Abstract
Objective:
To identify the proportion of weight lost as fat-free mass (FFM) by various weight loss interventions.
Methods:
Medline and Embase were systematically searched for reliable measurements of FFM before and after weight loss of >10 kg and eligible data were pooled. In a fixed effect model of % FFM loss/weight loss (%FFML), linear regression analysis was used to determine the influence of degree of caloric restriction, exercise, magnitude of weight loss, initial body mass index (BMI) and type of surgery.
Results:
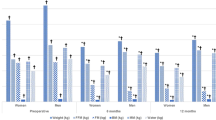
Data were included from 26 cohorts treated with dietary and behavioral interventions and 29 cohorts of bariatric surgery patients. The degree of caloric restriction was positively associated with %FFML (r2=0.31, P=0.006) and in three randomized controlled trials exercise was shown to decrease %FFML. Compared with laparoscopic adjustable gastric banding (LAGB), biliopancreatic diversion (BPD) and roux en Y gastric bypass (RYGB) caused greater loge (natural log) %FFML (r2=0.453, P<0.001). Differences in loge %FFML between surgical procedures were independent of initial BMI and magnitude of weight loss.
Conclusions:
The degree of caloric restriction, exercise and rate of weight loss influence the proportion of weight lost as FFM after non-surgical interventions. For surgical interventions, BPD and RYGB result in greater %FFML than LAGB.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Campbell I . The obesity epidemic: can we turn the tide? Heart 2003; 89 (Suppl 2): ii22–ii24.
Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM . Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. JAMA 2004; 291: 2847–2850.
Proietto J, Baur LA . 10: Management of obesity. Med J Aust 2004; 180: 474–480.
Marks BL, Rippe JM . The importance of fat free mass maintenance in weight loss programmes. Sports Med 1996; 22: 273–281.
Webster JD, Hesp R, Garrow JS . The composition of excess weight in obese women estimated by body density, total body water and total body potassium. Hum Nutr Clin Nutr 1984; 38: 299–306.
Fernandez JR, Heo M, Heymsfield SB, Pierson Jr RN, Pi-Sunyer FX, Wang ZM et al. Is percentage body fat differentially related to body mass index in Hispanic Americans, African Americans, and European Americans? Am J Clin Nutr 2003; 77: 71–75.
Gallagher D, Heymsfield SB, Heo M, Jebb SA, Murgatroyd PR, Sakamoto Y . Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr 2000; 72: 694–701.
Katz DL . Competing dietary claims for weight loss: finding the forest through truculent trees. Annu Rev Public Health 2005; 26: 61–88.
Abdel-Hamid TK . Exercise and diet in obesity treatment: an integrative system dynamics perspective. Med Sci Sports Exerc 2003; 35: 400–413.
Kojima M, Hosoda H, Date Y, Nakazato M, Matsuo H, Kangawa K . Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature 1999; 402: 656–660.
Fruhbeck G, Diez Caballero A, Gil MJ . Fundus functionality and ghrelin concentrations after bariatric surgery. N Engl J Med 2004; 350: 308–309.
Haarbo J, Gotfredsen A, Hassager C, Christiansen C . Validation of body composition by dual energy X-ray absorptiometry (DEXA). Clin Physiol 1991; 11: 331–341.
Pritchard JE, Nowson CA, Strauss BJ, Carlson JS, Kaymakci B, Wark JD . Evaluation of dual energy X-ray absorptiometry as a method of measurement of body fat. Eur J Clin Nutr 1993; 47: 216–228.
Salamone LM, Fuerst T, Visser M, Kern M, Lang T, Dockrell M et al. Measurement of fat mass using DEXA: a validation study in elderly adults. J Appl Physiol 2000; 89: 345–352.
Aloia JF, Vaswani A, Ma R, Flaster E . Comparative study of body composition by dual-energy x-ray absorptiometry. J Nucl Med 1995; 36: 1392–1397.
Bosy-Westphal A, Mast M, Eichhorn C, Becker C, Kutzner D, Heller M et al. Validation of air-displacement plethysmography for estimation of body fat mass in healthy elderly subjects. Eur J Nutr 2003; 42: 207–216.
Lukaski HC, Johnson PE, Bolonchuk WW, Lykken GI . Assessment of fat-free mass using bioelectrical impedance measurements of the human body. Am J Clin Nutr 1985; 41: 810–817.
Cox-Reijven PL, van Kreel B, Soeters PB . Accuracy of bioelectrical impedance spectroscopy in measuring changes in body composition during severe weight loss (comment). J Parenteral Enteral Nutr 2002; 26: 120–127.
Larsson I, Lindroos AK, Peltonen M, Sjostrom L . Potassium per kilogram fat-free mass and total body potassium: predictions from sex, age, and anthropometry. Am J Physiol Endocrinol Metab 2003; 284: E416–E423.
Ross R, Rissanen J, Pedwell H, Clifford J, Shragge P . Influence of diet and exercise on skeletal muscle and visceral adipose tissue in men. J Appl Physiol 1996; 81: 2445–2455.
Mitsiopoulos N, Baumgartner RN, Heymsfield SB, Lyons W, Gallagher D, Ross R . Cadaver validation of skeletal muscle measurement by magnetic resonance imaging and computerized tomography. J Appl Physiol 1998; 85: 115–122.
Pickering TG, Gerin W . Ambulatory blood pressure monitoring and cardiovascular reactivity testing for the evaluation of the role of psychosocial factors and prognosis in hypertensive patients. Am Heart J 1988; 116: 665–672.
Due A, Toubro S, Skov AR, Astrup A . Effect of normal-fat diets, either medium or high in protein, on body weight in overweight subjects: a randomised 1-year trial. Int J Obes Relat Metab Disord 2004; 28: 1283–1290.
Leenen R, van der Kooy K, Droop A, Seidell JC, Deurenberg P, Weststrate JA et al. Visceral fat loss measured by magnetic resonance imaging in relation to changes in serum lipid levels of obese men and women. Arterioscler Thromb 1993; 13: 487–494.
Gotfredsen A, Westergren Hendel H, Andersen T . Influence of orlistat on bone turnover and body composition. Int J Obes Relat Metab Disord 2001; 25: 1154–1160.
Gower BA, Weinsier RL, Jordan JM, Hunter GR, Desmond R . Effects of weight loss on changes in insulin sensitivity and lipid concentrations in premenopausal African American and white women. Am J Clin Nutr 2002; 76: 923–927.
Kockx M, Leenen R, Seidell J, Princen HM, Kooistra T . Relationship between visceral fat and PAI-1 in overweight men and women before and after weight loss. Thromb Haemost 1999; 82: 1490–1496.
Tchernof A, Nolan A, Sites CK, Ades PA, Poehlman ET . Weight loss reduces C-reactive protein levels in obese postmenopausal women. Circulation 2002; 105: 564–569.
Purnell JQ, Kahn SE, Albers JJ, Nevin DN, Brunzell JD, Schwartz RS . Effect of weight loss with reduction of intra-abdominal fat on lipid metabolism in older men. J Clin Endocrinol Metab 2000; 85: 977–982.
Tchernof A, Starling RD, Turner A, Shuldiner AR, Walston JD, Silver K et al. Impaired capacity to lose visceral adipose tissue during weight reduction in obese postmenopausal women with the Trp64Arg beta3-adrenoceptor gene variant. Diabetes 2000; 49: 1709–1713.
Shadid S, Jensen MD . Effects of pioglitazone versus diet and exercise on metabolic health and fat distribution in upper body obesity. Diabetes Care 2003; 26: 3148–3152.
Okura T, Nakata Y, Tanaka K . Effects of exercise intensity on physical fitness and risk factors for coronary heart disease. Obes Res 2003; 11: 1131–1139.
Kamel EG, McNeill G, Van Wijk MC . Change in intra-abdominal adipose tissue volume during weight loss in obese men and women: correlation between magnetic resonance imaging and anthropometric measurements. Int J Obes Relat Metab Disord 2000; 24: 607–613.
Berube-Parent S, Prud'homme D, St-Pierre S, Doucet E, Tremblay A . Obesity treatment with a progressive clinical tri-therapy combining sibutramine and a supervised diet – exercise intervention. Int J Obes Relat Metab Disord 2001; 25: 1144–1153.
Pronk NP, Donnelly JE, Pronk SJ . Strength changes induced by extreme dieting and exercise in severely obese females. J Am Coll Nutr 1992; 11: 152–158.
Hoie LH, Bruusgaard D, Thom E . Reduction of body mass and change in body composition on a very low calorie diet. Int J Obes Relat Metab Disord 1993; 17: 17–20.
Eston RG, Shephard S, Kreitzman S, Coxon A, Brodie DA, Lamb KL et al. Effect of very low calorie diet on body composition and exercise response in sedentary women. Eur J Appl Physiol Occup Physiol 1992; 65: 452–458.
Goodpaster BH, Kelley DE, Wing RR, Meier A, Thaete FL . Effects of weight loss on regional fat distribution and insulin sensitivity in obesity. Diabetes 1999; 48: 839–847.
Janssen I, Fortier A, Hudson R, Ross R . Effects of an energy-restrictive diet with or without exercise on abdominal fat, intermuscular fat, and metabolic risk factors in obese women. Diabetes Care 2002; 25: 431–438.
Janssen I, Ross R . Effects of sex on the change in visceral, subcutaneous adipose tissue and skeletal muscle in response to weight loss. Int J Obes Relat Metab Disord 1999; 23: 1035–1046.
Rice B, Janssen I, Hudson R, Ross R . Effects of aerobic or resistance exercise and/or diet on glucose tolerance and plasma insulin levels in obese men. Diabetes Care 1999; 22: 684–691.
Vettor R, Mingrone G, Manco M, Granzotto M, Milan G, Scarda A et al. Reduced expression of uncoupling proteins-2 and -3 in adipose tissue in post-obese patients submitted to biliopancreatic diversion. Eur J Endocrinol 2003; 148: 543–550.
Tacchino RM, Mancini A, Perrelli M, Bianchi A, Giampietro A, Milardi D et al. Body composition and energy expenditure: relationship and changes in obese subjects before and after biliopancreatic diversion. Metabolism 2003; 52: 552–558.
Gniuli D, Rosa G, Manco M, Scarfone A, Vega N, Greco AV et al. Changes in fat mass influence SREBP-1c and UCP-2 gene expression in formerly obese subjects. Obes Res 2005; 13: 567–573.
Mingrone G, Greco AV, Giancaterini A, Scarfone A, Castagneto M, Pugeat M . Sex hormone-binding globulin levels and cardiovascular risk factors in morbidly obese subjects before and after weight reduction induced by diet or malabsorptive surgery. Atherosclerosis 2002; 161: 455–462.
Fabris R, Mingrone G, Milan G, Manco M, Granzotto M, Dalla Pozza A et al. Further lowering of muscle lipid oxidative capacity in obese subjects after biliopancreatic diversion. J Clin Endocrinol Metab 2004; 89: 1753–1759.
Valera-Mora ME, Simeoni B, Gagliardi L, Scarfone A, Nanni G, Castagneto M et al. Predictors of weight loss and reversal of comorbidities in malabsorptive bariatric surgery. Am J Clin Nutr 2005; 81: 1292–1297.
Benedetti G, Mingrone G, Marcoccia S, Benedetti M, Giancaterini A, Greco AV et al. Body composition and energy expenditure after weight loss following bariatric surgery. J Am Coll Nutr 2000; 19: 270–274.
Greco AV, Mingrone G, Giancaterini A, Manco M, Morroni M, Cinti S et al. Insulin resistance in morbid obesity: reversal with intramyocellular fat depletion. Diabetes 2002; 51: 144–151.
Das SK, Roberts SB, McCrory MA, Hsu LK, Shikora SA, Kehayias JJ et al. Long-term changes in energy expenditure and body composition after massive weight loss induced by gastric bypass surgery. Am J Clin Nutr 2003; 78: 22–30.
Carey DG, Pliego GJ, Raymond RL, Skau KB . Body composition and metabolic changes following bariatric surgery: effects on fat mass, lean mass and basal metabolic rate. Obes Surg 2006; 16: 469–477.
Coupaye M, Bouillot JL, Coussieu C, Guy-Grand B, Basdevant A, Oppert JM . One-year changes in energy expenditure and serum leptin following adjustable gastric banding in obese women. Obes Surg 2005; 15: 827–833.
Pugnale N, Giusti V, Suter M, Zysset E, Heraief E, Gaillard RC et al. Bone metabolism and risk of secondary hyperparathyroidism 12 months after gastric banding in obese pre-menopausal women. Int J Obes Relat Metab Disord 2003; 27: 110–116.
Sergi G, Lupoli L, Busetto L, Volpato S, Coin A, Bertani R et al. Changes in fluid compartments and body composition in obese women after weight loss induced by gastric banding. Ann Nutr Metab 2003; 47: 152–157.
Gasteyger C, Suter M, Calmes JM, Gaillard RC, Giusti V . Changes in body composition, metabolic profile and nutritional status 24 months after gastric banding. Obes Surg 2006; 16: 243–250.
Giusti V, Gasteyger C, Suter M, Heraief E, Gaillard RC, Burckhardt P . Gastric banding induces negative bone remodelling in the absence of secondary hyperparathyroidism: potential role of serum C telopeptides for follow-up. Int J Obes 2005; 29: 1429–1435.
Giusti V, Suter M, Heraief E, Gaillard RC, Burckhardt P . Effects of laparoscopic gastric banding on body composition, metabolic profile and nutritional status of obese women: 12-months follow-up. Obes Surg 2004; 14: 239–245.
Garrapa GGM, Canibus P, Gatti C, Santangelo M, Frezza F, Feliciotti F et al. Changes in body composition and insulin sensitivity in severely obese subjects after laparoscopic adjustable silicone gastric banding (LASGB). Med Sci Monitor 2005; 11: CR522–CR528.
Forbes GB . Body fat content influences the body composition response to nutrition and exercise. Ann N Y Acad Sci 2000; 904: 359–365.
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K et al. Bariatric surgery: a systematic review and meta-analysis. Jama 2004; 292: 1724–1737.
Shuster MH, Vazquez JA . Nutritional concerns related to Roux-en-Y gastric bypass: what every clinician needs to know. Crit Care Nurs Q 2005; 28: 227–260.
Fruhbeck G, Diez-Caballero A, Gil MJ, Montero I, Gomez-Ambrosi J, Salvador J et al. The decrease in plasma ghrelin concentrations following bariatric surgery depends on the functional integrity of the fundus. Obes Surg 2004; 14: 606–612.
Langer FB, Reza Hoda MA, Bohdjalian A, Felberbauer FX, Zacherl J, Wenzl E et al. Sleeve gastrectomy and gastric banding: effects on plasma ghrelin levels. Obes Surg 2005; 15: 1024–1029.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chaston, T., Dixon, J. & O'Brien, P. Changes in fat-free mass during significant weight loss: a systematic review. Int J Obes 31, 743–750 (2007). https://doi.org/10.1038/sj.ijo.0803483
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0803483
Keywords
This article is cited by
-
The impact of leucine supplementation on body composition and glucose tolerance following energy restriction: an 8-week RCT in adults at risk of the metabolic syndrome
European Journal of Clinical Nutrition (2024)
-
Body Composition Changes in Adolescents Who Underwent Bariatric Surgery: A Systematic Review and Meta-analysis
Current Obesity Reports (2024)
-
Are methods of estimating fat-free mass loss with energy-restricted diets accurate?
European Journal of Clinical Nutrition (2023)
-
Associations of changes in physical activity and sedentary time with weight recurrence after bariatric surgery: a 5-year prospective study
International Journal of Obesity (2023)
-
Impact of Preoperative Protein Sparing Modified Fast Diet on Bariatric Surgery
Obesity Surgery (2023)