Abstract
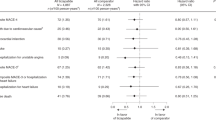
Our objective was to review all published trials of coenzyme Q10 for hypertension, assess overall efficacy and consistency of therapeutic action and side effect incidence. Meta-analysis was performed in 12 clinical trials (362 patients) comprising three randomized controlled trials, one crossover study and eight open label studies. In the randomized controlled trials (n=120), systolic blood pressure in the treatment group was 167.7 (95% confidence interval, CI: 163.7–171.1) mm Hg before, and 151.1 (147.1–155.1) mm Hg after treatment, a decrease of 16.6 (12.6–20.6, P<0.001) mm Hg, with no significant change in the placebo group. Diastolic blood pressure in the treatment group was 103 (101–105) mm Hg before, and 94.8 (92.8–96.8) mm Hg after treatment, a decrease of 8.2 (6.2–10.2, P<0.001) mm Hg, with no significant change in the placebo group. In the crossover study (n=18), systolic blood pressure decreased by 11 mm Hg and diastolic blood pressure by 8 mm Hg (P<0.001) with no significant change with placebo. In the open label studies (n=214), mean systolic blood pressure was 162 (158.4–165.7) mm Hg before, and 148.6 (145–152.2) mm Hg after treatment, a decrease of 13.5 (9.8–17.1, P<0.001) mm Hg. Mean diastolic blood pressure was 97.1 (95.2–99.1) mm Hg before, and 86.8 (84.9–88.8) mm Hg after treatment, a decrease of 10.3 (8.4–12.3, P<0.001) mm Hg. We conclude that coenzyme Q10 has the potential in hypertensive patients to lower systolic blood pressure by up to 17 mm Hg and diastolic blood pressure by up to 10 mm Hg without significant side effects.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Wilson PW . An epidemiologic perspective of systemic hypertension, ischemic heart disease, and heart failure. Am J Cardiol 1997; 80 (9B): 3J–8J.
Overvad K, Diamant B, Holm L, Holmer G, Mortensen SA, Stender S . Coenzyme Q10 in health and disease. Eur J Clin Nutr 1999; 53 (10): 764–770.
Langsjoen PH, Langsjoen AM . Overview of the use of CoQ10 in cardiovascular disease. Biofactors 1999; 9 (2–4): 273–284.
Yamagami T, Shibata N . Bioenergetics in clinical medicine: studies on coenzyme Q10 and essential hypertension. Res Comm Chem Path Pharmacol 1975; 11 (2): 273–288.
Langsjoen PH, Folkers K . Long-term efficacy and safety of coenzyme Q10 therapy for idiopathic dilated cardiomyopathy. Am J Cardiol 1990; 65 (7): 521–523.
Watts GF, Castelluccio C, Rice-Evans C, Taub NA, Baum H, Quinn PJ . Plasma coenzyme Q (ubiquinone) concentrations in patients treated with simvastatin. J Clin Pathol 1993; 46 (11): 1055–1057.
Hodgson JM, Watts GF, Playford DA, Burke V, Croft KD . Coenzyme Q10 improves blood pressure and glycaemic control: a controlled trial in subjects with type 2 diabetes. Eur J Clin Nutr 2002; 56 (11): 1137–1142.
Deeks JJ, Altman DG, Bradburn MJ . Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. In: Egger M, Smith GD, Altman DG (eds). Systematic Reviews in Health Care: Meta-Analysis in Context, 2nd edn. BMJ Publishing Group: London, UK, pp 285–312.
Flather MD, Farkouh ME, Pogue JM, Yusuf S . Strengths and limitations of meta-analysis: larger studies may be more reliable. Control Clin Trials 1997; 18 (6): 568–579 Discussion 661–666.
StataCorp. STATA, In. 8.2 edn. StataCorp: College Station, 2005.
Sterne JAC, Bradburn MJ, Egger M . Meta-analysis in stata. In: Egger M, Smith GD, Altman DG (eds). Systematic Reviews in Health Care: Meta-Analysis in Context, 2nd edn. BMJ Publishing Group: London, UK, pp 347–369.
Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF . Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of reporting of meta-analyses. Lancet 1999; 354 (9193): 1896–1900.
Yamagami T, Shibata N, Folkers K . Bioenergetics in Clinical Medicine VIII: administration of coenzyme Q10 to patients with essential hypertension. Res Comm Chem Path Pharmacol 1976; 14 (4): 721–727.
Yamagami T, Shibata N, Folkers K . Study of coenzyme Q10 in essential hypertension. In: Folkers K, Yamamura Y (eds). Biomedical & Clinical Aspects of Coenzyme Q. Elsevier, Biomedical Press: North Holland, 1977, pp 231–242.
Folkers K, Drzewoski J, Richardson PC, Ellis J, Shizukuiski S, Baker L . Bioenergetics in clinical medicine XVI: reduction of hypertension in patients by therapy with coenzyme Q10. Res Comm Chem Path Pharmacol 1981; 31 (1): 129–140.
Montaldo PL, Fadda G, Salis G, Satta G, Tronci M, DiCesare R et al. Effects of the prolonged administration of coenzyme Q10 in borderline hypertensive patients: a hemodynamic study. In: Folkers K, Littarru GP, Yamagami T (eds). Biomedical & Clinical Aspects of Coenzyme Q. Elsevier Science Publishers: Amsterdam, North Holland, 1991, pp 417–424.
Digiesi V, Cantini F, Bisi G, Guarino GC, Oradei A, Littarru GP . Mechanism of action of coenzyme Q10 in essential hypertension. Curr Ther Res 1992; 51 (5): 668–672.
Digiesi V, Cantini F, Oradei A, Bisi G, Guarino GC, Brocchi A et al. Coenzyme Q10 in essential hypertension. Mol Aspects Med 1994; 15 (Suppl): s257–s263.
Langsjoen P, Willis R, Folkers K . Treatment of essential hypertension with coenzyme Q10. Mol Aspects Med 1994; 15 (Suppl): S265–S272.
Yamagami T, Takagi M, Akagami H, Kubo H, Toyama S, Okamoto T et al. Effect of coenzyme Q10 on essential hypertension: a double blind controlled study. In: Folkers K, Yamamura Y (eds). Biomedical & Clinical Aspects of Coenzyme Q. Elsevier Science Publishers BV: Amsterdam, North Holland, 1986, pp 337–343.
Singh RB, Niaz MA, Rastogi SS, Shukla PK, Thakur AS . Effect of hydrosoluble coenzyme Q10 on blood pressures and insulin resistance in hypertensive patients with coronary artery disease. J Hum Hypertens 1999; 13 (3): 203–208.
Burke BE, Neuenschwander R, Olson RD . Randomized, double-blind, placebo-controlled trial of coenzyme Q10 in isolated systolic hypertension. South Med J 2001; 94 (11): 1112–1117.
Digiesi V, Cantini F, Brodbeck B . Effect of coenzyme Q10 on essential arterial hypertension. Curr Ther Res 1990; 47 (5): 841–845.
Molyneux S, Florkowski C, Lever M, George P . The bioavailability of coenzyme Q10 supplements available in New Zealand differs markedly. NZ Med J 2004; 117 (1203): U1108.
Satoh K, Ichihara K . Lipophilic HMG-CoA reductase inhibitors increase myocardial stunning in dogs. J Cardiovasc Pharmacol 2000; 35 (2): 256–262.
Baggio E, Gandini R, Plancher AC, Passeri M, Carmosino G . Italian multicenter study on the safety and efficacy of coenzyme Q10 as adjunctive therapy in heart failure. CoQ10 Drug Surveillance Investigators. Mol Aspects Med 1994; 15 (Suppl): s287–s294.
Turnbull F . Effects of different blood-pressure-lowering regimens on major cardiovascular events: results of prospectively-designed overviews of randomised trials. Lancet 2003; 362 (9395): 1527–1535.
Koska J, Syrova D, Blazicek P, Marko M, Grna JD, Kvetnansky R et al. Malondialdehyde, lipofuscin and activity of antioxidant enzymes during physical exercise in patients with essential hypertension. J Hypertens 1999; 17 (4): 529–535.
Grunfeld S, Hamilton CA, Mesaros S, McClain SW, Dominiczak AF, Bohr DF et al. Role of superoxide in the depressed nitric oxide production by the endothelium of genetically hypertensive rats. Hypertension 1995; 26 (6 Part 1): 854–857.
Watts GF, Playford DA, Croft KD, Ward NC, Mori TA, Burke V . Coenzyme Q(10) improves endothelial dysfunction of the brachial artery in Type II diabetes mellitus. Diabetologia 2002; 45 (3): 420–426.
Groneberg DA, Kindermann B, Althammer M, Klapper M, Vormann J, Littarru GP et al. Coenzyme Q10 affects expression of genes involved in cell signalling, metabolism and transport in human CaCo-2 cells. Int J Biochem Cell Biol 2005; 37 (6): 1208–1218.
Linnane AW, Eastwood H . Cellular redox poise modulation; the role of coenzyme Q10, gene and metabolic regulation. Mitochondrion 2004; 4 (5–6): 779–789.
Acknowledgements
Steven Joseph Haas previously received assistance via a National Health and Medical Research Council Public Health Postgraduate Research Scholarship, Scholarship application I.D. no. 237059. We acknowledge financial support for the Cardiac Surgical Research Unit from Pharma Nord Aps, Denmark, and Blackmores, Australia.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rosenfeldt, F., Haas, S., Krum, H. et al. Coenzyme Q10 in the treatment of hypertension: a meta-analysis of the clinical trials. J Hum Hypertens 21, 297–306 (2007). https://doi.org/10.1038/sj.jhh.1002138
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jhh.1002138
Keywords
This article is cited by
-
Mitochondrial impairment but not peripheral inflammation predicts greater Gulf War illness severity
Scientific Reports (2023)
-
The Possible Role of Nutraceuticals in the Prevention of Cardiovascular Disease
High Blood Pressure & Cardiovascular Prevention (2019)
-
Nutraceuticals: Reviewing their Role in Chronic Disease Prevention and Management
Pharmaceutical Medicine (2019)
-
The Effects of Coenzyme Q10 Supplementation on Blood Pressures Among Patients with Metabolic Diseases: A Systematic Review and Meta-analysis of Randomized Controlled Trials
High Blood Pressure & Cardiovascular Prevention (2018)
-
Oral CoQ10 attenuates high salt-induced hypertension by restoring neurotransmitters and cytokines in the hypothalamic paraventricular nucleus
Scientific Reports (2016)