Abstract
It is well established that numerous errors, biases and omissions in recording blood pressure exist. This study had two objectives. Firstly, to measure the accuracy of sphygmomanometers used in general practice and secondly to assess digit bias in blood pressure recording. This study was carried out in the then Northfield PCG, which comprised 18 practices and 67 GPs. A total of 131 mercury and aneroid sphygmomanometers were tested for accuracy by a trained technician in accordance with the methods specified in BS 2743 (1990). Accuracy was defined as an error of greater than 10 mm Hg. The second part of the methodology involved undertaking an audit of the proportion of registered patients aged 35–80 years who had their blood pressure measured within the last 5 years by members of the Primary Health Care Team. The results were that of the mercury and aneroid sphygmomanometers tested, 17% were inaccurate. Of these, 4% recorded an error greater than 10 mm Hg. One percent of mercury and 10% of aneroid sphygmomanometers recorded an error greater than 10 mm Hg respectively. Sixteen (12%) sphygmomanometers were so deteriorated (air leaks, dirt in mercury) that the researcher suggested their immediate withdrawal from service. The results of the blood pressure recording audit suggested digit bias of both systolic and diastolic recordings to the nearest 10 mm Hg. This study suggests that sphygmomanometers used in general practice are very likely to be inaccurate and some may well be so deteriorated that they should be withdrawn from service. The results of the blood pressure audit showed digit bias in systolic and diastolic readings to the nearest 10 mm Hg. The implications for clinical care—both over diagnosis and under diagnosis—although not assessed are likely to be appreciable. PCG Clinical Governance teams in conjunction with Practice Clinical Leads must address these basic issues.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Ramsey LE et al. Guidelines for management of hypertension: report of the third working party of the British Hypertension Society J Hum Hypertens 1999; 13: 569–592
Markandu ND, Whitcher F, Arnold A, Carney C . The mercury sphygmomanometer should be abandoned before it is prescribed J Hum Hypertens 2000; 14: 31–36
National Institute of Health, National Heart, Lung, and Blood Institute. The Sixth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure Arch Intern Med 1997; 153: 154–183
Zanchetti A et al. The 1993 Guidelines for the management of mild hypertension: memorandum from WHO/ISH meeting Hypertension 1993; 22: 392–403
Perloff D et al. Human blood pressure determination by sphygmomanometry Circulation 1993; 88: 2460–2470
Frohlich E et al. Recommendations for human blood pressure determination by sphygmomanometers Circulation 1988; 77: 501A–514A
Derry J . Sample size for audit Managing Audit in General Practice, Summer 1993: 17–20
Bailey RH, Knaus VL, Bauer JH . Aneroid sphygmomanometers Arch Intern Med 1991; 15: 1409–1412
Burke MJ et al. Sphygmomanometers in hospital and family practice: problems and recommendations Br Med J 1982; 285: 469–471
Mion D Jr, Pierin AMG . How accurate are sphygmomanometers? J Hum Hypertens 1998; 12: 245–248
http://www.white-medical.co.uk
Acknowledgements
We are grateful to all the GPs and staff in Northfield PCG for their co-operation and support in this study. We would also like to thank Mr David Stenson, Chief Officer, and Ann Rouine, Clinical Governance Nurse Board member, for their helpful comments on the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ali, S., Rouse, A. Practice audits: reliability of sphygmomanometers and blood pressure recording bias. J Hum Hypertens 16, 359–361 (2002). https://doi.org/10.1038/sj.jhh.1001384
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jhh.1001384
Keywords
This article is cited by
-
Association Between End-Stage Liver Disease and Incident Heart Failure in an Integrated Health System
Journal of General Internal Medicine (2023)
-
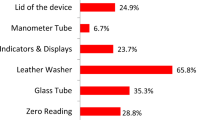
Results of a project to calibrate mercury sphygmomanometer blood pressure-measuring devices in Egypt
Journal of Human Hypertension (2021)
-
Nurse effects on measurement error in household biosocial surveys
BMC Medical Research Methodology (2020)
-
Blood pressure differences between a mercury sphygmomanometer and two automatic devices
Biomedical Engineering Letters (2015)
-
On Scales of Measurement in Autism Spectrum Disorders (ASD) and Beyond: Where Smitty Went Wrong
Journal of Autism and Developmental Disorders (2014)