Abstract
The aim of the study is to test whether fluvoxamine affects the function of the hypothalamic pituitary adrenal (HPA) axis in female borderline (borderline personality disorder, BPD) patients with and without a history of sustained childhood abuse. Special attention is given to the presence of comorbid major depressive disorder (MDD) and post-traumatic stress disorder (PTSD). The HPA axis of 30 female BPD patients with (n=17) and without (n=13) a history of sustained childhood abuse was challenged with a combined dexamethasone and corticotropin releasing hormone test (DEX/CRH test) before and after 6 (n=14) and 12 (n=16) weeks of fluvoxamine treatment (150 mg/day). Both 6- and 12-week fluvoxamine treatments were associated with a significant and robust reduction of the adrenocorticotrophic hormone (ACTH) and cortisol response to the DEX/CRH test. The magnitude of the reduction was dependent on the presence of sustained childhood abuse, but not on the presence of comorbid MDD or PTSD: patients with a history of sustained childhood abuse showed the strongest reduction in ACTH and cortisol. In conclusion, Fluvoxamine treatment reduces the hyperresponsiveness of the HPA axis in BPD patients with a history of sustained childhood abuse. This effect is likely to be obtained in the first 6 weeks of treatment.
Similar content being viewed by others
INTRODUCTION
A large number of patients with borderline personality disorder (BPD) report a history of severe and sustained childhood abuse, and many of them meet the criteria for comorbid major depressive disorder (MDD) and/or post-traumatic stress disorder (PTSD) (Zanarini et al, 1998). These related conditions are all associated with alterations of the hypothalamic pituitary adrenal (HPA) axis.
Sustained childhood abuse is associated with a permanently increased responsiveness of the HPA axis (Rinne et al, 2002). This is reflected in a much higher adrenocorticotrophic hormone (ACTH) and cortisol response to a combined dexamethasone/corticotropin releasing hormone (DEX/CRH) test in BPD patient with a history of sustained childhood abuse compared to BPD patients with no or incidental abuse and healthy controls (Rinne et al, 2002). In line with this finding, two other studies found a hyperarousal in response to a psychological stressor and CRH challenge in women with a history of childhood abuse. (Heim et al, 2000a, 2000b). Clinical and preclinical studies suggest that an enhanced expression of CRH and its potent coregulator arginine vasopressin (AVP) in the hypothalamic nucleus paraventricularis (PVN) is involved in the pathogenesis of this hyper-responsiveness of the HPA axis (Coplan et al, 1996; Hatalski et al, 1998; von Bardeleben et al, 1985). This hyper-responsiveness of the HPA axis may render the abused BPD patients very susceptible to stress, and in case of sustained stress to depression comparable with subjects with a heritable predisposition for MDD (Holsboer et al, 1995).
A total of 50% of the patients suffering from MDD demonstrate to have hypercortisolism, and a decreased negative feedback inhibition marked by a decreased efficacy of DEX to suppress circulating cortisol (Carroll et al, 1981a; Carroll, 1982; Evans and Nemeroff, 1985). In contrast, PTSD is associated with hypocortisolism, increased negative feedback inhibition and hypersuppression of circulating cortisol after DEX (Yehuda et al, 1990; Yehuda et al, 1993; Yehuda, 1998). During the 1980s, a series of dexamethasone suppression test (DST) studies have been conducted in BPD patients. Most of these studies were not conclusive, because the potential effects of MDD and/or PTSD on the outcome were not taken into account (for an overview see Lahmeyer) (Baxter et al, 1984; Carroll et al, 1981b; Kontaxakis et al, 1987; Krishnan et al, 1984; Lahmeyer et al, 1989; Soloff et al, 1982; Steiner et al, 1984; Sternbach et al, 1983).
Studies on the treatment of psychiatric disorders related to a hyperactive HPA axis show that recovery from MDD in patients treated with an antidepressant (eg selective serotonergic reuptake inhibitors: SSRIs) is paralleled by the attenuation of the hyperactive HPA axis (Barden et al, 1995; De Bellis et al, 1993; Holsboer and Barden, 1996). Moreover, animal studies have shown that antidepressants may restore HPA-axis feedback deficiency (Rowe et al, 1997).
In the present study, we hypothesize that the treatment with an antidepressant drug (eg the SSRI fluvoxamine) will reduce the responsiveness of the HPA axis in BPD patients. A history of sustained childhood abuse, concurrent MDD and/or PTSD is expected to modify substantially the outcome of the DEX/CRH test after fluvoxamine treatment. Therefore, these factors were taken into consideration in an analysis of covariance.
To investigate the hypotheses and to explore the time frame of the functional reduction of the HPA-axis activity, a combined DEX/CRH challenge test is performed before and after 6 or 12 weeks of fluvoxamine treatment in a group of patients with BPD, including both patients with and without sustained childhood abuse. This report is part of a larger study, and some data were described in an earlier paper (Rinne et al, 2002).
METHODS
Subjects
A total of 30 healthy female borderline patients with and without sustained childhood abuse were included in the study (for sample characteristic, see Table 1). Subjects were recruited from outpatient mental health-care centers and by advertising. In order to be included in the fluvoxamine trial, all of the patients had to obtain a score of 110 or more on the borderline trait and distress scale of a self-report screener ‘Assessment of DSM-IV Personality Disorder’ (ADP-IV) (Schotte et al, 1998), meet more than 5 of the BPD criteria on the ‘Structured Interview for DSM-IV Personality Disorders’ (SIDP-IV) (De Jong et al, 1996; Pfohl et al, 1995), and receive a score of 20 or more on the fully structured ‘Borderline Personality Disorder Severity Index’ (BPDSI) (Arntz et al, 2002; Weaver and Clum, 1993).
All eligible subjects were screened for somatic conditions and examined physically; an electrocardiogram, a complete blood count, routine blood chemistry analyses, and urine analyses were performed to exclude somatic illness.
Exclusion criteria were schizophrenia, a lifetime episode of mania, current major depression that did last more than 4 weeks and current drug or alcohol abuse or dependence according to a fully structured psychiatric interview: ‘Composite International Diagnostic Interview’ (CIDI) (ter Smitten et al, 1997; WHO, 1997).
Diagnoses of concurrent MDD and PTSD were also obtained by the CIDI. Specially trained psychologists who were blind for the diagnoses performed diagnostic interviews. Subgroups were defined according to the presence of sustained childhood abuse assessed with the ‘Structured Trauma Interview’ (STI)(Draijer, 1989). In this interview, patterns of both physical and sexual abuse are explored. The frequencies of abuse are scored along a 7-point scale (0=none, 1=only once, 2=once or twice a year, 3=once or twice in 6 months, 4=once or twice a month, 5=once or twice a week, 6=daily). The severity of the subjective perception of the abuse is measured along a 5-point scale ranging from 0 (=not distressing) to 4 (=very seriously distressing). The criteria for the assignment of the borderline patients to the group of ‘no or incidental childhood abuse’ or the group of ‘sustained childhood abuse’ were based on an abuse frequency score of 3 and higher, and onset of the abuse at an age younger than 16 years.
In previous studies, frequency of abuse, as assessed with the STI, was found to be a reliable predictor of the neuro-endocrine sequelae of childhood abuse (Rinne et al, 2000). In addition, frequency of abuse highly correlated with other abuse parameters such as duration in years (r=0.792, p<0.000) and age of onset (r=−0.810, p<0.000) (Rinne et al, 2002).
All subjects had to be medication-free at least 14 days prior to the neuro-endocrine challenge test (fluoxetine 6 weeks). They were also not allowed to drink alcohol 1 week prior to the test. All of the patients provided their fully informed written consent. The ethical committee of our clinic approved the study.
Design
After diagnostic baseline assessment, the first combined DEX/CRH test was performed just before the start of fluvoxamine treatment (150 mg/day). The second DEX/CRH test was performed for one group (n=14) after 6 weeks of fluvoxamine treatment, and for the other group (n=16) after 12 weeks of fluvoxamine treatment.
Neuro-endocrine challenge procedure
For the combined DEX suppression CRH releasing hormone challenge test (DEX/CRH), the refined procedure developed at the Max Planck Institute in Munich was adopted. (Heuser et al, 1994). Participants had to ingest an oral dosage of 1.5 mg of DEX at 11 pm the evening before the challenge. In order to check for the ingestion of DEX, 50 mg of riboflavin was added to the capsule. Riboflavin has a rapid renal clearing, and the subjects were therefore asked to collect their first urine the morning of the test procedure. The same morning, the participants had a light breakfast and were instructed to not eat or drink after 11:00 am, with the exception of water or herbal tea. The participants arrived at the research unit at 1:30 pm. The riboflavin concentrations in their morning urine were analyzed before 3:00 pm. They were asked to rest supine on a bed; a cannula was inserted in the forearm vein and kept open by heparanization. At 3:00 pm (after baseline sampling), 100 g of CRH (Ferring BV, Hoofddorp, The Netherlands) reconstituted in 1 ml of 0.9% saline was administered in the cannula within 30 s. Blood samples for cortisol and ACTH plasma level measurement were taken at five time points: 3:00 pm (baseline level before CRH), 3:30, 3:45, 4:00, and 4:15 pm. Blood pressure, heart rate, and temperature were also measured at the same time points. Baseline afternoon cortisol and ACTH plasma levels without a challenge probe (DEX/CRH) were measured on a different day before the start of fluvoxamine treatment. These baseline measurements were taken at the same time points as the DEX/CRH challenge the test measurements. All of the blood samples were extracted by vacuum into three plain tubes (5 ml); the first tube was discarded. The tubes were immediately placed on ice; after centrifugation, the plasma was kept frozen at −70°C until analysis. Cortisol and ACTH plasma levels were analyzed with commercially available assays. The cortisol assay was obtained from Boehringer Mannheim and the ACTH assay from Nichols Institute Diagnostics. The intra- interassay coefficients of variation for cortisol measurement were less then 6 and 10%, respectively. The intra–interassay coefficients of variation for ACTH measurement were less then 3.2 and 6.3%, respectively.
Statistical Analysis
The efficacy of fluvoxamine to reduce the increased responsiveness of the HPA axis in BPD patients could be reflected in the lower cortisol and ACTH afternoon baseline levels, or in the decreased ACTH or cortisol responses to CRH after DEX pretreatment. The latter data were calculated using the area under the concentration time curve (AUC) of ACTH and cortisol response. The overall effect of fluvoxamine on the response of the HPA axis to the DEX/CRH challenge tests in BPD patients was analyzed using paired Student's t-tests to compare the ACTH and cortisol AUCs before and after treatment. To assess the influence of the factors sustained childhood abuse, comorbid PTSD, and MDD on the effect of fluvoxamine, a stepwise backward analysis of (co)variance was performed for each dependent variable, starting from a full repeated model with pre- and post-treatment measures of the dependent variable as the repeated within-subject factor and sustained childhood abuse, comorbid PTSD and MDD as between-subject factors. Interaction of a between-subject factor with the within-subject factor indicates a moderating effect of this between-subject factor on the effectiveness of fluvoxamine. In all the analysis corrections for age, body mass index, and contraceptive pill usage were made, if required.
RESULTS
ACTH and Cortisol Response Pre/Post-Fluvoxamine
No significant overall changes in mean afternoon baseline cortisol and ACTH baseline levels were detected after 6 or 12 weeks of fluvoxamine treatment. However, fluvoxamine treatment was associated with a significant and robust decrease of the mean AUC of the ACTH and cortisol response to DEX/CRH challenge: Mean AUC of the cortisol concentration time curve decreased from 85.3 (SD=110.7) to 16.65 (SD=44.42); (t=3.77, df=29, p=0.001), and mean AUC of the ACTH concentration time curve from 8.77 (SD=9.21) to 2.21 (SD=5.18); (t=3.70, df=29 p=0.001).
Covariates: Childhood Abuse, MDD, and PTSD
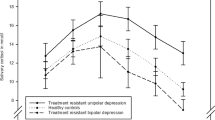
Regarding the question as to whether the reduction of the responsiveness of the HPA axis by fluvoxamine treatment is expressed more in BPD subjects with a history of sustained childhood abuse and whether this effect is affected by comorbid PTSD or MDD, stepwise backward analyses of covariance have been performed. This revealed no effects for changes in mean cortisol and ACTH afternoon baseline levels. However, changes in AUCs of the cortisol and ACTH response to the DEX/CRH test were significantly dependent on a history of sustained childhood abuse, but not on the various forms of psychiatric comorbidity. Mean AUC ACTH response for those subjects with sustained childhood abuse dropped from 12.70 (SD=10.41) to 2.37 (SD=5.82), while for those subjects with no or incidental childhood abuse the mean AUC ACTH response dropped from 3.63 (SD=3.19) to 2.00 (SD=4.43) (F(1.28)=7.19, p=0.012; see also Figure 1). Mean AUC cortisol response for those subjects with sustained childhood abuse dropped from 113, 2 (SD=121, 0) to 13, 9 (SD=30.7), while for those subjects with no or incidental childhood abuse the mean AUC cortisol response dropped from 48.9 (SD=87.0) to 20.2 (SD=59.1) (F(1.28)=4.08, p=0.058; see also Figure 2).
Concentration time curve of ACTH response to DEX/CRH challenge pre- and post-fluvoxamine (FLVX) treatment for abused (n=17) and not abused (n=13) BPD subjects. Student's t-test for independent samples of mean AUCs of ACTH of the abused vs not abused subjects pre-fluvoxamine treatment (a) t=3.390, df=28, p=0.005 and post-fluvoxamine (b) t=0.199, df=28, p=0.84. Student's paired t-test of mean AUC of ACTH pre- vs post-fluvoxamine treatment for the abused and not abused subjects (c) t=−3.80, df=16, p=0.002 and (d) t=1.61, df=12, p=0.134, respectively.
Concentration time curve of cortisol response to DEX/CRH challenge pre- and post-fluvoxamine (FLVX) treatment for abused (n=17) and not abused (n=13) BPD subjects. Student's t-test for independent samples of mean AUCs of cortisol of the abused vs not abused subjects pre-fluvoxamine treatment (a) t=1.69, df=27, 93, p=0.10 and post-fluvoxamine (b) t=0.352, df=16,93, p=0.73. Student's paired t-test of mean AUCs of cortisol pre- vs post-fluvoxamine treatment for the abused and not abused subjects (c) t=3.57, df=16, p=0.001 and (d) t=1.75, df=12, p=0.106, respectively.
Time Frame of the Fluvoxamine Effect on the HPA Axis
The AUC of ACTH response after DEX/CRH challenge decreased from 8.99 (SD=9.70) to 2.60 (SD=4.07) and from 8.57 (SD=9.08) to 1.87 (SD=6.10) after 6 weeks of fluvoxamine treatment (n=14) and after 12 weeks of fluvoxamine treatment (n=16), respectively. As a result of the equal decrease in both groups no statistically significant group by time effect could be found (F(1.28)=0.007, p=0.933), indicating that fluvoxamine is most likely to exert its effect in the first 6 weeks of treatment.
DISCUSSION
Fluvoxamine treatment was associated with a significant and robust reduction of the ACTH and cortisol response to the combined DEX/CRH challenge test in chronically abused BPD subjects. BPD subjects with no or incidental childhood abuse had low pre- and post-treatment ACTH and cortisol responses to DEX/CRH challenge. The presence of a comorbid diagnosis of MDD or PTSD did not influence the effect of fluvoxamine on ACTH and cortisol responses to the DEX/CRH test in these BPD subjects. The comparison of the 6 and 12 weeks treatment with fluvoxamine suggests that the decrease of the ACTH and cortisol response is already established in the first 6 weeks of the treatment. The robust decrease of the ACTH and cortisol response to the DEX/CRH test after fluvoxamine treatment in the chronically childhood abused BPD subjects may reflect a reduction of the enhanced CRH/AVP drive in these subjects (Rinne et al, 2002). In a previous study, we showed that the prolactine response following a challenge with the serotonergic agonist meta-chlorophenylpiperazine (m-CPP) in BPD subjects showed a strong inverse relation with sustained childhood abuse (Rinne et al, 2000). However, an 8-week treatment with fluvoxamine did not restore the severly blunted prolactine response (Rinne et al, 2002). The combination of these findings directs our attention to the HPA axis as primary target of SSRI treatment in the severely abused BPD subjects, and not to the central serotonergic system.
Preclinical research has provided some clues as to how these effects of childhood abuse and fluvoxamine on the HPA axis evolve (Levine et al, 2000). It appeared that early life stressors such as maternal deprivation persistently enhance the responsiveness of the HPA axis in adulthood (Ma and Lightman, 1998; Oitzl et al, 2000). The effect exerted by maternal deprivation resulted in the altered expression of the hippocampal mineralo (MR) and glucocorticoid receptor (GR) sites (Oitzl et al, 2000) in a manner that would explain the enhanced HPA responsiveness (De Kloet et al, 1998). In other studies, early stress was found to induce an increase in the number of hypothalamic CRH neurons and an increase in CRH and AVP m-RNA expression (Coplan et al, 1996, 2001; De Goeij et al, 1992; Hatalski et al, 1998; Lim, 2000; Plotsky and Meaney, 1993). An elevated AVP/CRH release is likely to enhance the expression of pro-opiomelanocortin (POMC) synthesis and the release of its peptide product ACTH in the pituitary corticotrophs. Preclinical studies on the effects of the chronic administration of different antidepressants demonstrate that a decrease of the HPA-axis activity is a final common pathway of antidepressant effects, but that the different antidepressants unfold their specific pharmaco-logical efficacy on varying HPA-axis levels and receptor subsystems. Tricyclic antidepressants as well as the SSRI fluoxetine are likely to increase either GR m-RNA or MR m-RNA expression in the hippocampus, depending on the type of drug (Barden et al, 1995; Brady et al, 1992; DeRijk et al, 2001; Holsboer and Barden, 1996; Jensen et al, 1999; Okugawa et al, 1999; Seckl and Fink, 1992). Owing to the increase of hippocampal MRs and GRs, they are thought to regain their balance re-establishing the inhibitory tone on the PVN in the hypothalamus. In accordance with this assumption, CRH m-RNA in the hypothalamic PVN and CSF CRH as well as AVP turn out to be decreased after fluoxetine treatment (Brady et al, 1992; De Bellis et al, 1993). In this context, another (hypothetical) pathway of SSRI's action on the HPA axis may be of interest (Brady, 1994). The CRH neurons of the PVN and the locus coruleus (LC) maintain a positive feedback loop in case of stress (Holsboer and Barden, 1996; Valentino et al, 1983). Sustained SSRI treatment leads to a reduced firing rate of noradrenergic neurons of the LC (Szabo et al, 1999, 2000), which is expected to have its repercussion on the hypothalamic CRH neurons and thus on the release of ACTH secretagogs.
In conclusion, the above-mentioned factors may contribute to a normalization of the hyper-responsive stress axis of the severely childhood abused BPD subjects, as reflected by a decreased ACTH, and cortisol response to the DEX/CRH test after fluvoxamine treatment. The failure to detect the expected neuro-endocrinological effects of concurrent MDD (Barden et al, 1995) in 11 BPD subjects on the ACTH and cortisol response to the DEX/CRH test after fluvoxamine treatment in our BPD sample, might be because of the considerable overlap of concurrent PTSD and MDD. Six of the 11 subjects who suffered from MDD also had comorbid PTSD. In a previous study—to which this study is linked up—we showed that the BPD subjects with concurrent MDD and PTSD exhibited a strongly increased negative feedback inhibition of the pituitary corticotrophs, as demonstrated by hypersuppression of circulating cortisol to DEX challenge, equally to subjects suffering only from PTSD (Rinne et al, 2002). In contrast, BPD subjects with only comorbid MDD showed decreased efficacy of cortisol suppression to DEX (Rinne et al, 2002). Therefore, the expected neuro-endocrine effects of MDD are most likely to be outnumbered by the overlap with comorbid PTSD. The childhood abuse subgroup was significantly older than the nonabuse subgroup, which was taken into account in the statistical analysis. The lower education level of the abused group may be a reflection of the adverse rearing conditions in which they grew up.
Some methodological limitations should be mentioned at this point. Since there was no placebo control group of BPD subjects with and without sustained childhood abuse, it cannot be ruled out that factors other than fluvoxamine treatment, such as natural course, account for the decreased ACTH and cortisol response to the DEX/CRH test. However, the observed effect is too large and too robust to presume that it is a result of only of natural course. Moreover, our finding is in line with the findings from other perclinical and clinical studies (vide supra). In addition, it should be noted that our conclusions regarding the time course of the functional reduction of the HPA axis are based on only two observations. It would have been better to have at least three different points in time during the fluvoxamine treatment with DEX/CRH test results. Therefore, our finding concerning the time course should be regarded as preliminary, and replication with a refined design is needed.
This study contributes to the knowledge of the effect of fluvoxamine in chronically childhood abused and not or incidentially abused borderline patients. Whereas childhood abuse seems to leave a chronic increase of the excitability of the HPA axis (Rinne et al, 2002), fluvoxamine turns out to reduce these effects as demonstrated by an attenuated ACTH and cortisol response after the combined DEX/CRH test. This normalization is likely to take place in the first 6 weeks of fluvoxamine treatment. Therefore, it can be concluded that SSRI treatment might be a supportive strategy in addition to cognitive training in stress management to reduce the susceptibility of the chronically abused BPD subjects to stress and stress-related disorders like MDD.
References
Arntz A, Hoorn van den M, Cornelis J, Verheul R, Bosch van den W, Bie de AJHT (2002). Reliability and validity of the Borderline Personality Disorder Severity Index. J. Personality, Disorders Accepted, pending revision.
Barden N, Reul JM, Holsboer F (1995). Do antidepressants stabilize mood through actions on the hypothalamic-pituitary-adrenocortical system? Trends Neurosci 18: 6–11.
Baxter L, Edell W, Gerner R, Fairbanks L, Gwirtsman H (1984). Dexamethasone suppression test and Axis I diagnoses of inpatients with DSM-III borderline personality disorder. J Clin Psychiatry 45: 150–153.
Brady LS (1994). Stress, antidepressant drugs, and the locus coeruleus. Brain Res Bull 35: 545–556.
Brady LS, Gold PW, Herkenham M, Lynn AB, Whitfield Jr HJ (1992). The antidepressants fluoxetine, idazoxan and phenelzine alter corticotropin-releasing hormone and tyrosine hydroxylase mRNA levels in rat brain: therapeutic implications. Brain Res 572: 117–125.
Carroll BJ (1982). Use of dexamethasone test in depression. J Clin Psychiatry 43: 44–50.
Carroll BJ, Feinberg M, Greden JF, Traika J, Albala AA, Haskett RF et al (1981a). A specific laboratory test for the diagnosis of melancholia; Standardization, validation, and clinical utility. Arch Gen Psychiatry 38: 15–22.
Carroll BJ, Greden JF, Feinberg M, Lohr N, James N, Steiner M et al (1981b). Neuroendocrine evaluation of depression in borderline patients. Psychiatr Clin North Am 4: 89–99.
Coplan JD, Andrews MW, Rosenblum LA, Owens MJ, Friedman S, Gorman JM et al (1996). Persistent elevations of cerebrospinal fluid concentrations of corticotropin-releasing factor in adult nonhuman primates exposed to early life stressors: implications for the pathophysiology of mood and anxiety disorders. Proc Natl Acad Sci USA 93: 1619–1623.
Coplan JD, Smith ELP, Altemus M, Scharf BA, Owens MJ, Nemeroff CB et al (2001). Variable foraging demand rearing: sustained elevations in cisternal cerebrospinal fluid corticotropin-releasing factor concentrations in adult primates. Biol Psychiatry 50: 200–204.
De Bellis MD, Gold PW, Geracioti Jr TD, Listwak SJ, Kling MA (1993). Association of fluoxetine treatment with reductions in CSF concentrations of corticotropin-releasing hormone and arginine vasopressin in patients with major depression. Am J Psychiatry 150: 656–657.
De Goeij DCE, Jezova D, Tilders FJH (1992). Repeated stress enhances vasopressin synthesis in corticotropin releasing factor neurons in the paraventricular nucleus. Brain Res 577: 165–168.
De Jong CAJ, Derks FCH, van Oel C, Rinne T (1996). Structured Interview for DSM-IV Personality Disorders (SIDP-VI); B Pfohl & N Blum & M Zimmermann—Authorized Dutch Translation. St.: Stichting Verslavingszorg Oost Brabant.
De Kloet ER, Vreugdenhil E, Oitzl MS, Joels M (1998). Brain corticosteroid receptor balance in health and disease. Endocr Rev 19: 269–301.
DeRijk RH, Meijer OC, De Kloet ER (2001). Brain corticosteroid receptors: targets for treatment of depression. In: Thakore JH (ed). Physical consequences of depression. 1st edn. Wrightson Biomedical Publishing Ltd, Petersfield, UK and Philadelphia, USA, pp 23–52.
Draijer N (1989). Structured Trauma Interview. Department of Psychiatry, Vrije Universiteit, Amsterdam.
Evans DL, Nemeroff CB (1985). Use of dexamethasone suppression test using DSM III criteria on an inpatient psychiatric unit. Biol Psychiatry 18: 505–511.
Hatalski CG, Guirguis C, Baram TZ (1998). Corticotropin releasing factor mRNA expression in the hypothalamic paraventricular nucleus and the central nucleus of the amygdala is modulated by repeated acute stress in the immature rat. J Neuroendocrinol 10: 663–669.
Heim C, Newport DJ, Heit S, Graham YP, Wilcox M, Bonsall R et al (2000a). Pituitary-adrenal and autonomic responses to stress in women after sexual and physical abuse in childhood. JAMA 284: 592–597.
Heim C, Newport DJ, Miller AH, Nemeroff CB (2000b). Long-term neuroendocrine effects of childhood maltreatment [In Process Citation]. JAMA 284: 2321.
Heuser IJE, Yassouridis A, Holsboer F (1994). The combined dexamethasone/CRH test: a refined laboratory test for psychiatric disorders. J Psychiatr Res 28: 341–356.
Holsboer F, Barden N (1996). Antidepressants and hypothalamic-pituitary-adrenocortical regulation. Endocr Rev 17: 187–205.
Holsboer F, Lauer CJ, Schreiber W, Krieg JC (1995). Altered hypothalamic-pituitary-adrenocortical regulation in healthy subjects at high familial risk for affective disorders. Neuroendocrinology 62: 340–347.
Jensen JB, Jessop DS, Harbuz MS, Mørk A, S C, Mikkelsen JD (1999). Acute and long-term treatments with the selective serotonin reuptake inhibitor citalopram modulate the HPA axis activity at different levels in male rats. J Neuroendocrinol 11: 465–471.
Kontaxakis V, Markianos M, Vaslamatzis G, Markidis M, Kanellos P, Stefanis C (1987). Multiple neuroendocrinological responses in borderline personality disorder patients. Acta Psychiatr Scand 76: 593–597.
Krishnan KRR, Davidson JR, Rayasam K, Shope F (1984). The dexamethasone suppression test in borderline personality disorder. Biol Psychiatry 19: 1149–1153.
Lahmeyer HW, Reynolds III CF, Kupfer DJ, King R (1989). Biologic markers in borderline personality disorder: a review. J Clin Psychiatry 50: 217–225.
Levine S, Dent G, De Kloet ER (2000). Stress-hyporesponsive period. In: Fink G (ed). Encyclopedia of Stress. 1st edn. Academic Press: San Diego, New York, London, pp 518–526.
Lim AT (2000). Corticotropine releasing factor (CRF). In: Fink G (ed). Encyclopedia of Stress. 1st edn. Academic Press: San Diego, New York, London, pp 578–581.
Ma XM, Lightman SL (1998). The arginine vasopressin and corticotrophin-releasing hormone gene transcription responses to varied frequencies of repeated stress in rats. J Physiol 510: 605–614.
Oitzl MS, Workel JO, Fluttert M, Frosch F, De Kloet ER (2000). Maternal deprivation affects behaviour from youth to senescence: amplification of individual differences in spatial learning and memory in senescent Brown Norway rats. Eur J Neurosci 12: 3771–3780.
Okugawa G, Omori K, Suzukawa J, Fujiseki Y, Kinoshita T, Inagaki C (1999). Long-term treatment with antidepressants increases glucocorticoid receptor binding and gene expression in cultured rat hippocampal neurons. J Neuroendocrinol 11: 887–895.
Pfohl B, Blum N, Zimmerman M (1995). Structured Interview For DSM-IV Personality Disorders. Department of Psychiatry, The University of Iowa, USA.
Plotsky PM, Meaney MJ (1993). Early postnatal experience alters hypothalamic corticotropin-releasing factor (CRF) mRNA, median eminence CRF content and stress-induced release in adult rats. Molecular Brain Res 18: 195–200.
Rinne T, Brink van den W, Westenberg HGM, Tilburg van W (2002). Fluvoxamine treatment does not affect blunted neuroendocrine responses to m-chlorophenylpiperazine in female BPD Patients. submitted.
Rinne T, De Kloet ER, Wouters L, Goekoop JG, de Rijk R, Brink van den W (2002). Hyperresponsiveness of the hypothalamus-pituitary-adrenal axis to combined dexamethasone/corticotropin-releasing hormone challenge in female borderline personality disorder subjects with a history of sustained childhood abuse. Biol Psychiatry. in press.
Rinne T, Westenberg HGM, Den Boer JA, Brink van den W (2000). Serotonergic blunting to meta-chlorophenylpiperazine (m-CPP) highly correlates with sustained childhood abuse in impulsive and autoaggressive female borderline patients. Biol Psychiatry 47: 548–556.
Rowe W, Steverman A, Walker M, Sharma S, Barden N, Seckl JR et al (1997). Antidepressants restore hypothalamic-pituitary-adrenal feedback function in aged, cognitively-impaired rats. Neurobiol Aging 18: 527–533.
Schotte CKW, Donker dD, Vankerkhoven C, Vertommen H, Cosyns P (1998). Self-report assessment of DSM-IV personality disorders. Measurement of trait and distress characteristics: the ADP-IV. Psychol Med 28: 1179–1188.
Seckl JR, Fink G (1992). Antidepressants increase glucocorticoid and mineralocorticoid receptor mRNA expression in rat hippocampus in vivo. Neuroendocrinology 55: 621–626.
Soloff PH, George A, Nathan RS (1982). The dexamethasone suppression test in patients with borderline personality disorders. Am J Psychiatry 139: 1621–1623.
Steiner M, Martin S, Wallace JE, Goldman SJ (1984). Distinguishing subtypes within the borderline domain: a combined psychoneuroendocrine approach. Biol Psychiatry 19: 907–911.
Sternbach HA, Fleming J, Extein I, Pottash ALC, Gold MS (1983). The dexamethasone suppression and thyrotropin-releasing hormone tests in depressed borderline patients. Psychoneuroendocrinology 8: 459–462.
Szabo ST, de Montigny C, Blier P (1999). Modulation of noradrenergic neuronal firing by selective serotonin reuptake blockers. Br J Pharmacol 126: 568–571.
Szabo ST, de Montigny C, Blier P (2000). Progressive attenua-tion of the firing activity of locus coeruleus nor-adrenergic neurons by sustained administration of selective serotonin reuptake inhibitors. Int J Neuropsychopharmacol 3: 1–11.
ter Smitten MH, Smeets RMW, Brink van den W (1997). Composite International Diagnostic Interview, Core Version 2.1. Dutch translation, 1 edn. Amsterdam: WHO-CIDI Training and Reference Center, Academic Medical Center University of Amsterdam.
Valentino RJ, Foote SL, Aston-Jones G (1983). Corticotropin-releasing factor activates noradrenergic neurons of the locus coeruleus. Brain Res 270: 363–367.
von Bardeleben U, Holsboer F, Stalla GK, Muller OA (1985). Combined administration of human corticotropin-releasing factor and lysine vasopressin induces cortisol escape from dexamethasone suppression in healthy subjects. Life Sci 37: 1613–1618.
Weaver TL, Clum GA (1993). Early family environments and traumatic experiences associated with borderline personality disorder. J Consulting Clin Psychol 61: 1068–1075.
WHO (1997). Composite International Diagnostic Interview, Core Version 2.1. Geneve: WHO.
Yehuda R (1998). Psychoneuroendocrinology of post-traumatic stress disorder. Psychiatr Clin North Am 21: 359–379.
Yehuda R, Southwick S, Krystal JH, Bremner JD, Charney DS, Mason JW (1993). Enhanced suppression of cortisol following dexamethasone administration in posttraumatic stress disorder. Am J Psychiatry 150: 83–86.
Yehuda R, Southwick S, Nussbaum G, Wahby V, Giller EL, Mason JW (1990). Low urinary cortisol excretion in patients with posttraumatic stress disorder. J Nerv Ment Dis 178: 366–369.
Zanarini MC, Frankenburg FR, Dubo ED, Sickel AE, Trikha A, Levin A (1998). Axis I comorbidity of borderline personality disorder. Am J Psychiatry 155: 1733–1739.
Acknowledgements
This study was supported by grants from the De Geestgronden Institute of Mental Health Care, the Stichting tot Steun of Vereniging Bennekom, and the National Fund for Mental Health Grant No: 4820, Solvay Pharma and Ferring B.V. None of the authors has conflicting interests which interfere with the integrity of the contents of the article.
The authors express their sincere appreciation to Wouter van Ewijk, chief executive officer of De Geestgronden Institute of Mental Health Care for providing the grant and facilities that made this study possible; Emiel Gans, Wijtske Kielstra, Rietta Oberink, Elise Ruys, and Jan van Zaane for conducting the interviews and patient supervision during the study; Karine Zuidgeest and Marga Wierikx for coordination of the study; Veronique van der Grient and the women from the Service Centre for their administrative support; and Nel Draijer for her valuable advice.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rinne, T., de Kloet, E., Wouters, L. et al. Fluvoxamine Reduces Responsiveness of HPA Axis in Adult Female BPD Patients with a History of Sustained Childhood Abuse. Neuropsychopharmacol 28, 126–132 (2003). https://doi.org/10.1038/sj.npp.1300003
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1300003
Keywords
This article is cited by
-
Cortisol and IL-6 Responses to Stress in Female Children Presenting at a Sexual Abuse Clinic
Journal of Child & Adolescent Trauma (2014)