Abstract
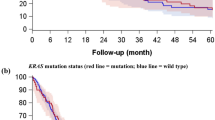
This study was performed to clarify the different effects of each mutant exon of p53 as indicators of a poor prognosis in patients with non-small cell lung cancer (NSCLC). Tumor tissues of 204 patients with NSCLC were analysed; 96 tumors were stage I, 22 stage II, and 86 stage III. DNA was extracted from frozen specimens and polymerase chain reaction-single strand conformation polymorphism (PCR–SSCP) and direct sequencing were performed to investigate mutations of p53 from exon 5 to exon 8. Seventy-five patients with NSCLC (36.8%) had mutations in p53 which included 72 cases of missense mutations and three cases of non-missense mutations. The overall survival rate of patients with mutant p53 adenocarcinomas was strikingly worse than that of patients whose tumors had wild-type p53 (35.7% vs 53.8%; P=0.041), but no significant difference in survival was found in the patients with NSCLC and squamous cell carcinoma. Mutations in exon 5 of p53 occurred in 33 cases (16.2%), mutation in exon 6 was detected in only one case (0.5%), mutations in exon 7 in 20 cases (9.8%), and mutations in exon 8 in 18 cases (8.8%). The overall survival rate of patients with mutations in exon 7 was worse than that of patients with wild-type p53 in NSCLCs and adenocarcinomas (42.9% vs 56.0%; P=0.025 and 33.3% vs 53.8%; P=0.048, respectively), whereas the overall survival of patients with mutations in exon 5 was almost the same as that of patients with wild-type p53. In addition, the overall survival rate of patients with mutations in exon 8 was strikingly worse than that of patients with wild-type p53 in NSCLCs, adenocarcinomas and squamous cell carcinomas (22.9% vs 56.0%; P<0.001, 19.0% vs 53.8%; P=0.004 and 33.3% vs 62.5%; P=0.042, respectively). Multivariate analysis with the Cox regression model of patients with NSCLC, adenocarcinoma and squamous cell carcinoma indicated that mutations in exon 8 were best correlated with the overall survival rate, followed by lymph node status (P<0.001, P=0.015 and P=0.006, respectively), and mutations in exon 7 of NSCLC were also revealed to have good correlation, followed by lymph node status and mutations in exon 8 (P=0.031). Mutation of p53 was a poor prognostic factor for adenocarcinoma as described previously. Moreover, mutations in exon 8 were more useful indicators of prognosis not only for adenocarcinoma but also for NSCLC. Worse overall survival of the patients with mutations in exon 8 of p53 was suggested to be associated with codon 273 mutations as well as mutations between codon 280 and 285 included into the H2 α helix corresponding to residues 278–286. These results suggested that abnormal conformation of H2 α helix might play an important role not only in the loss of normal function but also in the acquisition of tumorigenesis. Investigation of mutations in exon 8, especially codon 273 mutation and mutant H2 α helix was considered to be a clinically useful approach for determining the prognosis of patients with NSCLC.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 50 print issues and online access
$259.00 per year
only $5.18 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Huang, Cl., Taki, T., Adachi, M. et al. Mutations in exon 7 and 8 of p53 as poor prognostic factors in patients with non-small cell lung cancer. Oncogene 16, 2469–2477 (1998). https://doi.org/10.1038/sj.onc.1201776
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.onc.1201776
Keywords
This article is cited by
-
Chemopreventive effects of NSAIDs as inhibitors of cyclooxygenase-2 and inducers of apoptosis in experimental lung carcinogenesis
Molecular and Cellular Biochemistry (2012)
-
Specific TP53 mutations predict aggressive phenotype in head and neck squamous cell carcinoma: a retrospective archival study
Head & Neck Oncology (2011)
-
A combined histologic and molecular approach identifies three groups of gastric cancer with different prognosis
Virchows Archiv (2009)
-
Replacing PCR with COLD-PCR enriches variant DNA sequences and redefines the sensitivity of genetic testing
Nature Medicine (2008)
-
Assessing TP53 status in human tumours to evaluate clinical outcome
Nature Reviews Cancer (2001)