some individuals.
References
Acquas E, Carboni E, Di Chiara G (1991). Profound depression of mesolimbic dopamine release after morphine withdrawal in dependent rats. Eur J Pharmacol 193: 133–134.
Ambrosio E, Goldberg SR, Elmer GI (1995). Behavior genetic investigation of the relationship between spontaneous locomotor activity and the acquisition of morphine self-administration behavior. Behav Pharmacol 6: 229–237.
Aston-Jones G, Delfs JM, Druhan J, Zhu Y (1999). The bed nucleus of the stria terminalis. A target site for noradrenergic actions in opiate withdrawal. Ann NY Acad Sci 877: 486–498.
Aston-Jones G, Harris GC (2004). Brain substrates for increased drug seeking during protracted withdrawal. Neuropharmacology 47(Suppl 1): 167–179.
Blasig J, Herz A, Reinhold K, Zieglgansberger S (1973). Development of physical dependence on morphine in respect to time and dosage and quantification of the precipitated withdrawal syndrome in rats. Psychopharmacologia 33: 19–38.
Cecchi M, Khoshbouei H, Javors M, Morilak DA (2002). Modulatory effects of norepinephrine in the lateral bed nucleus of the stria terminalis on behavioral and neuroendocrine responses to acute stress. Neuroscience 112: 13–21.
Cicero TJ, Nock B, Meyer ER (2002). Gender-linked differences in the expression of physical dependence in the rat. Pharmacol Biochem Behav 72: 691–697.
Cloninger CR (1987). A systematic method for clinical description and classification of personality variants. A proposal. Arch Gen Psychiat 44: 573–588.
Conover WJ (1999). Practical Nonparametric Statistics. Wiley: New York.
Day HE, Campeau S, Watson Jr SJ, Akil H (1997). Distribution of alpha 1a-, alpha 1b- and alpha 1d-adrenergic receptor mRNA in the rat brain and spinal cord. J Chem Neuroanat 13: 115–139.
Day HE, Curran EJ, Watson Jr SJ, Akil H (1999). Distinct neurochemical populations in the rat central nucleus of the amygdala and bed nucleus of the stria terminalis: evidence for their selective activation by interleukin-1beta. J Comp Neurol 413: 113–128.
De Vries TJ, Shippenberg TS (2002). Neural systems underlying opiate addiction. J Neurosci 22: 3321–3325.
Delfs JM, Zhu Y, Druhan JP, Aston-Jones G (2000). Noradrenaline in the ventral forebrain is critical for opiate withdrawal-induced aversion. Nature 403: 430–434.
Deroche V, Piazza PV, Le Moal M, Simon H (1993). Individual differences in the psychomotor effects of morphine are predicted by reactivity to novelty and influenced by corticosterone secretion. Brain Res 623: 341–344.
Diana M, Pistis M, Muntoni A, Gessa G (1995). Profound decrease of mesolimbic dopaminergic neuronal activity in morphine withdrawn rats. J Pharmacol Exp Ther 272: 781–785.
Domyancic AV, Morilak DA (1997). Distribution of alpha1A adrenergic receptor mRNA in the rat brain visualized by in situ hybridization. J Comp Neurol 386: 358–378.
Dong HW, Petrovich GD, Watts AG, Swanson LW (2001). Basic organization of projections from the oval and fusiform nuclei of the bed nuclei of the stria terminalis in adult rat brain. J Comp Neurol 436: 430–455.
Dumont EC, Williams JT (2004). Noradrenaline triggers GABAA inhibition of bed nucleus of the stria terminalis neurons projecting to the ventral tegmental area. J Neurosci 24: 8198–8204.
Erb S, Stewart J (1999). A role for the bed nucleus of the stria terminalis, but not the amygdala, in the effects of corticotropin-releasing factor on stress-induced reinstatement of cocaine seeking. J Neurosci 19: RC35.
Frenois F, Cador M, Caille S, Stinus L, Le Moine C (2002). Neural correlates of the motivational and somatic components of naloxone-precipitated morphine withdrawal. Eur J Neurosci 16: 1377–1389.
Fuentealba JA, Forray MI, Gysling K (2000). Chronic morphine treatment and withdrawal increase extracellular levels of norepinephrine in the rat bed nucleus of the stria terminalis. J Neurochem 75: 741–748.
Gabilondo AM, Garcia-Sevilla JA (1995). Spontaneous withdrawal from long-term treatment with morphine accelerates the turnover of alpha 2-adrenoceptors in the rat brain: up-regulation of receptors associated with increased receptor appearance. J Neurochem 64: 2590–2597.
Georges F, Aston-Jones G (2002). Activation of ventral tegmental area cells by the bed nucleus of the stria terminalis: a novel excitatory amino acid input to midbrain dopamine neurons. J Neurosci 22: 5173–5187.
Gowing LR, Farrell M, Ali RL, White JM (2002). Alpha2-adrenergic agonists in opioid withdrawal. Addiction 97: 49–58.
Gracy KN, Dankiewicz LA, Koob GF (2001). Opiate withdrawal-induced fos immunoreactivity in the rat extended amygdala parallels the development of conditioned place aversion. Neuropsychopharmacology 24: 152–160.
Gutstein HB, Akil H (2001). Opioid analgesics. In: Hardman JG, Limbird LE, Goodman Gilman A (eds). The Pharmacological Basis of Therapeutics, 10th edn. McGraw-Hill: New York, NY. pp 569–619.
Hamlin AS, Buller KM, Day TA, Osborne PB (2004). Effect of naloxone-precipitated morphine withdrawal on c-fos expression in rat corticotropin-releasing hormone neurons in the paraventricular hypothalamus and extended amygdala. Neurosci Lett 362: 39–43.
Hopkins DA, Holstege G (1978). Amygdaloid projections to the mesencephalon, pons and medulla oblongata in the cat. Exp Brain Res 32: 529–547.
Hornby PJ, Piekut DT (1989). Opiocortin and catecholamine input to CRF-immunoreactive neurons in rat forebrain. Peptides 10: 1139–1146.
Howland JG, Taepavarapruk P, Phillips AG (2002). Glutamate receptor-dependent modulation of dopamine efflux in the nucleus accumbens by basolateral, but not central, nucleus of the amygdala in rats. J Neurosci 22: 1137–1145.
Isgor C, Cecchi M, Kabbaj M, Akil H, Watson SJ (2003). Estrogen receptor beta in the paraventricular nucleus of hypothalamus regulates the neuroendocrine response to stress and is regulated by corticosterone. Neuroscience 121: 837–845.
Kabbaj M, Isgor C, Watson SJ, Akil H (2002). Stress during adolescence alters behavioral sensitization to amphetamine. Neuroscience 113: 395–400.
Kabbaj M, Norton CS, Kollack-Walker S, Watson SJ, Robinson TE, Akil H (2001). Social defeat alters the acquisition of cocaine self-administration in rats: role of individual differences in cocaine-taking behavior. Psychopharmacology (Berlin) 158: 382–387.
Kimes AS, Bell JA, London ED (1990). Clonidine attenuates increased brain glucose metabolism during naloxone-precipitated morphine withdrawal. Neuroscience 34: 633–644.
Kosten TR, O'Connor PG (2003). Management of drug and alcohol withdrawal. N Engl J Med 348: 1786–1795.
Lee Y, Davis M (1997). Role of the hippocampus, the bed nucleus of the stria terminalis, and the amygdala in the excitatory effect of corticotropin-releasing hormone on the acoustic startle reflex. J Neurosci 17: 6434–6446.
Leri F, Flores J, Rodaros D, Stewart J (2002). Blockade of stress-induced but not cocaine-induced reinstatement by infusion of noradrenergic antagonists into the bed nucleus of the stria terminalis or the central nucleus of the amygdala. J Neurosci 22: 5713–5718.
McNally GP, Akil H (2002). Role of corticotropin-releasing hormone in the amygdala and bed nucleus of the stria terminalis in the behavioral, pain modulatory, and endocrine consequences of opiate withdrawal. Neuroscience 112: 605–617.
Mucha RF (1987). Is the motivational effect of opiate withdrawal reflected by common somatic indices of precipitated withdrawal? A place conditioning study in the rat. Brain Res 418: 214–220.
Nicholas AP, Pieribone VA, Hokfelt T (1993a). Cellular localization of messenger RNA for beta-1 and beta-2 adrenergic receptors in rat brain: an in situ hybridization study. Neuroscience 56: 1023–1039.
Nicholas AP, Pieribone V, Hokfelt T (1993b). Distributions of mRNAs for alpha-2 adrenergic receptor subtypes in rat brain: an in situ hybridization study. J Comp Neurol 328: 575–594.
O'Connor PG, Carroll KM, Shi JM, Schottenfeld RS, Kosten TR, Rounsaville BJ (1997). Three methods of opioid detoxification in a primary care setting. A randomized trial. Ann Intern Med 127: 526–530.
Paxinos G, Watson C (1998). The Rat Brain in Stereotaxic Coordinates, 4th edn. Academic Press: San Diego.
Phelix CF, Liposits Z, Paull WK (1994). Catecholamine–CRF synaptic interaction in a septal bed nucleus: afferents of neurons in the bed nucleus of the stria terminalis. Brain Res Bull 33: 109–119.
Piazza PV, Deminiere JM, Le Moal M, Simon H (1989). Factors that predict individual vulnerability to amphetamine self-administration. Science 245: 1511–1513.
Pieribone VA, Nicholas AP, Dagerlind A, Hokfelt T (1994). Distribution of alpha 1 adrenoceptors in rat brain revealed by in situ hybridization experiments utilizing subtype-specific probes. J Neurosci 14: 4252–4268.
Pothos E, Rada P, Mark GP, Hoebel BG (1991). Dopamine microdialysis in the nucleus accumbens during acute and chronic morphine, naloxone-precipitated withdrawal and clonidine treatment. Brain Res 566: 348–350.
Reti IM, Baraban JM (2003). Opiate withdrawal induces Narp in the extended amygdala. Neuropsychopharmacology 28: 1606–1613.
Rossetti ZL, Hmaidan Y, Gessa GL (1992). Marked inhibition of mesolimbic dopamine release: a common feature of ethanol, morphine, cocaine and amphetamine abstinence in rats. Eur J Pharmacol 221: 227–234.
Scheinin M, Lomasney JW, Hayden-Hixson DM, Schambra UB, Caron MG, Lefkowitz RJ et al (1994). Distribution of alpha 2-adrenergic receptor subtype gene expression in rat brain. Brain Res Mol Brain Res 21: 133–149.
Senay EC, Dorus W, Goldberg F, Thornton W (1977). Withdrawal from methadone maintenance. Rate of withdrawal and expectation. Arch Gen Psychiat 34: 361–367.
Smith CB, Moises HC, Spengler RN, Hollingsworth PJ (1989). Changes in alpha 2-adrenoceptor number and function in brains of morphine-dependent rats. Eur J Pharmacol 161: 111–119.
Stella L, De Novellis V, Vitelli MR, Capuano A, Mazzeo F, Berrino L et al (2003). Interactive role of adenosine and dopamine in the opiate withdrawal syndrome. Naunyn Schmiedebergs Arch Pharmacol 368: 113–118.
Stine SM, Southwick SM, Petrakis IL, Kosten TR, Charney DS, Krystal JH (2002). Yohimbine-induced withdrawal and anxiety symptoms in opioid-dependent patients. Biol Psychiat 51: 642–651.
Swanson LW, Petrovich GD (1998). What is the amygdala? Trends Neurosci 21: 323–331.
Veinante P, Stoeckel ME, Lasbennes F, Freund-Mercier MJ (2003). c-Fos and peptide immunoreactivities in the central extended amygdala of morphine-dependent rats after naloxone-precipitated withdrawal. Eur J Neurosci 18: 1295–1305.
Watanabe T, Nakagawa T, Yamamoto R, Maeda A, Minami M, Satoh M (2003). Involvement of noradrenergic system within the central nucleus of the amygdala in naloxone-precipitated morphine withdrawal-induced conditioned place aversion in rats. Psychopharmacology (Berlin) 170: 80–88.
Watanabe T, Yamamoto R, Maeda A, Nakagawa T, Minami M, Satoh M (2002). Effects of excitotoxic lesions of the central or basolateral nucleus of the amygdala on naloxone-precipitated withdrawal-induced conditioned place aversion in morphine-dependent rats. Brain Res 958: 423–428.
Yasui Y, Tsumori T, Oka T, Yokota S (2004). Amygdaloid axon terminals are in contact with trigeminal premotor neurons in the parvicellular reticular formation of the rat medulla oblongata. Brain Res 1016: 129–134.
Zuckerman M, Neeb M (1979). Sensation seeking and psychopathology. Psychiat Res 1: 255–264.
Acknowledgements
This work was supported by NIDA RO1 DA13386, ONR N00014-02-1-0879, and NIMH P01 MH42251. We thank Dr Ilan Kerman for helpful comments on the manuscript, and Richard Griggs for his excellent technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cecchi, M., Capriles, N., Watson, S. et al. β1 Adrenergic Receptors in the Bed Nucleus of Stria Terminalis Mediate Differential Responses to Opiate Withdrawal. Neuropsychopharmacol 32, 589–599 (2007). https://doi.org/10.1038/sj.npp.1301140
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1301140
Keywords
This article is cited by
-
Auricular neural stimulation as a new non-invasive treatment for opioid detoxification
Bioelectronic Medicine (2020)
-
Stress Modulation of Opposing Circuits in the Bed Nucleus of the Stria Terminalis
Neuropsychopharmacology (2016)
-
Alterations of naltrexone-induced conditioned place avoidance by pre-exposure to high fructose corn syrup or heroin in Sprague–Dawley rats
Psychopharmacology (2016)
-
Beta-2 adrenergic receptors mediate stress-evoked reinstatement of cocaine-induced conditioned place preference and increases in CRF mRNA in the bed nucleus of the stria terminalis in mice
Psychopharmacology (2014)
-
Extinction of conditioned opiate withdrawal in rats in a two-chambered place conditioning apparatus
Nature Protocols (2012)