Abstract
Objective:
To investigate whether leukocyte count, fibrinogen, von Willebrand factor (vWF) and plasminogen activator inhibitor-1 activity (PAI-1) are increased in subjects with the metabolic syndrome as defined by the National Cholesterol Education Program-Adult Treatment Panel III (NCEP-ATPIII) and the World Health Organisation (WHO).
Design:
Cross-sectional study.
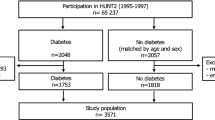
Subjects:
A total of 520 overweight and obese subjects: 379 women and 141 men, visiting the weight management clinic of a University Hospital.
Subjects and measurements:
Waist circumference, triglycerides, HDL cholesterol, blood pressure and fasting glucose were determined, and the presence or absence of the metabolic syndrome according to the NCEP-ATPIII criteria was assessed. In 349 subjects, data on the waist-to-hip ratio (WHR) and albumin excretion rate were available and the WHO criteria were applied. Insulin resistance was defined using the HOMA-IR index.
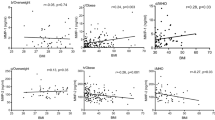
Results:
Subjects with the metabolic syndrome according to the NCEP-ATPIII criteria had significantly higher levels of leukocyte count (P<0.001) and PAI-1 (P<0.001), while no significant differences were found for fibrinogen or vWF (P>0.05). Using the WHO criteria, similar results were found except for vWF, where higher levels were found in subjects with the metabolic syndrome. When subjects were classified according to the number of components of the metabolic syndrome, levels of leukocyte count, vWF and PAI-1 activity were significantly different (P<0.05). In logistic regression analysis PAI-1, gender and leukocyte count were independent determinants of the metabolic syndrome (P<0.001).
Conclusion:
Evidence for being a true component of the metabolic syndrome is strong for PAI-1, less for leukocyte count and weak for vWF and fibrinogen.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Eckel RH, Krauss RM, for the AHA Nutrition Committee. American Heart Association call to action: obesity as a major risk factor for coronary heart disease. Circulation 1998; 97: 2099–2100.
Reaven GM . Banting Lecture 1988. Role of insulin resistance in human disease. Diabetes 1988; 37: 1595–1607.
World Health Organization. Definition, Diagnosis and Classification of Diabetes Mellitus and its Complications: Report of a WHO Consultation. Geneva, 1999, WHO/NCD/NCS 99.2.
National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002; 106: 3143–3421.
Libby P, Ridker PM, Maseri A . Inflammation and atherosclerosis. Circulation 2002; 105: 1135–1143.
Stenvinkel P . Endothelial dysfunction and inflammation – is there a link? Nephrol Dial Transplant 2001; 16: 1968–1971.
Esmon CT . Inflammation and thrombosis. J Thromb Haemost 2003; 1: 1343–1348.
Festa A, D'Agostino Jr R, Howard G, Mykkanen L, Tracy RP, Haffner SM . Chronic subclinical inflammation as part of the insulin resistance syndrome: the Insulin Resistance Atherosclerosis Study (IRAS). Circulation 2000; 102: 42–47.
Yudkin JS . Abnormalities of coagulation and fibrinolysis in insulin resistance. Evidence for a common antecedent? Diabetes Care 1999; 22 (Suppl 3): C25–C30.
Mertens I, Van Gaal LF . Obesity, haemostasis and the fibrinolytic system. Obes Rev 2002; 3: 85–101.
Lukaski HC, Johnson PE, Bolonchuk WW, Lykken GI . Assessment of fat-free mass using bioelctrical impedance measurements of the human body. Am J Clin Nutr 1985; 41: 810–817.
Deurenberg P, Weststrate JA, Hautvast JGAJ . Changes in fat-free mass during weight loss measured by bioelectrical impedance and by densitometry. Am J Clin Nutr 1989; 49: 33–36.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC . Homeostasis model assessment: insulin resistance and β-cell function from fasting glucose and insulin concentrations in man. Diabetologia 1985; 28: 412–419.
Lievens MM, Ketelslegers JM . Immunonephelometric method evaluated for determining low concentration of albumin in urine. Clin Chem 1988; 34: 992–993.
Balkau B, Charles MA . Comment on the provisional report from the WHO consultation. European Group for the Study of Insulin Resistance (EGIR). Diabet Med 1999; 16: 442–443.
Bonora E, Formentini G, Calcaterra F, Lombardi S, Marini F, Zenari L et al. HOMA-estimated insulin resistance is an independent predictor of cardiovascular disease in type 2 diabetic subjects: prospective data from the Verona Diabetes Complications Study. Diabetes Care 2002; 25: 1135–1141.
Ford ES . The metabolic syndrome and C-reactive protein, fibrinogen, and leukocyte count: findings from the Third National Health and Nutrition Examination Survey. Atherosclerosis 2003; 168: 351–358.
Case CC, Jones PH, Nelson K, O'Brian Smith E, Ballantyne CM . Impact of weight loss on the metabolic syndrome. Diabetes Obes Metab 2002; 4: 407–414.
Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA 2002; 288: 2709–2716.
Anand SS, Yi Q, Gerstein H, Lonn E, Jacobs R, Vuksan V et al. Study of Health Assessment and Risk in Ethnic Groups; Study of Health Assessment and Risk Evaluation in Aboriginal Peoples Investigators. Relationship of metabolic syndrome and fibrinolytic dysfunction to cardiovascular disease. Circulation 2003; 108: 420–425.
Bonora E, Kiechl S, Willeit J, Oberhollenzer F, Egger G, Bonadonna RC, et al., Bruneck Study. Metabolic syndrome: epidemiology and more extensive phenotypic description. Cross-sectional data from the Bruneck Study. Int J Obes Relt Metab Disord 2003; 27: 1283–1289.
Muntner P, He J, Chen J, Fonseca V, Whelton PK . Prevalence of non-traditional cardiovascular disease risk factors among persons with impaired fasting glucose, impaired glucose tolerance, diabetes and the metabolic syndrome: analysis of the Third National Health and Nutrition Examination Survey (NHANES III). Ann Epidemiol 2004; 14: 686–695.
Marques-Vidal P, Mazoyer E, Bongard V, Gourdy P, Ruidavets JB, Drouet L et al. Prevalence of insulin resistance syndrome in south-western France and its relationship with inflammatory and hemostatic markers. Diabetes Care 2002; 25: 1371–1377.
Agewall S, Bokemark L, Wikstrand J, Lindahl A, Fagerberg B . Insulin sensitivity and hemostatic factors in clinically healthy 58-year-old men. Thromb Haemost 2000; 84: 571–575.
Lim HS, Lip GY, Blann AD . Plasma von Willebrand Factor and the development of the metabolic syndrome in patients with hypertension. J Clin Endocrinol Metab 2004; 89: 5377–5381.
Ridker PM, Wilson PW, Grundy SM . Should C-reactive protein be added to metabolic syndrome and to assessment of global cardiovascular risk? Circulation 2004; 109: 2818–2825.
Juhan-Vague I, Thompson SG, Jespersen J . Involvement of the hemostatic system in the insulin resistance syndrome. A study of 1500 patients with angina pectoris. The ECAT Angina Pectoris Study Group. Arterioscler Thromb 1993; 13: 1865–1873.
Thogersen AM, Jansson JH, Boman K, Nilsson TK, Weinehall L, Huhtasaari F et al. High plasminogen activator inhibitor and tissue plasminogen activator levels in plasma precede a first acute myocardial infarction in both men and women: evidence for the fibrinolytic system as an independent primary risk factor. Circulation 1998; 98: 2241–2247.
Festa A, D'Agostino Jr R, Tracy RP, Haffner SM: Insulin Resistance Atherosclerosis Study. Elevated levels of acute-phase proteins and plasminogen activator inhibitor-1 predict the development of type 2 diabetes: the insulin resistance atherosclerosis study. Diabetes 2002; 51: 1131–1137.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mertens, I., Verrijken, A., Michiels, J. et al. Among inflammation and coagulation markers, PAI-1 is a true component of the metabolic syndrome. Int J Obes 30, 1308–1314 (2006). https://doi.org/10.1038/sj.ijo.0803189
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0803189
Keywords
This article is cited by
-
Role of PAI-1 in hepatic steatosis and dyslipidemia
Scientific Reports (2021)
-
Perimenopause, body fat, metabolism and menopausal symptoms in relation to serum markers of adiposity, inflammation and digestive metabolism
Journal of Endocrinological Investigation (2020)
-
Cardiometabolic importance of 1-h plasma glucose in obese subjects
Nutrition & Diabetes (2019)
-
The plasminogen activator inhibitor-1 paradox in cancer: a mechanistic understanding
Cancer and Metastasis Reviews (2019)
-
Cell adhesion molecules and plasminogen activator inhibitor type-1 (PAI-1) in patients with rheumatoid arthritis: influence of metabolic syndrome
Clinical and Experimental Medicine (2018)