Abstract
Objective:
To investigate the association between macrosomia and high weight-for-length/height in 1–3 years old Chinese infants.
Design:
A retrospective longitudinal study.
Subjects:
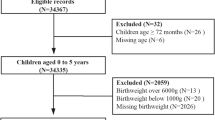
918 children aged 1–3 years in Shanghai, China.
Measurements:
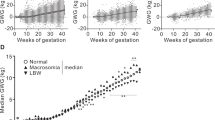
Body weight and length/height, illness status and feeding modalities were obtained during follow-up. Macrosomia was defined as birth weight ⩾90th percentile of sex specific birth weight distribution. High weight-for-length/height was defined as a weight-for-length/height z-score ⩾1.68 using the WHO growth reference.
Results:
The odds ratios (ORs) for high weight-for-length/height were 3.60 (95% confidence interval (CI), 1.74–7.42) for boys and 1.39 (95% CI, 0.51–3.81) for girls who were macrosomic compared with the nonmacrosomic counterparts after adjustment for age. The ORs were attenuated to 3.48 (95% CI, 1.63–7.43) for boys and were still nonsignificant for girls (OR, 1.38; 95% CI, 0.49–3.91) after further controlling for illness status, the age of breast-feeding cessation and the age at introduction of complementary foods. From the analysis of boys and girls combined, the ORs were 2.48 (95% CI, 1.40–4.40) with adjustment for age and sex and 2.33 (95% CI, 1.29–4.22) with all covariates.
Conclusion:
Macrosomia is an important predictor for high weight-for-length/height in Chinese children aged 1–3 years.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Taubes G . Weight increases worldwide? Science 1998; 280: 1368.
Manson JE, Willett WC, Stampfer MJ, Colditz GA, Hunter DJ, Hankinson SE et al. Body weight and mortality among women. N Engl J Med 1995; 333: 677–685.
Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath Jr CW . Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med 1999; 341: 1097–1105.
Sinha R, Fisch G, Teague B, Tamborlane WV, Banyas B, Allen K et al. Prevalence of impaired glucose tolerance among children and adolescents with marked obesity. N Engl J Med 2002; 346: 802–810.
Guo SS, Wu W, Chumlea WC, Roche AF . Predicting overweight and obesity in adulthood from body mass index values in childhood and adolescence. Am J Clin Nutr 2002; 76: 653–658.
Vanhala M, Vanhala P, Kumpusalo E, Halonen P, Takala J . Relation between obesity from childhood to adulthood and the metabolic syndrome: population based study. BMJ 1998; 317: 319.
Tanaka T, Matsuzaki A, Kuromaru R, Kinukawa N, Nose Y, Matsumoto T et al. Association between birthweight and body mass index at 3 years of age. Pediatr Int 2001; 43: 641–646.
Takahashi E, Yoshida K, Sugimori H, Miyakawa M, Izuno T, Yamagami T et al. Influence factors on the development of obesity in 3-year-old children based on the Toyama study. Prev Med 1999; 28: 293–296.
Whitaker RC . Predicting preschooler obesity at birth: the role of maternal obesity in early pregnancy. Pediatrics 2004; 114: e29–e36.
Parsons TJ, Power C, Manor O . Fetal and early life growth and body mass index from birth to early adulthood in 1958 British cohort: longitudinal study. BMJ 2001; 323: 1331–1335.
Liu S, Yao L, Chen Y, Liu Z, Sun M . Study on the trend of changes in fetal macrosomia in Yantai during the past 30 years. Chin J Obstet Gynecol 2002; 37: 469–471 (In Chinese).
Zhu L, Qin X, Qian S . Macrosomia and associated risk factors in Shanghai. Chin J Birth Heredity 2001; 9: 81–83 (In Chinese).
Sheng M, Zhao X . 10-year trends in incidence of newborn macrosomia and related factors. Shanghai Med J 2002; 25: 513–514 (In Chinese).
Wu Y . Overweight and obesity in China. BMJ 2006; 333: 362–363.
The World Health Organization. The WHO Child Growth Standards. Available from: http://www.who.int/childgrowth/standards/en/.
Baker JL, Michaelsen KF, Rasmussen KM, Sorensen TI . Maternal prepregnant body mass index, duration of breastfeeding, and timing of complementary food introduction are associated with infant weight gain. Am J Clin Nutr 2004; 80: 1579–1588.
Wilson AC, Forsyth JS, Greene SA, Irvine L, Hau C, Howie PW . Relation of infant diet to childhood health: seven year follow up of cohort of children in Dundee infant feeding study. BMJ 1998; 316: 21–25.
Ong KK, Emmett PM, Noble S, Ness A, Dunger DB, ALSPAC Study Team. Dietary energy intake at the age of 4 months predicts postnatal weight gain and childhood body mass index. Pediatrics 2006; 117: e503–e508.
Barker DJ . The fetal and infant origins of adult disease. BMJ 1990; 301: 1111.
Eriksson JG, Yliharsila H, Forsen T, Osmond C, Barker DJ . Exercise protects against glucose intolerance in individuals with a small body size at birth. Prev Med 2004; 39: 164–167.
Eriksson JG, Forsen TJ, Osmond C, Barker DJ . Pathways of infant and childhood growth that lead to type 2 diabetes. Diabetes Care 2003; 26: 3006–3010.
von Kries R, Koletzko B, Sauerwald T, von Mutius E, Barnert D, Grunert V et al. Breast feeding and obesity: cross sectional study. BMJ 1999; 319: 147–150.
Gillman MW, Rifas-Shiman SL, Camargo Jr CA, Berkey CS, Frazier AL, Rockett HR et al. Risk of overweight among adolescents who were breastfed as infants. JAMA 2001; 285: 2461–2467.
Grummer-Strawn LM, Mei Z . Does breastfeeding protect against pediatric overweight? Analysis of longitudinal data from the Centers for Disease Control and Prevention Pediatric Nutrition Surveillance System. Pediatrics 2004; 113: e81–e86.
Victora CG, Barros F, Lima RC, Horta BL, Wells J . Anthropometry and body composition of 18 year old men according to duration of breast feeding: birth cohort study from Brazil. BMJ 2003; 327: 901–906.
Dahlquist G, Bennich SS, Kallen B . Intrauterine growth pattern and risk of childhood onset insulin dependent (type I) diabetes: population based case-control study. BMJ 1996; 313: 1174–1177.
Virtanen SM, Knip M . Nutritional risk predictors of beta cell autoimmunity and type 1 diabetes at a young age. Am J Clin Nutr 2003; 78: 1053–1067.
Wei JN, Sung FC, Li CY, Chang CH, Lin RS, Lin CC et al. Low birth weight and high birth weight infants are both at an increased risk to have type 2 diabetes among schoolchildren in Taiwan. Diabetes Care 2003; 26: 343–348.
Rich-Edwards JW, Colditz GA, Stampfer MJ, Willett WC, Gillman MW, Hennekens CH et al. Birthweight and the risk for type 2 diabetes mellitus in adult women. Ann Intern Med 1999; 130: 278–284.
Freedman DS, Dietz WH, Srinivasan SR, Berenson GS . The relation of overweight to cardiovascular risk factors among children and adolescents: the Bogalusa heart s tudy. Pediatrics 1999; 103: 1175–1182.
Wang Y, Ge K, Popkin BM . Tracking of body mass index from childhood to adolescence: a 6-y follow-up study in China. Am J Clin Nutr 2000; 72: 1018–1024.
Acknowledgements
This study was supported by Ministry of Science and Technology of China (973 Program, Grant No. 2006CB503900) and Science and Technology Commission of Shanghai Municipality (Grants No. 04DZ14007). We thank all of the participants involved in this study and the health professionals who carried out the physical examination of the children.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Yu, Z., Sun, J., Haas, J. et al. Macrosomia is associated with high weight-for-height in children aged 1–3 years in Shanghai, China. Int J Obes 32, 55–60 (2008). https://doi.org/10.1038/sj.ijo.0803765
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0803765