Abstract
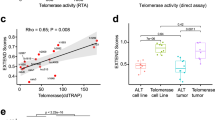
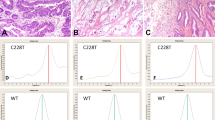
Human telomerase is expressed in germ tissues and in the majority of primary tumors. Cell renewal tissues and some pre-cancerous tissues also have weak telomerase activity. Yet, neither the exact location and frequency of telomerase-positive cells nor the changes in telomerase expression during differentiation or carcinogenesis of individual cells are known. This paper reports on the expression of hTERT (telomerase reverse transcriptase) protein in tumor and non-tumor colorectal tissues by Western blotting and tissue sections by immuno-histochemistry using antibodies raised against partial peptides of hTERT. Though telomerase activity and hTERT expression at both mRNA and protein levels were generally higher in tumor part than in non-tumor part, these two were not always correlated: expression of hTERT did not always give rise to high telomerase activity. Colonic carcinoma cell nuclei were stained with anti-hTERT antibodies but not with antigen-preabsorbed antibodies. In normal mucosa, hTERT protein was expressed, though weaker than in carcinoma, in all colonic crypt epithelial cells except those at the tip; the expressing-cell distribution was much wider than that of Ki-67 positive cells which were located at the bottom of the crypt. Isolated crypt contained a significant level of hTERT protein revealed by Western blotting, while having very weak telomerase activity. Telomerase activity was detected in epithelial cells only at the bottom half of the crypt. Specific hTERT-staining was positive in tissue lymphocytes but negative in almost all other stromal cells. It is of interest to see whether a significant level of hTERT expression with low telomerase activity is characteristic of physiologically regenerating tissues containing stem cells. In situ detection of the hTERT protein will permit further analysis of cancer diagnosis and stem cell differentiation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 50 print issues and online access
$259.00 per year
only $5.18 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Abbreviations
- RT – PCR:
-
reverse transcribed-polymerase chain reaction
- TRAP:
-
telomeric repeat amplification protocol
- hTERT:
-
human telomerase reverse transcriptase
- hTERC:
-
human telomerase RNA component
- hTEP1:
-
human telomerase protein 1
References
Avilion AA, Piatyszek MA, Gupta J, Shay JW, Bacchetti S and Greider CW. . 1996 Cancer Res. 56: 645–650.
Feng J, Funk WD, Wang SS, Weinrich SL, Avilion AA, Chiu CP, Adams RR, Chang E, Allsopp RC and Yu J. . 1995 Science 269: 1236–1241.
Harle Bachor C and Boukamp P. . 1996 Proc. Natl. Acad. Sci. USA 93: 6476–6481.
Harrington L, McPhail T, Mar V, Zhou W, Oulton R, Bass MB, Arruda I and Robinson MO. . 1997a Science 275: 973–977.
Harrington, L, Zhou W, McPhail T, Oulton R, Yeung DS, Mar V, Bass MB and Robinson MO. . 1997b Genes Dev. 11: 3109–3115.
Hiyama E, Tatsumoto N, Kodama T, Hiyama K, Shay JW and Yokoyama T. . 1996 Int. J. Oncol. 9: 453–458.
Hiyama K, Hirai Y, Kyoizumi S, Akiyama M, Hiyama E, Piatyszek MA, Shay JW, Ishioka S and Yamakido M. . 1995 J. Immunol. 155: 3711–3715.
Kilian A, Bowtell DD, Abud HE, Hime GR, Venter DJ, Keese PK, Duncan EL, Reddel RR and Jefferson RA. . 1997 Hum. Mol. Genet. 6: 2011–2019.
Kim NW, Piatyszek MA, Prowse KR, Harley CB, West MD, Ho PL, Coviello GM, Wright WE, Weinrich SL and Shay JW. . 1994 Science 266: 2011–2015.
Kolquist KA, Ellisen LW, Counter CM, Meyerson M, Tan LK, Weinberg RA, Haber DA and Gerald WL. . 1998 Nat. Genet. 19: 182–186.
Kuniyasu H, Domen T, Hamamoto T, Yokozaki H, Yasui W, Tahara H and Tahara E. . 1997 Jpn. J. Cancer Res. 88: 103–107.
Li H, Zhao LL, Funder JW and Liu JP. . 1997 J. Biol. Chem. 272: 16729–16732.
Meyerson M, Counter CM, Eaton EN, Ellisen LW, Steiner P, Caddle SD, Ziaugra L, Beijersbergen RL, Davidoff MJ, Liu Q, Bacchetti S, Haber DA and Weinberg RA. . 1997 Cell 90: 785–795.
Nakamura TM, Morin GB, Chapman KB, Weinrich SL, Andrews WH, Lingner J, Harley CB and Cech TR. . 1997 Science 277: 955–959.
Nakayama J, Saito M, Nakamura H, Matsuura A and Ishikawa F. . 1997 Cell 88: 875–884.
Nakayama J, Tahara H, Tahara E, Saito M, Ito K, Nakamura H, Nakanishi T, Tahara E, Ide T and Ishikawa F. . 1998 Nature Genet. 18: 65–68.
Ohyashiki K, Ohyashiki JH, Nishimaki J, Toyama K, Ebihara Y, Kato H, Wright WE and Shay JW. . 1997 Cancer Res. 57: 2100–2103.
Shay JW and Bacchetti S. . 1997 Eur. J. Cancer 33: 787–791.
Tahara H, Kuniyasu H, Yokozaki H, Yasui W, Shay JW, Ide T and Tahara E. . 1995 Clin. Cancer Res. 1: 1245–1251.
Yasui W, Akama Y, Kuniyasu H, Yokozaki H, Semba S, Shimamoto F and Tahara E. . 1996 J. Pathol. 180: 122–128.
Acknowledgements
We thank Drs K Inada and M Tatematsu (Aichi Cancer Center Institute) for technical suggestions of crypt isolation and Dr J Carl Barrett (National Institute of Environmental Health Sciences, NIH) for critical reading of and useful comments on this manuscript. This work was supported in part by Grant-in-Aid for Cancer Research and a Grant-in-Aid for Scientific Research on Priority Areas from the Ministry of Education, Science, Sports, and Culture of Japan.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Tahara, H., Yasui, W., Tahara, E. et al. Immuno-histochemical detection of human telomerase catalytic component, hTERT, in human colorectal tumor and non-tumor tissue sections. Oncogene 18, 1561–1567 (1999). https://doi.org/10.1038/sj.onc.1202458
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.onc.1202458
Keywords
This article is cited by
-
TERT Genetic Mutations as Prognostic Marker in Glioma
Molecular Neurobiology (2017)
-
A novel biomarker TERTmRNA is applicable for early detection of hepatoma
BMC Gastroenterology (2010)
-
RNA interference-mediated c-MYC inhibition prevents cell growth and decreases sensitivity to radio- and chemotherapy in childhood medulloblastoma cells
BMC Cancer (2009)
-
Expression profile and prognostic importance in prostate lesions of the reverse transcriptase component of human telomerase (hTERT) and of cyclin-dependent kinase inhibitor p57 (p57kip2a)
International Urology and Nephrology (2009)
-
Metachronous cancer development in patients with sporadic colorectal adenomas—multivariate risk model with independent and combined value of hTERT and survivin
International Journal of Colorectal Disease (2008)