Abstract
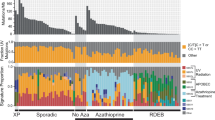
It is widely accepted that disruption of the hedgehog-patched pathway is a key event in development of basal cell cancer. In addition to patched gene alterations, p53 gene mutations are also frequent in basal cell cancer. We determined loss of heterozygosity in the patched and p53 loci as well as sequencing the p53 gene in tumors both from sporadic and hereditary cases. A total of 70 microdissected samples from tumor and adjacent skin were subjected to PCR followed by fragment analysis and DNA sequencing. We found allelic loss in the patched locus in 6/8 sporadic basal cell cancer and 17/19 hereditary tumors. All sporadic and 7/20 hereditary tumors showed p53 gene mutations. Loss of heterozygosity in the p53 locus was rare in both groups. The p53 mutations detected in hereditary tumors included rare single nucleotide deletions and unusual double-base substitutions compared to the typical ultraviolet light induced missense mutations found in sporadic tumors. Careful microdissection of individual tumors revealed genetically linked subclones with different p53 and/or patched genotype providing an insight on time sequence of genetic events. The high frequency and co-existence of genetic alterations in the patched and p53 genes suggest that both these genes are important in the development of basal cell cancer.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 50 print issues and online access
$259.00 per year
only $5.18 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Aszterbaum M, Epstein J, Oro A, Douglas V, LeBoit PE, Scott MP, Epstein Jr EH . 1999 Nat. Med. 5: 1285–1291
Berg C, Hedrum A, Holmberg A, Pontén F, Uhlen M, Lundeberg J . 1995 Clin. Chem. 41: 1461–1466
Brash DE, Pontén J . 1998 Cancer Surv. 32: 69–113
Brash DE, Rudolph JA, Simon JA, Lin A, Mckenna GJ, Baden HP, Halperin AJ, Pontén J . 1991 Proc. Natl. Acad. Sci. USA 88: 10124–10128
D'Errico M, Calcagnile A, Canzona F, Didona B, Posteraro P, Cavalieri R, Corona R, Vorechovsky I, Nardo T, Stefanini M, Dogliotti E, Rebel H, Mosnier LO, Berg RJ, Westerman-de Vries A, van Steeg H, van Kranen HJ, de Gruijl FR . 2000 Oncogene 19: 463–467
Futreal PA, Barrett JC, Wiseman RW . 1991 Nucleic Acids Res. 19: 6977
Gailani MR, Bale AE . 1997 J. Natl. Cancer Inst. 89: 1103–1108
Gailani MR, Leffell DJ, Ziegler A, Gross EG, Brash DE, Bale AE . 1996 J. Natl. Cancer Inst. 88: 349–354
Gallagher RP, Hill GB, Bajdik CD, Fincham S, Coldman AJ, McLean DI, Threlfall WJ . 1995 Arch. Dermatol. 131: 157–163
Green A, Battistutta D, Hart V, Leslie D, Weedon D . 1996 Am. J. Epidemiol. 144: 1034–1040
Greenblatt MS, Bennett WP, Hollstein M, Harris CC . 1994 Cancer Res. 54: 4855–4878
Gyapay G, Morissette J, Vignal A, Dib C, Fizames C, Millasseau P, Marc S, Bernardi G, Lathrop M, Weissenbach J . 1994 Nat. Genet. 7: 246–339
Hahn H, Wiking C, Zaphiropoulos PG, Gailani MR, Shanley S, Chidambaram A, Vorechovsky I, Holmberg E, Unden AB, Gillies S, Negus K, Smyth I, Pressman C, Leffell DJ, Gerrard B, Goldstein AM, Dean M, Toftgard R, Chenevix-Trench G, Wainwright B, Bale AE . 1996 Cell 85: 841–851
Hollstein M, Sidransky D, Vogelstein B, Harris CC . 1991 Science 253: 49–53
Holmberg E, Rozell BL, Toftgard R, Rebel H, Mosnier LO, Berg RJ, Westerman-de Vries A, van Steeg H, van Kranen HJ, de Gruijl FR . 1996 Br. J. Cancer 74: 246–250
Johnson RL, Rothman AL, Xie J, Goodrich LV, Bare JW, Bonifas JM, Quinn AG, Myers RM, Cox DR, Epstein Jr EH, Scott MP . 1996 Science 272: 1668–1671
Jonason AS, Kunala S, Price GJ, Restifo RJ, Spinelli HM, Persing JA, Leffell DJ, Tarone RE, Brash DE . 1996 Proc. Natl. Acad. Sci. USA 93: 14025–14029
Jones MH, Nakamura Y . 1992 Genes Chrom. Cancer 5: 89–90
Kawanishi S, Hiraku Y, Oikawa S . 2001 Mutat. Res. 488: 65–76
Knudson AG, Hethcote HW, Brown BW, Levine AJ . 1975 Proc. Natl. Acad. Sci. USA 72: 5116–5120
Ling G, Persson Å, Berne B, Lundeberg J, Pontén F . 2001 Am. J. Pathol. 159: 1247–1253
Moles JP, Moyret C, Guillot B, Jeanteur P, Guilhou JJ, Theillet C, Basset-Seguin N . 1993 Oncogene 8: 583–588
Nilsson M, Unden AB, Krause D, Malmqwist U, Raza K, Zaphiropoulos PG, Toftgard R . 2000 Proc. Natl. Acad. Sci. USA 97: 3438–3443
Pontén F, Berg C, Ahmadian A, Ren Z-P, Nistér M, Lundeberg J, Uhlén M, Pontén J . 1997 Oncogene 15: 1059–1067
Pontén F, Berne B, Ren Z, Nistér M, Pontén J . 1995 J. Invest. Dermatol. 105: 402–406
Ratner D, Peacocke M, Zhang H, Ping XL, Tsou HC . 2001 J. Am. Acad. Dermatol. 44: 293–297
Rebel H, Mosnier LO, Berg RJ, Westerman-de Vries A, van Steeg H, van Kranen HJ, de Gruijl FR . 2001 Cancer Res. 61: 977–983
Ren Z-P, Ahmadian A, Pontén F, Nistér M, Berg C, Lundeberg J, Uhlén M, Pontén J . 1997 Am. J. Pathol. 150: 1791–1803
Ren Z-P, Hedrum A, Pontén F, Nistér M, Ahmadian A, Lundeberg J, Uhlén M, Pontén J . 1996 Oncogene 12: 765–773
Sarasin A . 1999 Mutat. Res. 428: 5–10
Tabata H, Nagano T, Ray A, Flanagan N, Birch-MacHin M, Rees J . 1999 J. Invest. Dermatol. 113: 972–976
Taipale J, Beachy PA, Levine AJ . 2001 Nature 411: 349–354
Toftgard R . 2000 Cell. Mol. Life Sci. 57: 1720–1731
Undén AB, Zaphiropoulos PG, Bruce K, Toftgård R, Ståhle-Bäckdahl M . 1997 Cancer Res. 57: 2336–2340
Williams C, Pontén F, Ahmadian A, Ren ZP, Ling G, Rollman O, Ljung A, Jaspers NG, Uhlen M, Lundeberg J, Pontén J . 1998 Cancer Res. 58: 2449–2455
Zhang H, Ping XL, Lee PK, Wu XL, Yao YJ, Zhang MJ, Silvers DN, Ratner D, Malhotra R, Peacocke M, Tsou HC . 2001 Am. J. Pathol. 158: 381–385
Ziegler A-M, Leffell DJ, Kunala S, Sharma HW, Gailani M, Simon JA, Halperin AJ, Baden HP, Shapiro PE, Bale AE, Brash DE . 1993 Proc. Natl. Acad. Sci. USA 90: 4216–4220
Acknowledgements
This study was supported by grants from The Swedish Cancer Foundation and The Foundation for Strategic Research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ling, G., Ahmadian, A., Persson, Å. et al. PATCHED and p53 gene alterations in sporadic and hereditary basal cell cancer. Oncogene 20, 7770–7778 (2001). https://doi.org/10.1038/sj.onc.1204946
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.onc.1204946
Keywords
This article is cited by
-
Rezidivrisiko minimieren
Der Deutsche Dermatologe (2021)
-
Vorgehen beim Basalzellkarzinom
Der Onkologe (2021)
-
Diagnostik und Therapie des Basalzellkarzinoms
Der Hautarzt (2020)
-
Ocular manifestations in Gorlin-Goltz syndrome
Orphanet Journal of Rare Diseases (2019)
-
Therapiespektrum wird größer
Der Deutsche Dermatologe (2019)