Abstract
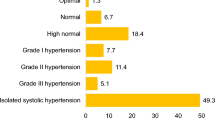
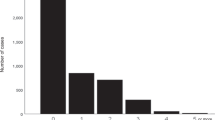
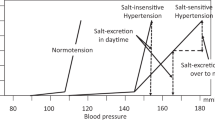
The objective of the present study was to determine the prevalence of symptoms generally attributed to hypertension and the relationship between symptoms and blood pressure categories. Routine office blood pressure measurement in the morning was obtained and morning symptoms were reported using a standardized questionnaire in a multicenter study from general practitioners in Germany. Dizziness and headaches were significantly (P<0.001) more prevalent in 2154 untreated hypertensives (19.6 and 17.0%) as compared with 1399 normotensives (13.6 and 7.4%), whereas tiredness was less in hypertensives (12.0 vs 17.0%, P<0.01). In untreated and in 52 469 treated hypertensives, the overall prevalence of symptoms increased constantly with blood pressure levels from 26.1% in untreated male patients with mild hypertension to 54.3% of female patients with severe treated hypertension, with a higher prevalence in women (+7% vs men) and in patients with concomitant diseases (+13% vs patients without concomitant diseases). The prevalence of symptoms in older patients with untreated isolated systolic hypertension was not different from younger normotensives. There was a tight positive correlation between systolic and diastolic blood pressure and dizziness (R=0.73 and 0.76) as well as headaches (R=0.83 and 0.90) for all blood pressure levels in all patient groups. Typical hypertension-attributed symptoms like dizziness and headaches are more prevalent in hypertensives and they are closely related to blood pressure levels in untreated and treated hypertensives. Morning symptoms in hypertensives may suggest that there is inadequate control of blood pressure. More attention should be paid to perceived symptoms in hypertensives.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Page IH . Hypertension: a symptomless but dangerous disease. N Engl J Med 1972; 287: 665–666.
Kullman S, Svardsudd K . Differences in perceived symptoms/quality of life in untreated hypertensive and normotensive men. Scand J Prim Health Care 1990; 1(Suppl): 47–53.
Marques-Vidal P, Tuomilehto J . Hypertension awareness, treatment and control in the community: is the ‘rule of halves’ still valid? J Hum Hypertens 1997; 11: 213–220.
Gasse C, Hense HW, Stieber J, Doring A, Liese AD, Keil U . Assessing hypertension management in the community: trends of prevalence, detection, treatment, and control of hypertension in the MONICA Project, Augsburg 1984–1995. J Hum Hypertens 2001; 15: 27–36.
Wolf-Maier K, Cooper R, Banegas JR, Giampaoli S, Hense HW, Joffres M et al. Hypertension prevalence and blood pressure levels in 6 European countries, Canada, and the United States. JAMA 2003; 289: 2363–2369.
Nunes MI . The relationship between quality of life and adherence to treatment. Curr Hypertens Rep 2001; 3: 462–465.
Mamon J, Green L, Levine DM, Gibson G, Gurley HT . Using the emergency department as a screening site for high blood pressure. A method for improving hypertension detection and appropriate referral. Med Care 1987; 25: 770–780.
Angard N, Chez RA, Young C . Personal health among midlife women hospital employees. J Womens Health 1998; 7: 1289–1293.
Williams GH . Beyond blood pressure control. Effect of antihypertensive therapy on quality of life. Am J Hypertens 1988; 1(Suppl): 363S–365S.
Di Tullio M, Alli C, Avanzini F, Bettelli G, Colombo F, Devoto MA et al. Prevalence of symptoms generally attributed to hypertension or its treatment: study on blood pressure in elderly outpatients (SPAA). J Hypertens 1988; 6(Suppl 1): S87–S90.
Kjellgren KI, Ahlner J, Dahlof B, Gill H, Hedner T, Saljo R . Perceived symptoms amongst hypertensive patients in routine clinical practice—a population-based study. J Intern Med 1998; 244: 325–332.
Erickson SR, Williams BC, Gruppen LD . Perceived symptoms and health-related quality of life reported by uncomplicated hypertensive patients compared to normal controls. J Hum Hypertens 2001; 15: 539–548.
Dimenas ES, Wiklund IK, Dahlöf CG, Lindvall KG, Olofsson BK, De Faire UH . Differences in the subjective well-being and symptoms of normotensives, borderline hypertensives and hypertensives. J Hypertens 1989; 7(11): 885–890.
MacDonald LA, Sackett DL, Haynes RB, Taylor DW . Labelling in hypertension: a review of the behavioural and psychological consequences. J Chronic Dis 1984; 37(12): 933–942.
Mena-Martin FJ, Martin-Escudero JC, Simal-Blanco F, Carretero-Ares JL, Arzua-Mouronte D, Herreros-fernandez V . Health-related quality of subjects with known and unknown hypertension: results from the population-based Hortega study. J Hypertens 2003; 21: 1283–1289.
Sigurdsson JA, Bengtsson C . Symptoms and signs in relation to blood pressure and antihypertensive treatment. A cross-sectional and longitudinal population study of middle-aged Swedish women. Acta Med Scand 1983; 213: 183–190.
Hoel D, Howard RB . Hypertension: stalking the silent killer. Postgrad Med 1997; 101: 116–121.
Vandenburg MJ, Evans SJ, Kelly BJ, Bradshaw F, Currie WJ, Cooper WD . Factors affecting the reporting of symptoms by hypertensive patients. Br J Clin Pharmacol 1984; 18(Suppl 2): 189S–195S.
Franklin SS, Pio JR, Wong ND, Larson MG, Leip EP, Vasan RS, Levy D . Predictors of new-onset diastolic and systolic hypertension: the Framingham Heart Study. Circulation 2005; 111: 1121–1127.
Bloom BS . Continuation of initial antihypertensive medication after 1 year of therapy. Clin Ther 1998; 20: 671–681.
Kottke TE, Tuomilehto J, Puska P, Salonen JT . The relationship of symptoms and blood pressure in a population sample. Int J Epidemiol 1979; 8: 355–359.
Wood WG, Elias MF, Schultz NR, Pentz III CA . Symptoms reported on the Cornell Medical Index in relationship to hypertension and age. Exp Aging Res 1978; 4: 421–431.
Wiklund I, Halling K, Ryden-Bergsten T, Fletcher A . Does lowering the blood pressure improve the mood? Quality-of-life results from the Hypertension Optimal Treatment (HOT) study. Blood Press 1997; 6: 357–364.
Middeke M, Lemmer B, Schaaf B, Eckes L . Prevalence of hypertension attributed symptoms: results of a large-scale, primary-care study conducted in Germany. Int Soc Hypertens 2006, 64 abstr.
Acknowledgements
Parts of these data were presented at the 21st Scientific Meeting of the International Society of Hypertension, 2006, Fukuoka, Japan (ref. 24). This work was supported by Boehringer Ingelheim Pharma, Germany.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Middeke, M., Lemmer, B., Schaaf, B. et al. Prevalence of hypertension-attributed symptoms in routine clinical practice: a general practitioners-based study. J Hum Hypertens 22, 252–258 (2008). https://doi.org/10.1038/sj.jhh.1002305
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jhh.1002305
Keywords
This article is cited by
-
A benchmark for machine-learning based non-invasive blood pressure estimation using photoplethysmogram
Scientific Data (2023)
-
A three-year longitudinal study of healthy lifestyle behaviors and adherence to pharmacological treatments in newly diagnosed patients with acute coronary syndrome: hierarchical linear modeling analyses
Journal of Public Health (2022)
-
Self-management and psychological resilience moderate the relationships between symptoms and health-related quality of life among patients with hypertension in China
Quality of Life Research (2019)
-
Supporting the self-management of hypertension: Patients’ experiences of using a mobile phone-based system
Journal of Human Hypertension (2016)