Abstract
Background:
Obesity, inflammation, insulin resistance and cardiovascular disease (CVD) risk are inter-related. Both weight-loss and long-chain n-3 polyunsaturated fatty acids (LC n-3 PUFA) are independently known to reduce metabolic risk, but the combined effects are unclear.
Objective:
This study examines whether addition of LC n-3 PUFA to a low fat/high carbohydrate weight-loss programme results in greater improvements in inflammation, insulin sensitivity and CVD risk, than weight-loss alone.
Design:
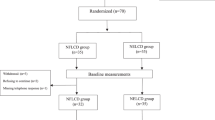
One hundred and sixteen overweight insulin-resistant women entered a 24-week randomised intervention study. Thirty-nine women were randomised to a weight-loss programme, with LC n-3 PUFA (WLFO), 38 to a weight-loss programme with placebo oil (WLPO), and 39 to receive placebo oil, with no weight-loss programme (control).
Results:
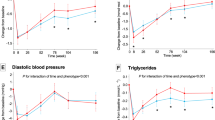
Ninety-three women completed the study (35 WLFO, 32 WLPO and 26 control), with significant weight-loss in WLFO (10.8±1.0%) and WLPO (12.4±1.0%) compared to the control group (P<0.0001). The WLFO, but not WLPO or control group, showed significant increases in adipose tissue LC n-3 PUFA (0.34±0.20 vs 0.17±0.10 and 0.16±0.10 %DHA, P<0.0001). Weight-loss showed significant improvements in insulin sensitivity (P<0.001), lipid profile (triglycerides P<0.05) and inflammation (sialic acid P<0.05). Time*group effects showed significant decreases in triglycerides (P<0.05) and increases in adiponectin (P<0.01) with LC n-3 PUFA, in the WLFO vs WLPO groups.
Conclusions:
Weight-loss improved risk factors associated with CVD, with some additional benefits of LC n-3 PUFA on triglycerides and adiponectin. Given the current low dietary intake of LC n-3 PUFA, greater attention should be given to increase these fatty acids in the treatment of obesity.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Manson JE, Willett WC, Stampfer MJ, Colditz GA, Hunter DJ, Hankinson SE et al. Body weight and mortality among women. N Engl J Med 1995; 333: 677–685.
WHO Division of Noncommunicable Diseases/World Health Organisation/Programme of Nutrition Family and Reproductive Health. Obesity – preventing and managing the global epidemic. Report of a WHO Consultation on Obesity. World Health Organisation: Geneva (WHO/NUT/NCD/98.1.), 1998.
Chan JM, Rimm EB, Colditz GA, Stampfer MJ, Willett WC . Obesity, fat distribution, and weight gain as risk factors for clinical diabetes in men. Diab Care 1994; 17: 961–969.
Colditz GA, Willett WC, Stampfer MJ, Manson JE, Hennekens CH, Arky RA et al. Weight as a risk factor for clinical diabetes in women. Am J Epidemiol 1990; 132: 501–513.
Manson JE, Colditz GA, Stampfer MJ, Willett WC, Rosner B, Monson RR et al. A prospective study of obesity and risk of coronary heart disease in women. N Engl J Med 1990; 322: 882–889.
Stamler R, Stamler J, Riedlinger WF, Algera G, Roberts RH . Weight and blood pressure. Findings in hypertension screening of 1 million Americans. JAMA 1978; 240: 1607–1610.
Krebs JD, Evans S, Cooney L, Mishra GD, Fruhbeck G, Finer N et al. Changes in risk factors for cardiovascular disease with body fat loss in obese women. Diab Obes Metab 2002; 4: 379–387.
Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002; 346: 393–403.
Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P et al. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 2001; 344: 1343–1350.
Visser M, Bouter LM, McQuillan GM, Wener MH, Harris TB . Elevated C-reactive protein levels in overweight and obese adults. JAMA 1999; 282: 2131–2135.
Pannacciulli N, Cantatore F, Minenna A, Bellacicco M, Giorgino R, De Pergola G . C-reactive protein is independently associated with total body fat, central fat, and insulin resistance in adult women. Int J Obes Relate Metab Disord 2001; 25: 1416–1420.
Festa A, D'Agostino Jr R, Williams K, Karter AJ, Mayer-Davis EJ, Tracy RP et al. The relation of body fat mass and distribution to markers of chronic inflammation. Int J Obes Relat Metab Disord 2001; 25: 1407–1415.
Festa A, D'Agostino Jr R, Howard G, Mykkanen L, Tracy RP, Haffner SM . Chronic subclinical inflammation as part of the insulin resistance syndrome: the Insulin Resistance Atherosclerosis Study (IRAS). Circulation 2000; 102: 42–47.
Browning LM, Jebb SA, Mishra GD, Cooke JH, O'Connell MA, Crook MA et al. Elevated sialic acid, but not CRP, predicts features of the metabolic syndrome independently of BMI in women. Int J Obes 2004; 28: 1004–1010.
Yudkin JS, Stehouwer CDA, Emeis JJ, Coppack SW . C-reactive protein in healthy subjects: associations with obesity, insulin resistance, and endothelial dysfunction. A potential role for cytokines originating from adipose tissue? Arterioscler Thromb Vasc Biol 1999; 19: 972–978.
Ridker PM, Hennekens CH, Burling JE, Rifai N . C-Reactive protein and other markers of inflammation in the prediciton of cardiovascular disease in women. N Engl J Med 2000; 342: 836–843.
Ridker PM, Stampfer MJ, Rifai N . Novel risk factors for systemic atherosclerosis: a comparison of C-reactive protein, fibrinogen, homocysteine, lipoprotein(a), and standard cholesterol screening as predictors of peripheral arterial disease. JAMA 2001; 285: 2481–2485.
Schmidt MI, Duncan BB, Sharrett AR, Lindberg G, Savage PJ, Offenbacher S et al. Markers of inflammation and prediction of diabetes mellitus in adults (Atherosclerosis Risk in Communities study): a cohort study. Lancet 1999; 353: 1649–1652.
Duncan BB, Schmidt MI, Pankow JS, Ballantyne CM, Couper D, Vigo A et al. Low-grade systemic inflammation and the development of type 2 diabetes: the atherosclerosis risk in communities study. Diabetes 2003; 52: 1799–1805.
Harris WS . n-3 fatty acids and lipoproteins: comparison of results from human and animal studies. Lipids 1996; 31: 243–252.
Roche HM, Gibney MJ . Postprandial triacylglycerolaemia: the effect of low-fat dietary treatment with and without fish oil supplementation. Eur J Clin Nutr 1996; 50: 617–624.
Kriketos AD, Robertson RM, Sharp TA, Drougas H, Reed GW, Storlien LH et al. Role of weight loss and polyunsaturated fatty acids in improving metabolic fitness in moderately obese, moderately hypertensive subjects. J Hypertens 2001; 19: 1745–1754.
James MJ, Gibson RA, Cleland LG . Dietary polyunsaturated fatty acids and inflammatory mediator production. Am J Clin Nutr 2000; 71: 343S–348S.
Chambrier C, Bastard JP, Rieusset J, Chevillotte E, Bonnefont-Rousselot D, Therond P et al. Eicosapentaenoic acid induces mRNA expression of peroxisome proliferator-activated receptor gamma. Obes Res 2002; 10: 518–525.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC . Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 1985; 28: 412–419.
Friedewald WT, Levy RI, Frederickson DS . Estimation of the concentration of low-density lipoprotein cholesterol in plasma without the use of the preparative ultracentrifuge. Clin Chem 1972; 18: 499–502.
Bastard JP, Cuevas J, Cohen S, Jardel C, Hainque B . Percutaneous adipose tissue biopsy by mini-liposuction for metabolic studies. Jpen: J Parenteral Enteral Nutr 1994; 18: 466–468.
Folch J, Lees M, Sloane-Stanley GH . A simple method for the isolation and purification of total lipids from animal tissues. J Biol Chem 1957; 226: 497–509.
Katan MB, Grundy SM, Willett WC . Should a low-fat, high-carbohydrate diet be recommended for everyone? Beyond low-fat diets. N Engl J Med 1997; 337: 563–566.
Katan MB . Effect of low-fat diets on plasma high-density lipoprotein concentrations. Am J Clin Nutr 1998; 67: 573S–576S.
Hainault I, Carolotti M, Hajduch E, Guichard C, Lavau M . Fish oil in a high lard diet prevents obesity, hyperlipemia, and adipocyte insulin resistance in rats. Ann NY Acad Sci 1993; 683: 98–101.
Sprecher H, Chen Q, Yin FQ . Regulation of the biosynthesis of 22:5n-6 and 22:6n-3: a complex intracellular process. Lipids 1999; 34 (Suppl): S153–S156.
Storlien LH, Kraegen EW, Chisholm DJ, Ford GL, Bruce DG, Pascoe WS . Fish oil prevents insulin resistance induced by high-fat feeding in rats. Science 1987; 237: 885–888.
Clarke SD . Polyunsaturated fatty acid regulation of gene transcription: a mechanism to improve energy balance and insulin resistance. Br J Nutr 2000; 83: S59–S66.
Mori TA, Burke V, Puddey IB, Watts GF, O'Neal DN, Best JD, Beilin LJ . Purified eicosapentaenoic and docosahexaenoic acids have differential effects on serum lipids and lipoproteins, LDL particle size, glucose, and insulin in mildly hyperlipidemic men (In Process Citation). Am J Clin Nutr 2000; 71: 1085–1094.
Friedberg CE, Janssen MJ, Heine RJ, Grobbee DE . Fish oil and glycemic control in diabetes. A meta-analysis. Diabet Care 1998; 21: 494–500.
Borkman M, Chisholm DJ, Furler SM, Storlien LH, Kraegen EW, Simons LA, Chesterman CN . Effects of Fish Oil Supplementation on Glucose and Lipid Metabolism in NIDDM. Diabetes 1989; 38: 1314–1319.
Mori TA . Purified eicosapentaenoic and docosahexaenoic acids have differential effects on serum lipids and lipoproteins, LDL particle size, glucose, and insulin in midly hyperlipidemic men. Am J Clin Nutr 2000; 71: 1085–1094.
Friedberg CE, Heine RJ, Janssen MJFM, Grobbee DE . Fish oil and glycaemic control in diabetes. A meta-analysis. Diabet Care 1998; 21: 494–500.
Borkman M, Chisholm DJ, Furler SM, Storlien LH, Kraegen EW, Simons LA, Chesterman CN . Effects of fish oil supplementation on glucose and lipid metabolism in NIDDM. Diabetes 1989; 38: 1314–1319.
Grundt H, Nilsen DW, Hetland O, Aarsland T, Baksaas I, Grande T et al. Improvement of serum lipids and blood pressure during intervention with n-3 fatty acids was not associated with changes in insulin levels in subjects with combined hyperlipidaemia. J Intern Med 1995; 237: 249–259.
Toft I, Bonaa KH, Ingebretsen OC, Nordoy A, Jenssen T . Effects of n-3 polyunsaturated fatty acids on glucose homeostasis and blood pressure in essential hypertension. A randomized, controlled trial. Ann Intern Med 1995; 123: 911–918.
Mori TA, Bao DQ, Burke V, Puddey IB, Watts GF, Beilin LJ . Dietary fish as a major component of a weight-loss diet: effect on serum lipids, glucose, and insulin metabolism in overweight hypertensive subjects. Am J Clin Nutr 1999; 70: 817–825.
Vessby B, Unsitupa M, Hermansen K, Riccardi G, Rivellese AA, Tapsell LC et al. Substituting dietary saturated for monounsaturated fat impairs insulin sensitivity in healthy men and women: The KANWU Study. Diabetologia 2001; 44: 312–319.
Browning LM, Krebs JD, Moore CM, Mishra GD, O'Connell MA, Jebb SA . The impact of long chain n-3 polyunsaturated fatty acid supplementation on inflammation, insulin sensitivity and CVD risk in a group of overweight women with an inflammatory phenotype. Diabet Obes Metabol 2005. (in press).
Bao DQ, Mori TA, Burke V, Puddey IB, Beilin LJ . Effects of dietary fish and weight reduction on ambulatory blood pressure in overweight hypertensives. Hypertension 1998; 32: 710–717.
Yang WS, Lee WJ, Funahashi T, Tanaka S, Matsuzawa Y, Chao CL et al. Weight reduction increases plasma levels of an adipose-derived anti-inflammatory protein, adiponectin. J Clin Endocrinol Metabol 2001; 86: 3815–3819.
Dandona P, Weinstock R, Thusu K, Abdel-Rahman E, Aljada A, Wadden T . Tumor necrosis factor-alpha in sera of obese patients: fall with weight loss. J Clin Endocrinol Metabol 1998; 83: 2907–2910.
Bastard JP, Hainque B, Dusserre E, Bruckert E, Robin D, Vallier P et al. Peroxisome proliferator activated receptor-gamma, leptin and tumor necrosis factor-alpha mRNA expression during very low calorie diet in subcutaneous adipose tissue in obese women. Diabet/Metabol Res Rev 1999; 15: 92–98.
Kern PA, Saghizadeh M, Ong JM, Bosch RJ, Deem R, Simsolo RB . The expression of tumor necrosis factor in human adipose tissue. Regulation by obesity, weight loss, and relationship to lipoprotein lipase. J Clin Investigat 1995; 95: 2111–2119.
Bastard J-P, Jardel C, Bruckert E, Blondy P, Capeau J, Laville M et al. Elevated levels of interleukin-6 are reduced in serum and subcutaneous adipose tissue of obese women after weight loss. J Clin Endocrinol Metabol 2000; 85: 3338–3342.
Calder PC . n-3 Polyunsaturated fatty acids and cytokine production in health and disease. Ann Nutr Metabol 1997; 41: 203–234.
Acknowledgements
This study was funded by the Medical Research Council. None of the authors had any conflicts of interest. We thank Ms J Cooke, HNR volunteer suite staff and Dieticians at Addenbrooke's Hospital for the volunteer work, Mr N Matthews for the fatty acid analysis, Mr I Halsall for the insulin analysis, Mr C Charalambos and the Nutritional Biochemistry Laboratory for other biochemical analyses. We also thank Pronova (Norway) for supplying the capsules for the intervention and SMILES for funding the development of the dietary advice programme.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions: JD Krebs was responsible for all aspects of the study design, data collection, analysis and writing the manuscript. SA Jebb was involved in study design, data analysis and writing the manuscript. LM Browning was involved in data collection, data analysis and writing the manuscript. N McLean was involved in the developing the weight-loss programme and reviewing the manuscript. JL Rothwell, CS Moore and GD Mishra were involved in data collection, analysis and reviewing the manuscript.
Supplementary information is available on the International Journal of Obesity website (http://www.nature.com/ijo)
Supplementary information
Rights and permissions
About this article
Cite this article
Krebs, J., Browning, L., McLean, N. et al. Additive benefits of long-chain n-3 polyunsaturated fatty acids and weight-loss in the management of cardiovascular disease risk in overweight hyperinsulinaemic women. Int J Obes 30, 1535–1544 (2006). https://doi.org/10.1038/sj.ijo.0803309
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0803309
Keywords
This article is cited by
-
The effects of canola and olive oils consumption compared to sunflower oil, on lipid profile and hepatic steatosis in women with polycystic ovarian syndrome: a randomized controlled trial
Lipids in Health and Disease (2021)
-
Long-term effects of increasing omega-3, omega-6 and total polyunsaturated fats on inflammatory bowel disease and markers of inflammation: a systematic review and meta-analysis of randomized controlled trials
European Journal of Nutrition (2021)
-
Omega-3 fatty acids as feed supplement modulates blood formation and body weight in Rattus norvegicus model
The Journal of Basic and Applied Zoology (2020)
-
High-dose omega-3 polyunsaturated fatty acid supplementation might be more superior than low-dose for major depressive disorder in early therapy period: a network meta-analysis
BMC Psychiatry (2020)
-
Higher erythrocyte n-3 polyunsaturated fatty acid were associated with a better profile of DXA-derived body fat and fat distribution in adults
International Journal of Obesity (2020)