Abstract
Objective:
To examine trends and effects of weight loss treatment on health-related quality of life (HRQL) in the severely obese over 10 years.
Design:
Swedish obese subjects (SOS) intervention study is a controlled, longitudinal trial of the health effects of weight loss in the severely obese.
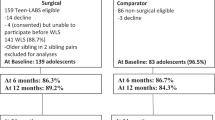
Subjects:
A total of 655 of 851 surgically treated and 621 of 852 conventionally treated obese men (body mass index, BMI⩾34) and women (BMI⩾38) who completed 10 years of the study.
Measurements:
HRQL was assessed before treatment and after 0.5, 1, 2, 3, 4, 6, 8 and 10 years.
Results:
HRQL change during the 10-year observation period largely followed phases of weight loss, weight regain and weight stability. Improvements and deteriorations in HRQL were associated with the magnitude of weight loss or regain, except regarding anxiety. Peak improvements in the surgical group were observed during the first year of weight loss, whereas the weight regain phase (mainly between 1- and 6-year follow-up) was accompanied by a gradual decline in HRQL. The period from 6- to 10-year follow-up was characterized by relatively stable observations in both weight and HRQL. At 10 years, net gains were noted in all HRQL domains compared to baseline. Comparisons of treatment effects on HRQL in the surgical vs conventional group after 10 years showed significantly better outcome in the surgical group on current health perceptions, social interaction, psychosocial functioning and depression, whereas no significant differences were found for overall mood and anxiety. Long-term results of the study suggest that a maintained weight loss of about 10% is sufficient for positive long-term effects on HRQL, a limit that was reached in about two-thirds of the surgically treated patients who completed 10 years of the study.
Conclusion:
Long-lasting weight reduction in the severely obese has a general long-standing positive outcome on HRQL. Bariatric surgery is a favorable option for the treatment of severe obesity, resulting in long-term weight loss and HRQL improvements in a majority of patients. However, difficulties among some surgical patients to control and maintain weight loss over time should not be ignored. Future research should study if the long-term efficacy of bariatric surgery may be further enhanced by implementing lifestyle modification techniques in the postoperative management of patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Östman J, Britton M, Jonsson E (eds) Treating and Preventing Obesity–An Evidence Based Review. Wiley: Weinheim, 2004.
Sullivan M, Karlsson J, Sjöström L, Taft C . Why quality-of-life measures should be used in the treatment of patients with obesity. In: Björntorp P. (ed). International Textbook in Obesity. Wiley: Chichester, 2001.
Sullivan M, Karlsson J . Quality of life. In: Östman J, BrittonM, Jonsson E (eds). Treating and Preventing Obesity – An evidence based review. Wiley: Weinheim, 2004.
Kolotkin RL, Meter K, Williams GR . Quality of life and obesity. Obes Rev 2001; 2: 219–229.
Karlsson J, Sjöström L, Sullivan M . Swedish obese subjects (SOS) – an intervention study of obesity. Two-year follow-up of health related quality of life (HRQL) and eating behavior after gastric surgery for severe obesity. Int J Obes Relat Metab Disord 1998; 21: 113–126.
Kolotkin RL, Crosby RD, Williams GR, Hartley GG, Nicol S . The relationship between health-related quality of life and weight loss. Obes Res 2001; 9: 564–571.
Karlsson J, Taft C, Sjöström L, Torgerson JS, Sullivan M . Psychosocial functioning in the obese before and after weight reduction: construct validity and responsiveness of the Obesity-related Problems scale (OP). Int J Obes Relat Metab Disord 2003; 27: 617–630.
Sarwer DB, Wadden TA, Fabricatore AN . Psychosocial and behavioral aspects of bariatric surgery. Obes Res 2005; 13: 639–648.
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K et al. Bariatric surgery: a systematic review and meta-analysis. JAMA 2004; 292: 1724–1737.
Maciejewski ML, Patrick DL, Williamson DF . A structured review of randomized controlled trials of weight loss showed little improvement in health-related quality of life. J Clin Epidemiol 2005; 58: 568–578.
Hsu LK, Benotti PN, Dwyer J, Roberts SB, Saltzman E, Shikora S et al. Nonsurgical factors that influence the outcome of bariatric surgery: a review. Psychosom Med 1998; 60: 338–346.
Sjöström L, Larsson B, Backman L, Bengtsson C, Bouchard C, Dahlgren S et al. Swedish Obese Subjects (SOS). Recruitment for an intervention study and a selected description of the obese state. Int J Obes Relat Metab Disord 1992; 16: 465–479.
Sullivan M, Karlsson J, Sjöström L, Backman L, Bengtsson C, Bouchard C et al. Swedish Obese Subjects (SOS). An intervention study of obesity. Baseline evaluation of health and psychosocial functioning in the first 1743 subjects examined. Int J Obes Relat Metab Disord 1993; 17: 503–512.
Sjöström L, Lindroos AK, Peltonen M, Torgerson J, Bouchard C, Carlsson B et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med 2004; 351: 2683–2693.
Larsson I, Berteus Forslund H, Lindroos AK, Lissner L, Naslund I, Peltonen M et al. Body composition in the SOS (Swedish Obese Subjects) reference study. Int J Obes Relat Metab Disord 2004; 28: 1317–1324.
Davies AR, Sherbourne CR, Peterson JR, Ware Jr JE . Scoring Manual: Adult Health Status and Patient Satisfaction Measures Used in RAND's Health Insurance Experiment. Santa Monica, CA: The RAND Corporation, (No. N-2190-HHS) 1988.
Karlsson J, Sjöström L, Sullivan M . Swedish Obese Subjects (SOS) – an intervention study of obesity. Measuring psychosocial factors and health by means of short-form questionnaires. Results from a method study. J Clin Epidemiol 1995; 48: 817–823.
Sjöberg L, Svensson E, Persson L . The measurement of mood. Scand J Psychol 1979; 20: 1–18.
Karlsson J, Hallgren P, Kral J, Lindroos AK, Sjöström L, Sullivan M . Predictors and effects of long-term dieting on mental well-being and weight loss in obese women. Appetite 1994; 23: 15–26.
Zigmond AS, Snaith RP . The hospital anxiety and depression scale. Acta Psychiatr Scand 1983; 67: 361–370.
Bergner M, Bobitt RA, Carter WB, Gilson BS . The sickness impact profile: development and final revision of a health status measure. Med Care 1981; 19: 787–805.
Bradley JW . Distribution-Free Statistical tests. London: Prentice-Hall, 1968, pp. 68–86.
Siegel S . Nonparametric Statistics for the Behavioral Sciences. New York: MacGraw-Hill, 1956, pp. 184–194.
Winer BJ . Statistical Principles in Experimental Design. London: MacGraw-Hill, 1970, pp. 46–104.
Mantel N . Chi square test with one degree of freedom: extensions of the Mantel-Haenszel procedure. J Am Stat Assoc 1963; 58: 690–700.
Cohen J . Statistical Power Analysis for the Behavioral Sciences. New York: Academic Press, 1978.
Katz JN, Larson MG, Phillips CB, Fossel AH, Liang MH . Comparative measurement sensitivity of short and longer health status instruments. Med Care 1992; 30: 917–925.
Kolotkin RL, Crosby RD, Williams GR . Health-related quality of life varies among obese subgroups. Obes Res 2002; 10: 748–756.
Engel SG, Crosby RD, Kolotkin RL, Hartley GG, Williams GR, Wonderlich SA et al. Impact of weight loss and regain on quality of life: mirror image or differential effect? Obes Res 2003; 11: 1207–1213.
Ware Jr JE, Snow KK, Kosinski M, Gandek B . SF-36 Health Survey Manual and Interpretation Guide. Boston: New England Medical Center: The Health Institute, 1993.
Persson L-O, Karlsson J, Bengtsson C, Steen B, Sullivan M . The Swedish SF-36 Health Survey. II. Evaluation of clinical validity: Results from population studies of elderly and women in Gothenburg. J Clin Epidemiol 1998; 51: 1095–1103.
Björner JB, Sondergaard Kristensen T, Orth-Gomér K, Tibblin G, Sullivan M, Westerholm P . Self-Rated Health – A Useful Concept in Research, Prevention and Clinical Medicine. Swedish council for planning and coordination of research, Report 96:9 Spri: Stockholm 1996.
Näslund I . Lessons from the Swedish Obese Subjects study: the effects of surgically induced weight loss on obesity comorbidity. Surg Obes Relat Dis 2005; 1: 140–144.
National Health Lung Blood Institute. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. Obes Res 1998; 6: 51S–210S.
Kaukua J, Pekkarinen T, Sane T, Mustajoki P . Health-related quality of life in obese outpatients losing weight with very-low-energy diet and behaviour modification – a 2-y follow-up study. Int J Obes Rebat Metls Disord 2003; 27: 1233–1241.
Fabricatore AN, Wadden TA . Psychological aspects of obesity. Clin Dermatol 2004; 22: 332–337.
Herva A, Laitinen J, Miettunen J, Veijola J, Karvonen JT, Laksy K, Joukamaa M . Obesity and depression: results from the longitudinal Northern Finland 1966 Birth Cohort Study. Int J Obes Relat Metab Disord 2006; 30: 520–527.
Dixon JB, Dixon ME, O'Brien PE . Depression in association with severe obesity: changes with weight loss. Arch Intern Med 2003; 163: 2058–2065.
Velcu LM, Adolphine R, Mourelo R, Cottam DR, Angus LDG . Weight loss, quality of life and employment status after Roux-en-Y gastric bypass: 5-year analysis. Surg Obes Relat Dis 2005; 1: 413–417.
Arnold PD, Zai G, Richter MA . Genetics of anxiety disorders. Curr Psychiatry Rep 2004; 6: 243–254.
Gordon JA, Hen R . Genetic approaches to the study of anxiety. Annu Rev Neurosci 2004; 27: 193–222.
Brolin RL, Robertson LB, Kenler HA, Cody RP . Weight loss and dietary intake after vertical banded gastroplasty and Roux-en-Y gastric bypass. Ann Surg 1994; 220: 782–790.
Hernandez-Estefania R, Gonzalez-Lamuno D, Garcia-Ribes M, Garcia-Fuentes M, Cagigas JC, Ingelmo A, Escalante C . Variables affecting BMI evolution at 2 and 5 years after vertical banded gastroplasty. Obes Surg 2000; 10: 160–166.
Wadden TA, Butryn ML, Byrne KJ . Efficacy of lifestyle modification for long-term weight control. Obes Res 2004; 12: 151S–162S.
Jakicic JM, Otto AD . Physical activity considerations for the treatment and prevention of obesity. Am J Clin Nutr 2005; 82: 226S–229S.
Wing R, Phelan S . Long-term weight loss maintenance. Am J Clin Nutr 2005; 82: 222S–225S.
Klem ML, Wing RR, Chang CC, Lang W, McGuire MT, Sugerman HJ et al. A case-control study of successful maintenance of a substantial weight loss: individuals who lost weight through surgery versus those who lost weight through nonsurgical means. Int J Obes Relat Metab Disord 2000; 24: 573–579.
Warburton DE, Nicol CW, Bredin SS . Health benefits of physical activity: the evidence. Can Med Assoc J 2006; 174: 801–809.
Bensimhon DR, Kraus WE, Donahue MP . Obesity and physical activity: a review. Am Heart J 2006; 151: 598–603.
Hsu LK, Betancourt S, Sullivan SP . Eating disturbances before and after vertical banded gastroplasty: a pilot study. Int J Eat Disord 1996; 19: 23–34.
Kalarchian MA, Marcus MD, Wilson GT, Labouvie EW, Brolin RE, LaMarca LB . Binge eating among gastric bypass patients at long-term follow-up. Obes Surg 2002; 12: 270–275.
Kinzl JF, Trefalt E, Fiala M, Biebl W . Psychotherapeutic treatment of morbidly obese patients after gastric banding. Obes Surg 2002; 12: 292–294.
Ryden A, Karlsson J, Sullivan M, Torgerson JS, Taft C . Coping and distress: what happens after intervention? A 2-year follow-up from the Swedish Obese Subjects (SOS) study. Psychosom Med 2003; 65: 435–442.
Nicolai A, Ippoliti C, Petrelli MD . Laparoscopic adjustable gastric banding: essential role of psychological support. Obes Surg 2002; 12: 857–863.
Acknowledgements
This project has been supported by the Swedish Council for Working Life and Social Research (project 97–0355:1B and 2B; F0140/2000; 2001–1106; 2002–0109), the Swedish Foundation for Health Care Sciences and Allergy Research (project V96–065; V99–046; V2002–172(F)), the Swedish Research Council/Medicine (project K2003–27VX-14685–01A) and the Sahlgrenska Academy at Göteborg University (project ALFGBG-2780), Göteborg.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Karlsson, J., Taft, C., Rydén, A. et al. Ten-year trends in health-related quality of life after surgical and conventional treatment for severe obesity: the SOS intervention study. Int J Obes 31, 1248–1261 (2007). https://doi.org/10.1038/sj.ijo.0803573
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0803573
Keywords
This article is cited by
-
A Randomized Controlled Trial Investigating the Impact of a Low-Calorie Dietary Approach to Stop Hypertension (DASH) on Anthropometric and Glycemic Measures in Patients Experiencing Weight Regain 2 Years Post Sleeve Surgery
Obesity Surgery (2024)
-
Endoscopic Management of Gastric Band Erosion: a Systematic Review and Meta-Analysis
Obesity Surgery (2024)
-
Brain functional and structural magnetic resonance imaging of obesity and weight loss interventions
Molecular Psychiatry (2023)
-
Bariatric Surgery and Psychological Health: A Randomised Clinical Trial in Patients with Obesity and Type 2 Diabetes
Obesity Surgery (2023)
-
Mental health status as a predictor of emergency department visits and hospital readmissions post bariatric surgery: a retrospective cohort study
Surgical Endoscopy (2023)