Abstract
A clinical follow-up study was performed of adolescent major depressives and normal control subjects approximately 10 years after the subjects had undergone serial cortisol measurements over a 24-h period. In light of their young adulthood clinical status, our objective was to ascertain whether there were any premorbid cortisol abnormalities associated with depressive course of illness. In all, 77 young adults who had received a diagnosis of adolescent major depressive disorder, or were determined to be normal volunteers free of psychiatric diagnosis at index period and during follow-up, were studied. When subjects were adolescents, blood samples were collected for cortisol at 20-min intervals during the 24-h period coinciding with the third consecutive night of sleep EEG. The subjects, in young adulthood at the time of follow-up, were reinterviewed regarding longitudinal course of illness, and the original adolescent cortisol data were analyzed in the light of information obtained. Of the subjects who had experienced at least one lifetime major depressive episode during the follow-up period, the subgroup who would go on to make suicide attempts during the follow-up period secreted significantly greater levels of cortisol in the 4, 6, and 12 h prior to sleep onset. Conversely, this same subgroup exhibited reduced cortisol levels 2–4 h following sleep onset. Adolescents who are at risk to make suicide attempts appear to display significant elevations of cortisol prior to sleep onset, a time when the hypothalamic–pituitary–adrenal (HPA) axis is normally most quiescent. Dysregulation of the HPA axis, combined with dysfunction of sleep-onset mechanisms previously reported in this same cohort, might serve as premorbid biological substrates that predict suicide attempts during follow-up.
Similar content being viewed by others
INTRODUCTION
The role of central corticotropin releasing factor (CRF) hypersecretion and hypercortisolism in mood disorders continues to be an area of intense neuroscientific (Nemeroff, 1998) and neurodevelopmental focus (Caldji et al, 2000; Coplan et al, 1996; Goodyer et al, 2001b). Several recent developments, aided by a major improvement in an array of technological methodologies, have served to emphasize the key role that glucocorticoid overdrive may play in the pathophysiology of adult major depressive disorder (MDD) (Posener et al, 2000). The recognition that elevations of cortisol may have an inhibitory effect on neuroprotective brain trophic factors (Duman et al, 2000) and neurogenesis in animals (Gould et al, 1999) has highlighted the potentially deleterious effects of chronic stress and its neuroendocrine correlates in humans. Moreover, antidepressants that enhance synaptic concentrations of serotonin and/or norepinephrine may share the common mechanism of downmodulating multiple elements of the hypothalamic–pituitary–adrenal (HPA) axis (Holsboer, 2001) as well as increasing production of neuroprotective factors such as brain-derived neurotrophic factor (BDNF) (Duman et al, 2000).
It is therefore noteworthy that largely unremarkable 24-h cortisol secretory patterns have been observed in comparisons of adolescent outpatients with depression to normal controls (Dahl et al, 1989; Kutcher et al, 1991). Consistent with the adolescent findings, no evidence of HPA axis activity was noted in prepubertal depressives by Puig-Antich et al (1989). In a separate follow-up sample of both in- and outpatient depressed adolescents, Dahl et al (1991) examined the 24-h cortisol secretory pattern by a symptomatic subgroup of adolescent depressives. The authors noted that inpatient and suicidal status was associated with an increase of cortisol secretion during the usual evening nadir period prior to sleep onset when compared to less severely ill adolescent depressives and nonpsychiatrically ill volunteers.
Since diagnostic group assignment of subjects in studies of adolescent depression is complicated by the evaluation conceivably preceding manifestation of overt disorder, longitudinal follow-up of subjects may shed light on what had previously been reported as unremarkable patterns of 24-h cortisol secretion. Rao et al (1996) examined the relation between longitudinal clinical course and cortisol secretion in adolescent unipolar MDD. Subjects were 28 adolescents with a mean age of 15 years systematically diagnosed with unipolar MDD and 35 group-matched normal controls who participated in index sleep EEG and neuroendocrine studies. Follow-up clinical assessments were conducted approximately 7 years later in 94% of the original cohort. Although initial group comparisons failed to show significant differences in biologic measures, analyses incorporating clinical follow-up revealed that depressed subjects with a recurrent unipolar course showed a trend towards elevated plasma cortisol near sleep onset, compared to MDD subjects who had no further episodes during the follow-up interval. In a follow-up study by Rao et al (1999) in the same aforementioned cohort, increased anxiety traits and elevated cortisol secretion, also near sleep onset, were both associated with substance abuse disorders in depressed teenagers.
A third pediatric study revealed elevations of salivary cortisol, again in the evening hours (08:00 h), in 82 8- to 16-year-old major depressives, in comparison to 65 control cases (Goodyer et al, 1996), while longitudinal follow-up of this cohort revealed that chronic depression was marked by cortisol hypersecretion in the evening (Goodyer et al, 2001a). In the adult literature, a number of HPA axis studies in depressed subjects have yielded conflicting results for a multitude of factors, including method of ascertainment, disorder heterogeneity, and the complex circadian and ultradian periodicity of cortisol (see Posener et al, 2000 for a review).
In this report, we examined HPA axis function in 77 of the 88 (93.1%) adolescents who were originally studied by Joaquim Puig-Antich in the late 1970s and early 1980s, and described by Dahl et al (1989), in the light of independent and blind clinical follow-up conducted when the cohort was in young adulthood (Weissman et al, 1999). It is important to note that this New York City study sample is entirely independent of the Dahl et al (1991) study of depressed adolescents conducted at the University of Pittsburgh and followed up by Rao et al (1996). In the light of their young adulthood clinical status, and prior reports suggesting increased sleep-related growth hormone (GH) secretion predicted future suicide attempts in this cohort (Coplan et al, 2000a), our objective was to ascertain whether there were any premorbid cortisol abnormalities in this sample associated with depressive course of illness and attempted suicide. Based on our (and other groups') findings documenting extensive and complex interactions between HPA axis and GH secretory patterns (Coplan et al, 2000b; Coplan et al, 1997 for a review), we hypothesized that the course of adolescent-onset depression marked by suicide attempts in this unique sample would also be associated with sleep-related cortisol dysregulation.
METHODS AND MATERIALS
Initial Assessment
All procedures in the original and follow-up study were approved by the Institutional Review Boards of Columbia University and the New York State Psychiatric Institute, in accordance with the Declaration of Helsinki. Adolescents were accepted for screening at the New York State Psychiatric Institute between 1978 and 1984 if they were reported to appear sad or self-reported sadness, or presented with suicidal ideation or behavior, school refusal, nervousness, fears, or rituals. Each adolescent was screened during a 2-week diagnostic evaluation including the Schedule for Affective Disorder and Schizophrenia for School Age Children (K-SADS) (Chambers et al, 1985), Psychosocial Schedule (PSS) (Lukens et al, 1983), pediatric examination including Tanner staging for pubertal status, and IQ testing. A repeat K-SADS was conducted 10–16 days later to evaluate the stability of the symptomatology and aid in diagnosis.
Adolescents were also administered the K-SADS-E (epidemiologic version; Orvaschel et al, 1982) to assess the presence and nature of any previous episodes of psychiatric disorders. Inter-rater reliability and test–retest reliability for symptoms as reported at the time of the original study were both high (Chambers et al, 1985). The assessments were performed independently, and both the child and parent were interviewed. Only when there was complete agreement on diagnosis, and the child met the inclusion criteria for one of the proband groups, was the child entered into the study. The diagnosis of major depression was made using the unmodified adult Research Diagnostic Criteria (RDC; Spitzer et al, 1978). The normal subject control group was recruited by advertisement and word of mouth, contact with schools and counselors, and meetings with parent and teacher organizations. Normal subjects were required to have no current or past history of any psychiatric disorder. Neither the children nor their parents were told the aims of the study to avoid biased sampling. The K-SADS-E was used to interview the healthy control children and at least one of their parents. Only children who met none of the DSM-III (American Psychiatric Association 1980) criteria for psychiatric diagnoses during their lifetime were accepted into the normal group. Adolescents were accepted into the study only if they had attained at least Tanner Stage III (Marshall and Tanner, 1968) of pubertal development, and were determined to be medically healthy by a pediatrician. Informed consent was obtained from a parent or guardian and assent from all adolescents. The normal subjects were paid for their participation in the study.
The following ‘exclusion criteria’ were implemented: (1) medications (a 2-week washout was used); (2) significant medical illness; (3) pregnancy; (4) meeting DSM-III diagnostic criteria for anorexia nervosa, autism, schizophrenia, organic mental disorder, or substance abuse or dependence; (5) IQ <70.
Procedures Performed during Adolescence
The adolescents were admitted to the Sleep-Neuroendocrine Laboratory for three consecutive nights. Electrode placement for the standard sleep EEG recording was performed 1 h prior to the subject's usual bedtime. An intravenous catheter was placed in the morning after the second night of sleep. Blood samples were serially collected every 20 min for the next 24 h (inclusive of the third consecutive night of sleep). Blood samples were drawn through a three-way closed stopcock system. The samples were centrifuged; plasma was separated and then frozen at −20°C until the assay was performed. Plasma cortisol was analyzed by a competitive protein-binding modification of the method described by Murphy (1967).
Follow-Up Study performed during Young Adulthood
The original sample was relocated using old addresses of the subjects and their contacts, clinic records, files maintained by credit bureaus, public utilities, and newspaper advertisement (see Weissman et al (1999) for full details of methodology). If they consented, subjects and one informant were directly interviewed about the subjects' lifetime psychiatric history using the SADS-LA (Schedule for Affective Disorders and Schizophrenia-Lifetime Version (modified for the study of anxiety disorders)) (Mannuzza et al, 1986). The interviews were performed by clinicians extensively trained in the administration of this semistructured instrument. Interviewers were blind to the aims of the study and to the diagnostic group of the proband as well as the initial biological status. Diagnostic and course-of-illness information were also obtained from one informant (parent or another family member) per proband, in addition to the direct interview. Final follow-up psychiatric diagnoses were based on the best estimate procedure (Leckman et al, 1982).
Subjects were included in these reanalyses if they participated in the sleep EEG and 24 h neuroendocrine study as an adolescent, and subsequently completed a direct interview as an adult or had an informant complete an interview about them by SADS-LA prior to March 1997 (66% of the subjects had direct interviews, 34% had informant-only interviews). Of the original 88 subjects, 11 were not included either because they had not been located for follow-up or refused participation in the clinical follow-up (Weissman et al, 1999).
Characterization of Subject Groups
In order to further understand the relation between the adolescent cortisol data and course of illness, with a specific focus on suicide attempt history, four diagnostic outcome groups were characterized, identical to those utilized in prior biological investigations in this cohort (Coplan et al, 2000a; Goetz et al, 2001). See Table 1 for a summary of subject grouping.
In the original study (Dahl et al, 1989), 48 adolescents with MDD and 40 subjects without any psychiatric disorder (normal controls) participated. Of the original 88 adolescents, 77 (42 with original MDD and 35 original normal controls) were followed up clinically as adults about 10 years later, the subject of this paper. Lifetime-depressive subjects (n=56), who included both subjects diagnosed with MDD at baseline and members of the original control group who were found to have developed MDD at follow-up, were divided into three groups based on suicide-attempt status. Suicide attempt here refers to an actual attempt or definite plan, not simply suicidal ideation, gesture, or other parasuicidal behavior.
At 10-year follow-up as adults, 20 subjects had made suicide attempts prior to the original neuroendocrine studies (MDD T1 Suicide), and a subgroup of these also made attempts during the follow-up period, with seven completed suicides reported (Rao et al, 1993). Psychological autopsy revealed that five of the seven had recurrent depressive symptoms and were clinically depressed at the time of death (Rao et al, 1993). In all, 13 subjects would go on to make their initial suicide attempt during the follow-up period (MDD T10 Suicide) (this group was inclusive of 10 MDD subjects at time 1, and three time 1 controls that would become depressed and suicidal during the follow-up period). A total of 23 subjects would or had exhibited major depression but never had a suicide attempt (MDD no Suicide). Finally, 21 of the original normal control adolescent subjects remained depression-free (DFN) upon re-evaluation as adults. Of these subgroups, the MDD TI Suicide group had a significantly greater proportion of subjects (13 of 20) with a comorbid anxiety disorder (separation anxiety, phobias, GAD) at original assessment, vs the two other depressed groups (one subject in MDD no Suicide, and two subjects in MDD T10 Suicide) (χ2=30.42, df=3, p=0.001).
A subgroup of the adolescents (52 of 77) was assessed for first-degree family history of depression (Wickramaratne et al, 2000). Family history was assessed by direct interview with the SADS-LA or by family history with the Family History Screen (FHS; Weissman et al, 2000). The FHS is a brief screen that collects information on 15 psychiatric disorders and suicidal behavior in informants and their first-degree relatives; thus, cortisol measures were also analyzed for possible differences between subjects who did and did not have a positive family history of depression. The numbers available for this study who were in the family history study (Wickramaratne et al, 2000), and have cortisol data from time 1, were 30 for depressed and 22 for depression-free control subjects. In all, 80% of the depressed subjects and 68% of the depression-free controls had a first-degree relative with depression in the present study.
Statistical Analyses
The first step of the analysis was to align all serial cortisol samples to sleep onset. Sleep onset was defined by the first occurrence (30-s epoch) of stage 2 sleep, which was followed by 10 min of continuous sleep composed of stages 1, 2, 3, 4 or REM sleep. Repeated-measures analyses of covariance (ANCOVA-RMs) were used to compare the serial cortisol samples for the various subject groupings based upon the original adolescent and the adult clinical follow-up data. Greenhouse-Geisser adjusted degrees of freedom and probability levels were applied to all analyses. Age and gender served as covariates during all analyses. Gender could not be assessed as a separate factor because various group cells were too small. The ANCOVA-RMs were performed on specific secretory regions of interest (ROI), including the full 24-h period and 100 min before and after sleep onset, according to the convention of previous sleep neuroendocrine reports. After examination of the cortisol secretory patterns, we performed additional analyses of the 6 and 12 h prior to sleep onset (waking periods), and during the periods 4 h before and after sleep onset.
A number of discrete variables were calculated to characterize cortisol secretion. Simpson's approximation was used to calculate area under the cortisol curve for the 100 min prior to sleep onset (AUCPRE) and after sleep onset (AUCPOST). The maximum cortisol secretion overall and during wakefulness (24-h max and waking max), and the mean cortisol for the full 24-h period and during wakefulness (24-h mean and waking mean) were utilized. These were analyzed using multivariate ANCOVA, again including age and gender as covariates. When significant between-group differences were revealed, post hoc pairwise comparisons were performed to identify specific group differences. All data are expressed as mean±standard deviation (SD) unless otherwise specified, and a two-tailed α level of 0.05 is applied throughout.
Figure 1 presents the 24-h cortisol curves for the original MDDs and normal controls followed up approximately 10 years later. The two curves are nearly identical, verifying the original findings of Dahl et al (1989) in the subgroup that was available for follow-up. Notably the original report by Dahl et al, did not note significant gender differences among groups; in the current report, when gender was used as a covariate, the effect of gender was significant (F(1,71)=6.36, p=0.014), with females displaying higher cortisol overall. None of the statistically significant effects which follow can be attributed to the potential artifact created by the noninclusion of subjects which were included in the original analysis, as there were no differences in cortisol secretion between the subgroup followed longitudinally in comparison with that portion of the sample lost to follow-up. Likewise, none of the results are affected by anxiety disorder comorbidity, when used as a covariate.
RESULTS
Subjects with an original diagnosis of MDD were re-interviewed at a mean age of 25.19 (SD=2.42) years, and subjects originally assessed as normal controls were re-interviewed at a mean age of 25.92 (SD=2.16) years (t=1.4; p=0.16). Using the original diagnostic assignments, the mean duration of interval between neuroendocrine studies and clinical re-evaluation was 9.89 (SD=1.65) years in the depressed group and 9.55 (SD=1.35) years (t value=0.95; p=0.34) in the normal control group.
Differences between Subjects with Lifetime MDD Grouped by Suicide Attempt Status and Depression-Free Control Subjects
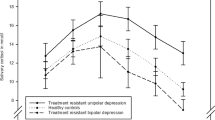
For the entire 24-h period of 72 samples, a significant group by time interaction is noted (F(36,827)=1.65, p=0.010; see Figure 2). During the period prior to sleep onset (samples 44 through sleep onset (sleep onset occurs between sample 1 and sample 2)), the MDD T10 Suicide group (the adolescent group who attempted suicide in the time between baseline assessment and follow-up) exhibited cortisol secretion levels that are elevated compared to the other three groups. This period approximates the late afternoon, early evening, and night time period prior to sleep onset. At the same time, this group's cortisol curve converges with the sleep onset cortisol nadir levels exhibited by all the groups (see Figure 2, samples 1–4). Upon sleep onset (between samples 1 and 2), low cortisol is typically associated with the first half of sleep and constitutes the diurnal nadir of cortisol secretion (Figure 2).
The 24-h cortisol secretion, including all subjects who were reassessed as young adults. Lifetime-depressive subjects were divided into three groups based on suicide-attempt status: suicide attempts at the time of the original biological studies (LT-MDDs TI Suicide), suicide attempts during the follow-up period (LT-MDDs T10 Suicide), and lifetime depressive subjects who did not make attempts (LT-MDDs w/o Suicide). The final group was the depression-free control subjects. For the entire 24-h period of 72 samples, a significant group by time interaction is noted (F(3,36)=1.65; p=0.010).
Previous investigations have defined 100 min before and after sleep onset as ROI (Rao et al, 1996; Dahl et al, 1989). However, inspection of the cortisol curves, mentioned above, revealed other ROI related to the MDD T10 Suicide group: specifically the region 6 h prior to sleep onset. Thus, we performed an analysis that included the 100 min pre- and post-sleep onset, and then a separate analysis of the 6 h period prior to sleep onset (approximate to early evening through bedtime). The analyses of the 100-min period pre- and post-sleep onset revealed a significant time by gender interaction (F (3.8,268)=3.45, p<0.010). There was also a trend interaction for time and group (F(11.5,268)=1.65, p=0.082). Age and gender were used as covariates. For the extended ROI, 6 h pre-sleep onset, an overall group effect was noted (F(3,70)=3.67; p=0.016), but no time effect (F(5,355)=1.60, p=0.157) and no group by time interaction (F(15,355)=0.89, p=0.579) was present (see Figure 3). Post hoc testing (pairwise) indicated that the MDD T10 Suicide group had significantly higher overall cortisol levels during these periods than the other three groups, including the MDD T1 Suicide group.
Given the suggestion of group differences in the time period prior to sleep onset, a ‘zoom in’ onto the 18 cortisol samples (6 h) prior to sleep was performed. Age and gender were used as covariates. An overall group effect was noted (F(3,70)=3.67; p=0.016), but no time effect (F=1.60, p=0.157) or group by time effect (F=0.89, p=0.579) were found. Post hoc testing (pairwise) indicated that the MDD T10 Suicide group (suicide attemptors during the follow-up period) had significantly higher overall cortisol levels than the other three groups including the MDD T1 Suicide group (those who made attempts at the time of original biological assessments). LT-MDDs w/o Suicide: subjects with lifetime histories of major depression without suicide; Dep-Free Controls: No history of depression.
Despite higher pre-sleep cortisol levels in the MDD T10 Suicide group, the MDD T10 Suicide group appeared to exhibit lower cortisol levels approximately 2–4 h after sleep onset. An analysis was performed where an additional factor representing 240 min (4 h) pre-sleep onset and post-sleep onset periods was analyzed. The first 4 h prior to sleep onset was designated pre-sleep and the first 4 h after sleep onset was designated as post-sleep onset. Age and gender were used as covariates. As above, gender could not be assessed as a separate factor because various group cells were too small. There was no overall group effect (F(3,70)=0.24, p=0.86); however, there was a significant interaction for group with pre-sleep/post-sleep factor (F(3,70)=4.00, p=0.011), and a significant interaction for gender with the pre-sleep/post-sleep factor (F(1,70)=4.70, p=0.034). These reflected the decline in cortisol levels as subjects went to sleep (Figure 4), the higher levels of cortisol in the MDD T10 Suicide group pre-sleep, and their lower levels of cortisol approximately 2–4 h after sleep onset. Among the discrete cortisol measures, the waking mean cortisol level significantly differed among the groups (F(3,72)=2.94, p=0.039), and this difference was attributable to the lower values for the MDD T10 Suicide group.
Illustration of the fact that despite higher pre-sleep cortisol levels in the MDD T10 Suicide group (suicide attemptors in the follow-up period), the MDD T10 Suicide group appeared to exhibit lower cortisol levels some 2–4 h after sleep onset (sample 13 on the graph). There was no overall group effect (F(3,70)=0.24, p=0.86), a significant pre-sleep/post-sleep effect (F(1,70)=4.27, p<0.042), and a significant interaction for the group with pre-sleep/post-sleep factor (F(3,70)=4.00, p=0.011). These reflected the decline in cortisol levels as subjects went to sleep, the higher levels of cortisol in the MDD T10 Suicide group pre-sleep, and their lower levels of cortisol approximately 2–4 h after sleep onset.
When subjects were divided into nonrecurrent depressives and recurrent depressives and compared with the depression-free controls, there was no effect over the 24-h period of sampling for recurrence group (F(2,70)=0.64, p=0.53) or recurrence group by time (F(22,775)=0.84, p>0.69), nor were any effects apparent in the other specific ROI. Latent depressives (those normal adolescents who experienced depressive episodes during the follow-up period) were not distinguishable from major depressive subjects or depression-free controls using the 20-min cortisol sampling method. When comparing the depression-free normals vs subjects with lifetime depression, no group effects or group-by-sample effects were noted for the 24-h sampling period or for the other ROI.
For the cortisol discrete variables, there was a trend noted for the cortisol waking maximum and 24-h mean secretion to be higher among subjects with lifetime depression (F(1,74)=3.64, p=0.060, and F(1,74)=3.40, p=0.069) vs depression-free normals.
As noted earlier, a subgroup of adolescents took part in family history assessments (Wickramaratne et al, 2000). Including family history as a factor revealed no significant cortisol curve differences; however, an analysis of the discrete measures indicated a strong trend for the family history-positive adolescents to exhibit a lower 24-h cortisol mean level (F=3.57, p=0.066). The small number of subjects with family history data available for analysis precluded more definitive analyses.
DISCUSSION
There were no significant differences between depressed and normal control adolescents on measures of HPA axis function in the original cohort (Dahl et al, 1989). However, the reanalysis of adolescent 24-h cortisol values in the light of longitudinal follow-up as adults yielded several significant findings which had not been evident as adolescents. Most significantly, adolescents with a depressive history who made future suicide attempts displayed evidence of HPA axis activation in the late evening hours, a time when the HPA axis is generally quiescent. It is of note that Rao et al (1996), in a smaller longitudinal study design, found that trend elevations of cortisol during a similar evening diurnal period were associated with a higher risk for a relapsing course of illness. Taken together, these studies suggest that cortisol elevations in this pre-sleep time period in adolescents might confer vulnerability for disorder recurrence and suicide attempts, although further longitudinal studies with larger samples are needed.
Other longitudinal follow-up studies in this same cohort have identified biological predictors of suicide attempts, prompting our investigation of potential HPA axis abnormalities as a function of suicidality. Of the subjects who had experienced at least one lifetime major depressive episode during the follow-up, the subgroup who would go on to make suicide attempts secreted significantly greater amounts of GH during the first 4 h of sleep (Coplan et al, 2000a). In addition, slow-wave sleep, REM latency, and the interaction between REM latency and slow wave sleep significantly or marginally predicted lifetime suicide attempts (Goetz et al, 2001). Future analyses that integrate these measures with the 24-h cortisol sleep studies are warranted, given that all three biological systems (GH, sleep, HPA axis) appear to be abnormally regulated in children and adolescents at risk for mood disorders (Birmaher et al, 2000; Rao et al, 2002; Goodyer et al, 2000).
Previous longitudinal studies in adolescent depression have failed to reveal HPA axis predictors of suicidality, although several studies in adult depression suggest that baseline HPA axis overactivity might be associated with either a history of past or future suicide attempts. Future suicide attempts in adults were predicted by elevated 24-h urinary 6-hydroxycorticosterone concentrations, while suicidal acts were associated with elevated plasma cortisol and dexamethasone suppression test (DST) resistance (see van Heeringen et al, 2000). Engstrom et al (1997) noted, using a personality cluster analysis, that nonsuppression on the DST bestowed an increased risk for future suicide attempt independent of personality cluster type. Further, a recent report (Coryell and Schlesser, 2001) of a 15-year longitudinal follow-up of depressed adult inpatients revealed that baseline HPA axis hyperactivity, as manifested by an abnormal DST, increased the odds of an eventual suicide 14-fold. However, another study revealed that increased plasma cortisol levels and DST resistance were significant predictors for severity of depression, but not for past suicidal acts (Brown et al, 1986). In terms of etiological determinants of adult suicidal behavior in mood disorders, there is an association between suicide attempts and a history of child abuse; notably, child abuse can result in HPA axis overreactivity to future stressors (see Heim and Nemeroff 2001). Retrospective investigations of early traumatic experiences among the MDD T10 suicide group, in comparison to the other depressed subgroups and controls, might be fruitful, although methodologically problematic.
There are several limitations that limit the generalizability of these findings. First, the high rate of the original normal controls who became depressed at 10-year follow-up is notable, as well as the original control group's high rate of family history of mood disorders. This fact illustrates that previous negative findings in biological studies of children and adolescents with MDD vs controls may be a consequence of studying traits in individuals who have not passed through the period of high risk for depression. In order to retain a larger cohort of ‘true’ controls in follow-up analyses, future biological investigations in adolescent and childhood depression should utilize ‘low-risk’ normal control groups, as has been performed in recent Pittsburgh studies (Birmaher et al, 2000). Second, our sample size, while representing the largest adolescent depressed sample followed up into adulthood, is still small for detailed analysis of subgroups. Third, approximately one-third of the follow-up subjects' diagnosis was made by indirect methods, and since follow-up covered a long time span, there was potential for retrospective recall bias in both that group and in the directly interviewed subjects, although the use of best estimate procedures served to minimize this bias.
In conclusion, the current study indicates that information on the clinical course of depression and suicidality of adolescents as they enter into young adulthood leads to the emergence of previously undetectable HPA axis abnormalities, most importantly in those subjects who are at risk for future suicide attempts. The debate of the factors which contribute to 24 h cortisol secretory patterns is clearly complex, with severity of illness, duration of illness, presence of psychosis, psychomotor agitation, age, suicidality, and outpatient status bearing relevance on these issues (Brown et al, 1986).
References
Birmaher B, Dahl RE, Williamson DE, Perel JM, Brent DA, Axelson DA et al (2000). Growth hormone secretion in children and adolescents at high risk for major depressive disorder. Arch Gen Psychiatry 57: 867–872.
Brown RP, Mason B, Stoll P, Brizer D, Kocsis J, Stokes PE et al (1986). Adrenocortical function and suicidal behavior in depressive disorders. Psychiatry Res 17: 317–323.
Caldji C, Diorio J, Meaney MJ (2000). Variations in maternal care in infancy regulate the development of stress reactivity. Biol Psychiatry 48: 1164–1174.
Chambers WJ, Puig-Antich J, Ryan N, Rabinovich H, Ambrosini P, Nelson B et al (1985). The assessment of affective disorders in children and adolescents by semi-structured interviews. Arch Gen Psychiatry 42: 696–702.
Coplan JD, Andrews MW, Rosenblum LA, Owens MJ, Friedman S, Gorman JM et al (1996). Persistent elevations of cerebrospinal fluid concentrations of corticotropin-releasing factor in adult nonhuman primates exposed to early-life stressors: implications for the pathophysiology of mood and anxiety disorders. Proc Natl Acad Sci USA 93: 1619–1623.
Coplan JD, Pine DS, Papp LA, Gorman JM (1997). A view on noradrenergic, hypothalamic–pituitary–adrenal axis and extrahypothalamic corticotrophin-releasing factor function in anxiety and affective disorders: the reduced growth hormone response to clonidine. Psychopharmacol Bull 33: 193–204.
Coplan JD, Smith EL, Trost RC, Scharf BA, Altemus M, Bjornson L et al (2000b). Growth hormone response to clonidine in adversely reared young adult primates: relationship to serial cerebrospinal fluid corticotropin-releasing factor concentrations. Psychiatry Res 95: 93–102.
Coplan JD, Wolk SI, Goetz RR, Ryan ND, Dahl RE, Mann JJ et al (2000a). Nocturnal growth hormone secretion studies in adolescents with or without major depression re-examined: integration of adult clinical follow-up data. Biol Psychiatry 47: 594–604.
Coryell W, Schlesser M (2001). The dexamethasone suppression test and suicide prediction. Am J Psychiatry 158: 748–753.
Dahl R, Puig-Antich J, Ryan N (1989). Cortisol secretion in adolescents with major depressive disorder. Acta Psychiatr Scand 80: 18–26.
Dahl RE, Ryan ND, Puig-Antich J, Nguyen NA, al-Shabbout M, Meyer VA et al (1991). 24-hour cortisol measures in adolescents with major depression: a controlled study. Biol Psychiatry 30: 25–36.
Duman RS, Malberg J, Nakagawa S, D'Sa C (2000). Neuronal plasticity and survival in mood disorders. Biol Psychiatry 48: 732–739.
Engstrom G, Alling C, Gustavsson P, Oreland L, Traskman-Bendz L (1997). Clinical characteristics and biological parameters in temperamental clusters of suicide attempters. J Affect Disord 44: 45–55.
Goetz RR, Wolk SI, Coplan JD, Ryan ND, Weissman MM (2001). Premorbid polysomnographic signs in depressed adolescents: a reanalysis of EEG sleep after longitudinal follow-up in adulthood. Biol Psychiatry 49: 930–942.
Goodyer IM, Herbert J, Altham PM, Pearson J, Secher SM, Shiers HM (1996). Adrenal secretion during major depression in 8- to 16-year-olds, I. Altered diurnal rhythms in salivary cortisol and dehydroepiandrosterone (DHEA) at presentation. Psychol Med 26: 245–256.
Goodyer IM, Herbert J, Tamplin A, Altham PM (2000). First-episode major depression in adolescents: affective, cognitive and endocrine characteristics of risk status and predictors of onset. Br J Psychiatry 176: 142–149.
Goodyer IM, Park RJ, Herbert J (2001a). Psychosocial and endocrine features of chronic first-episode major depression in 8–16 year olds. Biol Psychiatry 50: 351–357.
Goodyer IM, Park RJ, Netherton CM, Herbert J (2001b). Possible role of cortisol and dehydroepiandrosterone in human development and psychopathology. Br J Psychiatry 179: 243–249.
Gould E, Reeves AJ, Graziano MS, Gross CG (1999). Neurogenesis in the neocortex of adult primates. Science 286: 548–552.
Heim C, Nemeroff CB (2001). The role of childhood trauma in the neurobiology of mood and anxiety disorders: preclinical and clinical studies. Biol Psychiatry 49: 1023–1039.
Holsboer F (2001). Stress, hypercortisolism and corticosteroid receptors in depression: implications for therapy. J Affect Disord 62: 77–91.
Kutcher S, Malkin D, Siverberg J, Marton P, Williamson P, Malkin A et al (1991). Nocturnal cortisol and thyroid stimulating hormone and growth secretory profiles in depressed adolescents. J Am Acad Child Adolesc Psychiatry 30: 407–414.
Leckman JF, Sholomskas D, Thompson WD, Belanger A, Weissman MM (1982). Best estimate of lifetime psychiatric diagnosis: a methodological study. Arch Gen Psychiatry 39: 879–883.
Lukens E, Puig-Antich J, Behn J, Goetz R, Tabrizi M, Davies M (1983). Reliability of the psychosocial schedule for school age children. J Am Acad Child Psychiatry 22: 29–39.
Mannuzza S, Fyer AJ, Klein DF, Endicott J (1986). Schedule for affective disorders and schizophrenia: lifetime version; modified for the Study of Anxiety Disorders (SADS-LA). J Psychiatr Res 20: 317–325.
Marshall WA, Tanner JM (1968). Growth and physiological development during adolescence. Annu Rev Med 29: 283–300.
Murphy BEP (1967). Some studies of the protein binding of steroids and their application to the micro and ultramicro measurement of various binding radio assay. J Clin Neuroendocrinol Metab 27: 973.
Nemeroff CB (1998). The neurobiology of depression. Sci Am 278: 42–49.
Orvaschel H, Puig-Antich J, Chambers W, Tabrizi MA, Johnson R (1982). Retrospective assessment of prepubertal major depression with the Kiddie-SADS-e. J Am Acad Child Psychiatry 21: 392–397.
Posener JA, De Battista C, Williams GH, Kraemer HC, Kalehzan BM, Schatzberg AF (2000). 24-hour monitoring of cortisol and corticotropin secretion in psychotic and nonpsychotic major depression. Arch Gen Psychiatry 57: 755–760.
Puig-Antich J, Dahl R, Ryan N (1989). Cortisol secretion in prepubertal children with major depressive disorders. Arch Gen Psychiatry 46: 801–809.
Rao U, Dahl RE, Ryan ND, Birmaher B, Williamson DE, Giles DE et al (1996). The relationship between longitudinal clinical course and sleep and cortisol changes in adolescent depression. Biol Psychiatry 40: 474–484.
Rao U, Dahl RE, Ryan ND, Birmaher B, Williamson DE, Rao R, Kaufman J (2002). Heterogeneity in EEG sleep findings in adolescent depression: unipolar versus bipolar clinical course. J Affect Disord 70: 273–280.
Rao U, Ryan ND, Dahl RE, Birmaher B, Rao R, Williamson DE et al (1999). Factors associated with the development of substance use disorder in depressed adolescents. J Am Acad Child Adolesc Psychiatry 38: 1109–1117.
Rao U, Weissman MM, Martin JA, Hammond RW (1993). Childhood depression and risk of suicide: a preliminary report of a longitudinal study. J Am Acad Child Adolesc Psychiatry 32: 21–27.
Spitzer RL, Endicott J, Robins E (1978). Research diagnostic criteria: rationale and reliability. Arch Gen Psychiatry 35: 773–782.
Van Heeringen K, Audenaert K, Van de Wiele L, Verstraete A (2000). Cortisol in violent suicidal behaviour: association with personality and monoaminergic activity. J Affect Disord 60: 181–189.
Weissman MM, Adams P, Wolk SI, Verdeli L, Wickramaratne PJ, Olfson M (2000). Brief screening for family psychiatric history: the Family History Screen (FHS). Arch Gen Psychiatry 57: 675–682.
Weissman MM, Wolk S, Goldstein RB, Moreau D, Adams P, Greenwald S et al (1999). Depressed adolescents grown up. JAMA 281: 1707–1713.
Wickramaratne PJ, Greenwald S, Weissman MM (2000). Psychiatric disorders in the relatives of probands with prepubertal-onset or adolescent-onset major depression. J Am Acad Child Adolesc Psychiatry 39: 1396–1405.
Acknowledgements
This work was supported by grants from NIMH R01(MH 50666) and RO1 36197 (to Dr Weissman), Scientist Development Awards for Clinicians MH-01039 (to Dr Coplan), and American Foundation for Suicide Prevention (Dr Mathew).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mathew, S., Coplan, J., Goetz, R. et al. Differentiating Depressed Adolescent 24 h Cortisol Secretion in Light of Their Adult Clinical Outcome. Neuropsychopharmacol 28, 1336–1343 (2003). https://doi.org/10.1038/sj.npp.1300184
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1300184
Keywords
This article is cited by
-
Insomnische Symptome und Suizidalität – Zusammenhänge und Management
neuropsychiatrie (2023)
-
A Comprehensive Review of the Literature on Sleep Difficulties and Suicidality in Youth to Inform an Integrative Developmental Model and Future Directions
Current Sleep Medicine Reports (2022)
-
The underlying neurobiology of key functional domains in young people with mood and anxiety disorders: a systematic review
BMC Psychiatry (2016)
-
Multi-Level Risk Factors for Suicidal Ideation Among at-Risk Adolescent Females: The Role of Hypothalamic-Pituitary-Adrenal Axis Responses to Stress
Journal of Abnormal Child Psychology (2015)
-
Die Bedeutung von Schlafstörungen für die Prävention von Suizidalität
Somnologie - Schlafforschung und Schlafmedizin (2015)