Abstract
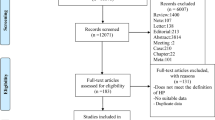
The aim of the study was to review published evidence on whether blood pressure (BP) levels and the prevalence of hypertension are higher in adult populations of African descent living in the UK as compared to the white population. A systematic literature review was carried out using MEDLINE 1966–2002 and EMBASE 1980–2002 and citations from references. In all, 14 studies were identified. Nearly all studies were carried out in the London area. The data showed important differences between studies in terms of age and sex of samples, definition of African/black and methods of evaluating BP. A total of 10 studies reported higher mean systolic BPs, while 11 studies reported higher mean diastolic BPs in men from African descent compared to white men. In women, 10 of 12 studies reported higher systolic, and 10 of 12 studies reported higher diastolic BPs. For prevalence of hypertension, eight of 10 studies reported higher rates in men from African descent; eight of nine studies showed higher rates of hypertension in women from African descent. Overall, the most representative sample and up-to-date data came from the Health Survey for England '99. Ethnic group differences in BP were not present in the younger age groups. Women of African descent had higher BP and higher body mass index (BMI). In men of African descent high BP did not coincide with higher BMI. In conclusion, the reported higher rates of hypertension in people from African descent in the UK are confirmatory of the USA African-American and white comparisons. Variations in study methods, size and body composition, and in the mix of Afro-Caribbean and West African groups explain much of the inconsistent results in the UK studies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Cruickshank JK et al. Similarity of blood pressure in blacks, whites and Asians in England: The Birmingham Factory Study. J Hypertens 1985; 3: 365–371.
Senior PA, Bhopal R . Ethnicity as variable in epidemiological research. BMJ 1994; 309: 327–330.
Meade TW et al. Ethnic groups comparisons of variables associated with ischaemic heart disease. Br Heart J 1978; 40: 789–795.
Sever PS et al. Ethnic differences in blood pressure with observation on nor-adrenaline and renin. Clin Exp Hypertens 1979; 1: 733–744.
Cruickshank JK et al. Blood pressure in black, white and Asian factory workers in Birmingham. Postgrad Med J 1983; 59: 622–626.
Haines AP, Boorof A, Goldenberg E . Blood pressure, smoking, obesity and alcohol consumption in blacks and whites in general practice. J Hum Hypertens 1987; 1: 39–46.
Miller GJ et al. Dietary and other characteristics relevant for coronary heart disease in men of Indian, West Indian and European descent in London. Atherosclerosis 1988; 70: 63–72.
Cruickshank JK et al. Ethnic differences in fasting plasma C-peptide and insulin in relation to glucose tolerance and blood pressure. Lancet 1991; 338: 842–847.
McKeigue PM, Shah B, Marmot MG . Relation of central obesity and insulin resistance with high diabetes prevalence and cardiovascular risk in South Asians. Lancet 1991; 337: 382–386.
Chaturvedi N, McKeigue PM, Marmot MG . Resting and ambulatory Blood pressure differences in Afro-Caribbeans and Europeans. Hypertension 1993; 22: 90–96.
Cappuccio FP, Cooj DG, Atkinson RW, Wicks PD . The Wandsworth Heart and Stroke Study. A population-based survey of cardiovascular risk factors in different ethnic groups. Methods and baseline findings. Nutr Metab Cardiovasc Dis 1998; 8: 371–385.
Whitty CJM et al. Differences in biological risk factors for cardiovascular disease between three ethnic groups in the Whitehall II study. Atherosclerosis 1999; 142: 279–286.
Primatesta P, Bost L, Poulter NR . Blood pressure levels and hypertension status among ethnic groups in England. J Hum Hypertens 2000; 14: 143–148.
Karlsen S, Primatesta P, McMum A . Blood Pressure. Chapter 7 In: Erens B, Primatesta P, Prior G. Health Survey for England—The Health of Minority Ethnic Groups '99. London, The Stationary Office, 2001, pp 175–197.
Cruickshank JK et al. Hypertension in four African-origin populations: current ‘Rule of Halves’, quality of blood pressure control and attributable risk of cardiovascular disease. J Hypertens 2001; 19: 41–46.
Lane D, Beevers DG, Lip GYH . Ethnic differences in blood pressure and prevalence of hypertension in England. J Hum Hypertens 2002; 16: 267–273.
Pacy PJ et al. Prevalence of hypertension in white, black and Asian diabetic in a district hospital diabetic clinic. Diabetic Med 1984; 2: 125–130.
Khattar RS, Swales JD, Senior R, Lahiri A . Racial variation in cardiovascular morbidity and mortality in essential hypertension. Heart 2000; 83: 267–271.
Rowlands DB . Intra-arterial blood pressure and cardiovascular responses in black and white hypertensives. Postgrad Med J 1981; 57: 772–773.
World Health Organisation. Hypertension Control: Report of a WHO Expert Committee. Geneva: WHO, 1996.
Gill PS, Kai J, Bhopal RS, Wild S . Health care needs assessment: black and minority ethnic groups. In: Raftery J (ed). Health Care Needs Assessment. The Epidemiologically Based Needs Assessment Reviews. Third Series. Abingdon: Radcliffe Medical Press Ltd. (in press), available at http://hcna.radcliffe-online.com/bemgframe.htm
Weaver MG, Park MK, Lee DH . Difference in blood pressure levels obtained by auscultatory and oscillometric methods. Am J Dis Child 1990; 144: 911–914.
Bolling K . Dinamap 8100 Calibration Study. OPCS: London, HMSO, 1994.
Pickering TG et al. How common is white coat hypertension? J Am Med Assoc 1988; 259: 225–228.
Verdecchia P . Variability between current definition of ‘normal’ ambulatory blood pressure: implications in the assessment of white coat hypertension. Hypertension 1992; 20: 555–562.
Agyemang C, Bhopal R S . Is blood pressure of South Asian adults in the UK higher or lower than that in European white adults? A review of cross-sectional data. J Hum Hypertens 2002; 16: 739–751.
De Giovanni JV, Pentecost BL, Beevers DG . The Birmingham blood pressure school study. Postgrad Med J 1983; 59: 627–629.
Khaw KT, Marmot MG . Blood pressure in 15 to 16-year-old adolescents of different ethnic groups in two London Schools. Postgrad Med J 1983; 59: 630–631.
MacMahon S, Peto R, Cutler J . Blood pressure, stroke, and coronary heart disease, Part 1, prolonged differences in blood pressure: prospective observational studies corrected for the regression dilution biases. Lancet 1990; 335: 765–774.
McKeigue PM, Sevak L . Coronary Heart Disease in South Asian Communities. London: Health Education Authority, 1994.
Hypertension Detection and Follow-up Program Co-operative Group Group. Five-year findings of the Hypertension Detection and Follow-up Program, II. Mortality by race, sex and age. J Am Med Assoc 1979; 242: 2562–2577.
Miller GJ et al. Adult male all-cause, cardiovascular and cerebrovascular mortality in relation to ethnic group, systolic blood pressure and blood glucose concentration in Trinidad, West Indies. Int J Epidemiol 1988; 17: 62.
Cruickshank JK, Beevers DG . Epidemiology of hypertension: blood pressure in blacks and whites. Clin Sci 1982; 62: 1–6.
Acknowledgements
We thank A de Jonge for her valuable advice throughout this work, S Sengupta-Wiebe for her advice during the initial literature search and Hazel King for secretarial support. We also thank Dr Kennedy Cruickshank and Dr Nishi Chaturvedi for their useful comments and Dr Lisa Riste for supplying unpublished data. We thank the anonymous referee, who provided comments that helped improve an earlier version of this paper.
Author information
Authors and Affiliations
Corresponding author
Additional information
Glossary of ethnicity termsIn extracting information from the original papers, whenever appropriate, we have taken the terms used by the authors.
Ethnicity—refers to the group individuals belong to as a result of their culture, which includes language, religion, diet, and ancestry.2
Ethnic minority group—refers to minority non-European non-white populations.
White people—refers to people with European ancestral origin.
Black people—refers to people with African ancestral origin.
Afro-Caribbean—refers to people, and their offspring, with African ancestral origin but migrating to Britain via the Caribbean islands.
Rights and permissions
About this article
Cite this article
Agyemang, C., Bhopal, R. Is the blood pressure of people from African origin adults in the UK higher or lower than that in European origin white people? A review of cross-sectional data. J Hum Hypertens 17, 523–534 (2003). https://doi.org/10.1038/sj.jhh.1001586
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jhh.1001586
Keywords
This article is cited by
-
Predictors of diastolic dysfunction in ethnic groups: observations from the Hypertensive Cohort of The Ethnic-Echocardiographic Heart of England Screening Study (E-ECHOES)
Journal of Human Hypertension (2018)
-
White Coat Hypertension and Cardiovascular Diseases: Innocent or Guilty
Current Cardiology Reports (2018)
-
Ideal cardiovascular health among Ghanaian populations in three European countries and rural and urban Ghana: the RODAM study
Internal and Emergency Medicine (2018)
-
Measurement of blood pressure for the diagnosis and management of hypertension in different ethnic groups: one size fits all
BMC Cardiovascular Disorders (2017)
-
Risk factor control in secondary prevention of cardiovascular disease: results from the multi-ethnic HELIUS study
Netherlands Heart Journal (2017)