Abstract
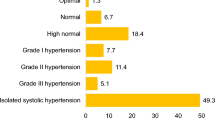
The aim of this observational study was to assess whether there were differences in perception of overall cardiovascular risk (OCVR) in hypertensive patients depending on the gender of the primary care provider (PCP). We performed this study in 2003: 2979 male PCPs (MPCPs) and 562 female PCPs (FPCPs) participated throughout France. The patients included were hypertensive either treated or untreated, uncontrolled (blood pressure (BP) ⩾140/90 mm Hg) with at least one other cardiovascular risk factor (CVRF) associated. OCVR of patients was both calculated according to French Agence Nationale d'Accréditation et d'Evaluation en Santé guidelines for uncontrolled hypertensive patients and subjectively estimated by the PCP as ‘low’, ‘moderate’, ‘high’ or ‘very high’. About 11 770 patients were included, mean age was 63.7±11.2 years and 54.1% were men. Mean BP was 157±13/90±9 mm Hg. According to French guidelines, the calculated OCVR was ‘moderate’ in 23.7% of patients, ‘high’ in 47.5% and ‘very high’ in 28.8%. The PCP perceived OCVR was that 9.1% of patients were considered to be at ‘low risk’, 40.7% at ‘moderate risk’, 38.1% at ‘high risk’, and only 11.2% at ‘very high risk’ (OCVR was not estimated for 0.9% of patients). The overall agreement rate between the PCPs’ estimation of OCVR and its calculation was 43.5%. Thus, in spite of extensive diffusion of ANAES guidelines, we found that PCPs in France generally underestimated OCVR though there were no significant differences between male and female physicians (45% for FPCPs and 43.2% for MPCPs).
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Strasser R . The doctor–patient relationship in general practice. Med J Aust 1992; 156(5): 334–338.
Tarrant C, Windridge K, Boulton M, Baker R, Freeman G . How important is personal care in general practice? BMJ 2003; 326(7402): 1310.
Hall JA, Roter DL . Do patients talk differently to male and female physicians? A meta-analytic review. Patient Educ Couns 2002; 48(3): 217–224.
Roter DL, Hall JA, Aoki Y . Physician gender effects in medical communication: a meta-analytic review. JAMA 2002; 288(6): 756–764.
Roter DL, Hall JA . Physician gender and patient-centered communication: a critical review of empirical research. Annu Rev Public Health 2004; 25: 497–519.
Frank E, Harvey LK . Prevention advice rates of women and men physicians. Arch Fam Med 1996; 5(4): 215–219.
1999 World Health Organization-International Society of Hypertension Guidelines for the Management of Hypertension. Guidelines Subcommittee. J Hypertens 1999; 17(2): 151–183.
2003 European Society of Hypertension-European Society of Cardiology. Guidelines for the management of arterial hypertension. J Hypertens 2003; 21(6): 1011–1053.
Wolf-Maier K, Cooper RS, Kramer H, Banegas JR, Giampaoli S, Joffres MR et al. Hypertension treatment and control in five European countries, Canada, and the United States. Hypertension 2004; 43(1): 10–17.
Amar J, Vaur L, Perret M, Bailleau C, Etienne S, Chamontin B . Hypertension in high-risk patients: beware of the underuse of effective combination therapy (results of the PRATIK study). J Hypertens 2002; 20(4): 779–784.
Brindle P, Emberson J, Lampe F, Walker M, Whincup P, Fahey T et al. Predictive accuracy of the Framingham coronary risk score in British men: prospective cohort study. BMJ 2003; 327(7426): 1267.
Conroy RM, Pyorala K, Fitzgerald AP, Sans S, Menotti A, De Backer G et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: the SCORE project. Eur Heart J 2003; 24(11): 987–1003.
Acknowledgements
We thank the contribution of all participating investigators without whom the study would not have been possible.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Baguet, JP., Fiquet, B., Yau, C. et al. Attitudes to and application of the concept of overall cardiovascular risk: comparison of male and female primary care providers. J Hum Hypertens 21, 359–365 (2007). https://doi.org/10.1038/sj.jhh.1002155
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jhh.1002155