Abstract
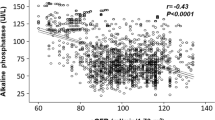
A reduction in renal function is associated with high cardiovascular morbidity and mortality in hypertension. The aim of the present study was to investigate the relationship between creatinine clearance and subclinical organ damage in 957 never previously treated, middle-aged patients with primary hypertension. Renal function was estimated by means of the serum creatinine level using the Cockcroft–Gault formula; left ventricular hypertrophy (LVH) was determined according to electrocardiographic criteria; and retinal vascular changes were evaluated by direct ophthalmoscopy. Creatinine clearance was, on the average, 83±21.2 ml/min, and the prevalence of LVH and retinopathy was 13 and 49%, respectively. Creatinine clearance was inversely related to the duration of disease (r=−0.132, P<0.0001), systolic blood pressure (r=−0.110, P=0.001), serum glucose (r=−0.090, P=0.007), total cholesterol (r=−0.196, P<0.0001), and LDL-cholesterol (r=−0.196, P<0.0001). Patients in the lower quintile of creatinine clearance showed a higher prevalence of electrocardiogram (ECG) determined LVH (P=0.04), as well as retinal changes (P=0.02). The risk of having LVH or retinal vascular changes increases significantly with each s.d. decrease in creatinine clearance, regardless of traditional cardiovascular risk factors. Moreover, patients with ECG-determined LVH and retinal changes showed lower creatinine clearance as compared to those with lesser degrees of target organ involvement (P<0.01). In conclusion, a mild reduction in creatinine clearance is associated with preclinical end-organ damage in patients with normal creatinine and primary hypertension. These data may help explain the high cardiovascular mortality observed in patients with renal dysfunction. Routine evaluation of creatinine clearance could be useful for identifying patients at higher cardiovascular risk.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Schillaci G, Reboldi G, Verdecchia P . High-normal serum creatinine concentration is a predictor of cardiovascular risk in essential hypertension. Arch Intern Med 2001; 161: 886–891.
Jensen JS et al. Arterial hypertension, microalbuminuria, and risk of ischemic heart disease. Hypertension 2000; 35: 898–903.
Culleton BF et al. Cardiovascular disease and mortality in a community-based cohort with mild renal insufficiency. Kidney Int 1999; 56: 2214–2219.
Kronenberg F et al. Lipoprotein(a) serum concentrations and apolipoprotein(a) phenotypes in mild and moderate renal failure. J Am Soc Nephrol 2000; 11: 105–115.
Fliser D et al. Insulin resistance and hyperinsulinemia are already present in patients with incipient renal disease. Kidney Int 1998; 53: 1343–1347.
Cockcroft DW, Gault MH . Prediction of creatinine clearance from serum creatinine. Nephron 1976; 16: 31–41.
Ruilope LM et al. Renal function and intensive lowering of blood pressure in hypertensive participants of the hypertension optimal treatment (HOT) study. J Am Soc Nephrol 2001; 12: 218–225.
Sokolow M, Perloff D . The prognosis of essential hypertension treated conservatively. Circulation 1981; 23: 697–713.
Guidelines Committee. The sixth report of Joint National Committee on prevention, detection, evaluation and treatment of high blood pressure. Arch Intern Med 1997; 157: 2413–2446.
Guidelines Subcommittee. World Health Organization/International Society of Hypertension (WHO/ISH) guidelines for the management of hypertension. J Hypertens 1999; 17: 151–183.
Schouten EG, Vandenbroucke JP, van der Heide-Wessel C, van der Heide RM . Retinopathy as an independent indicator of all-causes mortality. Int J Epidemiol 1986; 15: 234–236.
Pontremoli R et al. Prevalence and clinical correlates of microalbuminuria in essential hypertension. The MAGIC study. Hypertension 1997; 30: 1135–1143.
Sokolow M, Lyon TP . The ventricular complex in left ventricular hypertrophy as obtained by unipolar precordial and limb reads. Am Heart J 1949; 37: 161–186.
Molloy TJ, Okin PM, Devereux RB, Kligfield P . Electrocardiographic detection of left ventricular hypertrophy by the simple QRS voltage-duration product. J Am Coll Cardiol 1992; 20: 1180–1186.
Keith NM, Wagener HP, Barker MW . Some different types of essential hypertension: their course and prognosis. Am J Med Sci 1974; 268: 336–345.
Shulman NB et al. Prognostic value of serum creatinine and effect of treatment of hypertension on renal function. Results from the hypertension detection and follow-up program. The Hypertension Detection and Follow-up Program Cooperative Group. Hypertension 1989; 13: 180–193.
Pahor M et al. Diuretic-based treatment and cardiovascular events in patients with mild renal dysfunction enrolled in the systolic hypertension in the elderly program. Arch Intern Med 1998; 158: 1340–1345.
JF et al. Renal insufficiency as a predictor of cardiovascular outcomes and the impact of ramipril: the HOPE randomized trial. Ann Intern Med 2001; 134: 629–636.
Perrone RD, Madias NE, Levey AS . Serum creatinine as an index of renal function: new insight into old concepts. Clin Chem 1992; 38: 1933–1953.
Vakili BA, Okin PM, Devereux RB . Prognostic implications of left ventricular hypertrophy. Am Heart J 2001; 141: 334–341.
Devereux RB et al. Cost-effectiveness of echocardiography and electrocardiography for detection of left ventricular hypertrophy in patients with systemic hypertension. Hypertension 1987; 9: 69–76.
Levy D . Left ventricular hypertrophy. Epidemiological insights from the Framingham Heart Study. Drugs 1988; 35: 1–5.
Cuspidi C et al. Evaluation of target organ damage in arterial hypertension: which role for qualitative funduscopic examination? Ital Heart J 2001; 2: 702–706.
Wong TY et al. Retinal microvascular abnormalities and incident stroke; The Atherosclerosis Risk in Communities Study. Lancet 2001; 358: 1134–1140.
Duncan BB et al. Hypertensive retinopathy and incident coronary heart disease in high risk men. Br J Ophthalmol 2002; 86: 1002–1006.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Leoncini, G., Viazzi, F., Parodi, D. et al. Creatinine clearance and signs of end-organ damage in primary hypertension. J Hum Hypertens 18, 511–516 (2004). https://doi.org/10.1038/sj.jhh.1001689
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jhh.1001689
Keywords
This article is cited by
-
DBnorm as an R package for the comparison and selection of appropriate statistical methods for batch effect correction in metabolomic studies
Scientific Reports (2021)
-
Routine management of locally advanced cervical cancer with concurrent radiation and cisplatin. Five-year results
BMC Women's Health (2006)