Abstract
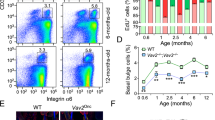
While important in carcinogenesis, the role of Ras in normal self-renewing tissues such as epidermis is unclear. To address this, we altered Ras function in undifferentiated and differentiating epidermal layers. Ras blockade within undifferentiated basal epidermal cells leads to decreased integrin expression, diminished growth capacity and induction of differentiation. Ras blockade in post-mitotic suprabasal epidermis exerts no effect. In contrast, regulated Ras and Raf activation inhibits differentiation. These findings indicate that spatially restricted Ras/Raf signaling divides epidermis into an undifferentiated proliferative compartment and a differentiating post-mitotic compartment and suggest a new role for Ras in tissue homeostasis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 50 print issues and online access
$259.00 per year
only $5.18 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout







Similar content being viewed by others
References
Bailleul B, Surani MA, White S, Barton SC, Brown K, Blessing M, Jorcano J, Balmain A . 1990 Cell 62: 697–708
Brown K, Strathdee D, Bryson S, Lambie W, Balmain A . 1998 Curr. Biol. 8: 516–524
Choate KA, Kinsella TM, Williams ML, Nolan GP, Khavari PA . 1996a Hum. Gene Ther. 7: 2247–2253
Choate KA, Medalie DA, Morgan JR, Khavari PA . 1996b Nat. Med. 2: 1263–1267
Crespo P, Leon J . 2000 Cell. Mol. Life Sci. 57: 1613–1636
Dale BA, Gown AM, Fleckman P, Kimball JR, Resing KA . 1987 J. Invest. Dermatol. 88: 306–313
de Rooij J, Bos JL . 1997 Oncogene 14: 623–625
Deng H, Choate KA, Lin Q, Khavari PA . 1998 BioTechniques 25: 274–280
Dlugosz AA, Cheng C, Williams EK, Dharia AG, Denning MF, Yuspa SH . 1994 Cancer Res. 54: 6413–6420
Elenbaas B, Spirio L, Koerner F, Fleming MD, Zimonjic DB, Donaher JL, Popescu NC, Hahn WC, Weinberg RA . 2001 Genes Dev. 15: 50–65
Esteban LM, Vicario-Abejon C, Fernandez-Salguero P, Fernandez-Medarde A, Swaminathan N, Yienger K, Lopez E, Malumbres M, McKay R, Ward JM, Pellicer A, Santos E . 2001 Molec. Cell. Biol. 21: 1444–1452
Ewen ME . 2000 Prog. Cell. Cycle Res. 4: 1–17
Feig LA, Cooper GM . 1988 Mol. Cell. Biol. 8: 3235–3243
Ferbeyre G, de Stanchina E, Querido E, Baptiste N, Prives C, Lowe SW . 2000 Genes Dev. 14: 2015–2027
Gille H, Downward J . 1999 J. Biol. Chem. 274: 22033–22040
Greenhalgh DA, Quintanilla MI, Orengo CC, Barber JL, Eckhardt JN, Rothnagel JA, Roop DR . 1993a Cancer Res. 53: 5071–5075
Greenhalgh DA, Rothnagel JA, Quintanilla MI, Orengo CC, Gagne TA, Bundman DS, Longley MA, Roop DR . 1993b Mol. Carcinog. 7: 99–110
Haase I, Hobbs RM, Romero MR, Broad S, Watt FM . 2001 J. Clin. Invest. 108: 527–536
Hahn WC, Counter CM, Lundberg AS, Beijersbergen RL, Brooks MW, Weinberg RA . 1999 Nature 400: 464–468
Halfar K, Rommel C, Stocker H, Hafen E . 2001 Development 128: 1687–1696
Ise K, Nakamura K, Nakao K, Shimizu S, Harada H, Ichise T, Miyoshi J, Gondo Y, Ishikawa T, Aiba A, Katsuki M . 2000 Oncogene 19: 2951–2956
Ivanyi D, Ansink A, Groeneveld E, Hageman PC, Mooi WJ, Heintz AP . 1989 J. Pathol. 159: 7–12
Johnson L, Greenbaum D, Cichowski K, Mercer K, Murphy E, Schmitt E, Bronson RT, Umanoff H, Edelmann W, Kucherlapati R, Jacks T . 1997 Genes Dev. 11: 2468–2481
Kinsella TM, Nolan GP . 1996 Hum. Gene Ther. 7: 1405–1413
Konieczny SF, Drobes BL, Menke SL, Taparowsky EJ . 1989 Oncogene 4: 473–481
Kozma L, Baltensperger K, Klarlund J, Porras A, Santos E, Czech MP . 1993 Proc. Natl. Acad. Sci. USA 90: 4460–4464
Li A, Simmons PJ, Kaur P . 1998 Proc. Natl. Acad. Sci. USA 95: 3902–3907
Lin AW, Lowe SW . 2001 Proc. Natl. Acad. Sci. USA 98: 5025–5030
Mainiero F, Murgia C, Wary KK, Curatola AM, Pepe A, Blumemberg M, Westwick JK, Der CJ, Giancotti FG . 1997 EMBO J. 16: 2365–2375
Malumbres M, Perez De Castro I, Hernandez MI, Jimenez M, Corral T, Pellicer A . 2000 Mol. Cell. Biol. 20: 2915–2925
Marshall CJ . 1999 Biochem. Soc. Trans. 27: 363–370
Olson EN, Spizz G, Tainsky MA . 1987 Mol. Cell. Biol. 7: 2104–2111
Pelengaris S, Littlewood T, Khan M, Elia G, Evan G . 1999 Mol. Cell. 3: 565–577
Pierceall WE, Goldberg LH, Tainsky MA, Mukhopadhyay T, Ananthaswamy HN . 1991 Mol. Carcinog. 4: 196–202
Qui MS, Green SH . 1992 Neuron 9: 705–717
Robbins PB, Lin Q, Goodnough JB, Tian H, Chen X, Khavari PA . 2001 Proc. Natl. Acad. Sci. USA 98: 5193–5198
Roop DR, Lowy DR, Tambourin PE, Strickland J, Harper JR, Balaschak M, Spangler EF, Yuspa SH . 1986 Nature 323: 822–824
Roovers K, Assoian RK . 2000 Bioessays 22: 818–826
Roper E, Weinberg W, Watt FM, Land H . 2001 EMBO Rep. 2: 145–150
Ruiz-Hidalgo MJ, Garces C, Laborda J . 1999 Int. J. Oncol. 14: 777–783
Schmidt M, Goebeler M, Posern G, Feller SM, Seitz CS, Brocker EB, Rapp UR, Ludwig S . 2000 J. Biol. Chem. 275: 41011–41017
Schulze A, Lehmann K, Jefferies HB, McMahon M, Downward J . 2001 Genes Dev. 15: 981–994
Seitz CS, Lin Q, Deng H, Khavari PA . 1998 Proc. Natl. Acad. Sci. USA 95: 2307–2312
Serrano M, Lin AW, McCurrach ME, Beach D, Lowe SW . 1997 Cell 88: 593–602
Shi B, Isseroff RR . 2000 Biochem. Cell Biol. 78: 469–476
Shields JM, Pruitt K, McFall A, Shaub A, Der CJ . 2000 Trends Cell Biol. 10: 147–154
Stewart S, Guan KL . 2000 J. Biol. Chem. 275: 8854–8862
Stockschlader MA, Schuening FG, Graham TC, Storb R . 1994 Gene Ther. 1: 317–322
Takahashi H, Honnma M, Ishida-Yamamoto A, Namikawa K, Kiyama H, Iizuka H . 2001 J. Biol. Chem. 276: 36632–36638
Umanoff H, Edelmann W, Pellicer A, Kucherlapati R . 1995 Proc. Natl. Acad. Sci. USA 92: 1709–1713
Vasioukhin V, Bauer C, Degenstein L, Wise B, Fuchs E . 2001 Cell 104: 605–617
Vassar R, Rosenberg M, Ross S, Tyner A, Fuchs E . 1989 Proc. Natl. Acad. Sci. USA 86: 1563–1567
Watt FM . 1998 Philos. Trans. R. Soc. Lond. B. Biol. Sci. 353: 831–837
White MA, Nicolette C, Minden A, Polverino A, Van Aelst L, Karin M, Wigler MH . 1995 Cell 80: 533–541
Woods D, Cherwinski H, Venetsanakos E, Bhat A, Gysin S, Humberg M, Bray PF, Saylor VL, McMahon M . 2001 Mol. Cell Biol. 21: 3192–3205
Woods D, Parry D, Cherwinski H, Bosch E, Lees E, McMahon M . 1997 Mol. Cell. Biol. 17: 5598–5611
Yuspa SH . 1994 Cancer Res. 54: 1178–1189
Yuspa SH, Vass W, Scolnick E . 1983 Cancer Res. 43: 6021–6030
Zhu AJ, Haase I, Watt FM . 1999 Proc. Natl. Acad. Sci. USA 96: 6728–6733
Acknowledgements
Supported by the USVA Office of Research and Development and AR43799 and AR45192, AR44012 from the NIAMS, NIH. M Dajee is a recipient of an NRSA Award from NIAMS. We thank M Lazarov, O Oro, J Ferrell, R Roth, Q Lin and D Kingsley for helpful discussions and pre-submission review. We thank E Fuchs for the K14 promoter, D Roop for the HK1 promoter, H Greulich for RasN17, M McMahon for Raf mutants, S Lowe for RasV12 and L Van Aelst for RasV12 S35, C40 and G37 mutants.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dajee, M., Tarutani, M., Deng, H. et al. Epidermal Ras blockade demonstrates spatially localized Ras promotion of proliferation and inhibition of differentiation. Oncogene 21, 1527–1538 (2002). https://doi.org/10.1038/sj.onc.1205287
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.onc.1205287
Keywords
This article is cited by
-
Cutis verticis gyrata and Noonan syndrome: report of two cases with pathogenetic variant in SOS1 gene
Italian Journal of Pediatrics (2022)
-
Expression of Mammalian BM88/CEND1 in Drosophila Affects Nervous System Development by Interfering with Precursor Cell Formation
Neuroscience Bulletin (2019)
-
Paracrine signalling during ZEB1-mediated epithelial–mesenchymal transition augments local myofibroblast differentiation in lung fibrosis
Cell Death & Differentiation (2019)
-
Interrogating the protein interactomes of RAS isoforms identifies PIP5K1A as a KRAS-specific vulnerability
Nature Communications (2018)
-
Ras signaling is essential for skin development
Oncogene (2014)