Abstract
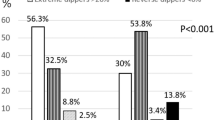
To investigate whether in recently diagnosed essential hypertensives a reduced nocturnal fall in blood pressure (BP), established on the basis of two 24-h ambulatory blood pressure monitorings (ABPM) is related to a greater cardiovascular damage. In all, 355 consecutive, recently diagnosed, never-treated essential hypertensives referred for the first time to our outpatient clinic were included in the study. Each patient underwent the following procedures: (1) two 24-h ABPMs performed within 3 weeks, (2) 24-h urinary collection for microalbuminuria, (3) nonmydriatic photography of ocular fundi, (4) echocardiography, (5) carotid ultrasonography. We defined nondipping profile as a night–day systolic and diastolic fall ⩽10 % (mean of two ABPMs). A dipper BP profile was found in 238 patients, whereas in 117 patients a nondipper profile was present. The two groups were similar for age, gender, body mass index, smoking habit, clinic BP, 48-h BP and heart rate, while, by definition, night-time systolic and diastolic BP were significantly higher in nondippers than in dippers (130/81 vs 121/74 mmHg, P< 0.0001).The prevalence of left ventricular hypertrophy (LVH) defined by four different criteria: (a) LV mass index (LVMI) ⩾125 g/m2 in both genders; (b) LVMI ⩾134 gm2 in men and ⩾110 in women; (c) LVMI⩾125 g/m2 in men and ⩾110 g/m2 in women; (d) LVMI⩾51 g/m2.7 in men and ⩾47 g/m2.7 in women was significantly higher in nondippers than in dippers (a: 12 vs 7%, P<0.05; b: 16 vs 7%, P<0.01; c: 20 vs 11%, P<0.01; d: 35 vs 23% P<0.02) and this finding was associated with a significant increase in aortic root and left atrium dimensions. There were no differences between the two groups in the prevalence of carotid and retinal changes and microalbuminuria. In conclusion our findings suggest that never-treated hypertensives with a reduced BP fall in the night time, defined on the basis of two ABPMs, have a higher prevalence of TOD than dippers, in terms of echocardiographic LVH. In this population setting, cardiac structural alterations are a more sensitive marker of the impact of the nocturnal BP load on cardiovascular system than other extracardiac signs of TOD.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Mallion JM et al. Clinical value of ambulatory blood pressure monitoring. J Hypertens 1999; 17: 585–595.
Pickering TG . The clinical significance of diurnal blood pressure variations. Dippers and nondippers. Circulation 1990; 81: 700–702.
Staessen J et al. The diurnal blood pressure profile: a population study. Am J Hypertens 1992; 5: 386–392.
Verdecchia P, Schillaci G, Porcellati G . Dippers versus nondippers. J Hypertens 1991; 9 (Suppl 2): S42–S44.
Staessen J et al. Nocturnal blood pressure fall on ambulatory monitoring in a large international database. Hypertension 1997; 29: 30–39.
White W . Diurnal blood pressure and blood pressure variability in diabetic normotensive and hypertensive subjects. J Hypertens 1992; 10 (Suppl 1): S35–S41.
Timio M et al. Nondipper hypertensive patients and progressive renal insufficiency: a 3 year longitudinal study. Clin Nephrol 1995; 43: 382–383.
Mann S et al. Circadian variation of blood pressure in autonomic failure. Circulation 1983; 68: 477–483.
Parati G . Blood pressure reduction at night: sleep and beyond. J Hypertens 2000; 18: 1725–1729.
Palatini P et al. Clinical relevance of nighttime blood pressure and of daytime blood pressure variability. Arch Intern Med 1992; 152: 1855–1860.
Pierdomenico SD et al. Arterial disease in dipper and nondipper hypertensive patients. Am J Hypertens 1997; 10: 511–518.
Bianchi S et al. Diurnal variations of blood pressure and microalbuminuria in essential hypertension. Am J Hypertens 1994; 7: 23–29.
Shimada K et al. Diurnal blood pressure variations and silent cerebrovascular damage in elderly patients with hypertension. J Hypertens 1992; 10: 875–878.
Klander L et al. Hypertension is related to cognitive impairment: a 20-year follow-up of 999 men. Hypertension 1998; 31: 780–786.
Kobrin I et al. Diurnal variation of blood pressure in elderly patients with essential hypertension. J Am Geriatr Soc 1984; 32: 896–899.
Roman MJ et al. Is the absence of a nocturnal fall in blood pressure (nondipping) associated with cardiovascular target organ damage? J Hypertens 1997; 15: 969–978.
Grandi AM et al. Relation of extent of nocturnal blood pressure decrease to cardiovascular remodelling in never-treated patients with essential hypertension. Am J Cardiol 2002; 89: 1193–1196.
Bjorklund K et al. The majority of nondipping men do not have increased cardiovascular risk: a population-based study. J Hypertens 2002; 20: 1501–1506.
Mochizuchi J et al. Limited reproducibility of circadian variation in blood pressure dippers and nondippers. Am J Hypertens 1998; 11: 403–409.
Manning G et al. Variability of diurnal changes in ambulatory blood pressure and nocturnal dipping status in untreated hypertensive and normotensive subjects. Am J Hypertens 2000; 13: 1035–1038.
Devereux RB et al. Echocardiographic determination of left ventricular mass in men. Anatomic validation of the method. Circulation 1977; 55: 613–618.
Devereux RB et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol 1986; 57: 450–458.
Wachtell K et al. Impact of different partition values on prevalence of left ventricular hypertrophy and concentric geometry in a large hypertensive population in the Life Study. Hypertension 2000; 35: 6–12.
Ganau A et al. Patterns of left ventricular hypertrophy and geometric remodelling in essential hypertension. J Am Coll Cardiol 1992; 19: 1550–1558.
Spirito P, Maron BJ . Doppler echocardiography for assessing left ventricular diastolic function. Ann Intern Med 1988; 109: 122–126.
Pignoli P et al. Intimal plus medial thickness of the arterial wall: a direct measurement with ultrasound imaging. Circulation 1986; 74: 1399–1408.
Salonen R et al. Measurement of intima-media thickness of common carotid arteries with high resolution B-mode ultrasonography: inter and intraobserver variability. Ultrasound Med Biol 1991; 17: 225–230.
Zanchetti A et al. on behalf of the ELSA Investigators. Risk factors associated with alterations in carotid intima-media thickness in hypertension: baseline data from the European Lacidipine Study on Atherosclerosis. J Hypertens 1998; 16: 949–961.
Hodis HN et al. The role of carotid arterial-intima-media thickness in predicting clinical coronary events. Ann Intern Med 1998; 128; 262–269.
Cuspidi C et al. Lack of correlation between left ventricular mass and diameter of left coronary main trunk in hypertensive patients. Am J Hypertens 1999; 12: 1163–1168.
Cuspidi C et al. Echocardiographic and ultrasonographic evaluation of cardiac and vascular hypertrophy in patients with essential hypertension. Cardiology 1992; 80; 305–310.
Dimmit SB et al. Usefulness of ophthalmoscopy in mild to moderate hypertension. Lancet 1989; i: 1103–1106.
Cuspidi C et al. Target organ damage and nondipping pattern defined by two sessions of ambulatory blood pressure monitoring in recently diagnosed essential hypertensive patients. J Hypertens 2001; 19: 1–7.
Verdecchia P et al. Circadian blood pressure changes and left ventricular hypertrophy in essential hypertension. Circulation 1990; 81: 528–536.
Dimsdale JE, Heeren MM . How reliable is nighttime blood pressure dipping? Am J Hypertens 1998; 11: 606–609.
Omboni S et al. Reproducibility and clinical value of nocturnal hypertension, prospective evidence from the SAMPLE study. J Hypertens 1998; 16: 733–738.
Ferrara A et al. Cardiovascular abnormalities in non-treated hypertensives according to nondipper status. Am J Hypertens 1998; 11: 1352–1357.
Cuspidi C et al. Impact of nocturnal fall in blood pressure on early cardiovascular changes in essential hypertension. J Hypertens 1999; 17: 1339–1344.
Kohara K et al. Autonomic nervous function in nondipper essential hypertensive subjects Evaluation by power spectral analysis of heart rate variability. Hypertension 1995; 26: 808–814.
Mancia G, Parati G . Ambulatory blood pressure monitoring and organ damage. Hypertension 2000; 36: 894–900.
Morgan TO et al. Cardiac hypertrophy depends upon sleep blood pressure: a study in rats. J Hypertens 2000; 18: 445–451.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cuspidi, C., Michev, I., Meani, S. et al. Reduced nocturnal fall in blood pressure, assessed by two ambulatory blood pressure monitorings and cardiac alterations in early phases of untreated essential hypertension. J Hum Hypertens 17, 245–251 (2003). https://doi.org/10.1038/sj.jhh.1001546
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jhh.1001546
Keywords
This article is cited by
-
Short-term blood pressure variability as a potential therapeutic target for kidney disease
Clinical Hypertension (2023)
-
Retinal vessel caliber and its relationship with nocturnal blood pressure dipping status: the SABPA study
Hypertension Research (2016)
-
Does sympathetic overactivation feature all hypertensives? Differences of sympathovagal balance according to night/day blood pressure ratio in patients with essential hypertension
Hypertension Research (2016)
-
Nocturnal blood pressure non-dipping is not associated with increased left ventricular mass index in hypertensive children without end-stage renal failure
European Journal of Pediatrics (2016)
-
Effect of telmisartan vs. ramipril on ‘dipping’ status and blood pressure variability: pooled analysis of the PRISMA studies
Hypertension Research (2014)