Abstract
BACKGROUND:
Observational studies have shown an inverse association between dietary calcium intake and body weight, and a causal relation is likely. However, the underlying mechanisms are not understood.
OBJECTIVE:
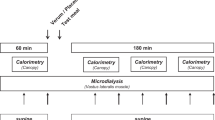
We examined whether high and low calcium intakes from mainly low-fat dairy products, in diets high or normal in protein content, have effects on 24-h energy expenditure (EE) and substrate oxidation, fecal energy and fat excretion, and concentrations of substrates and hormones involved in energy metabolism and appetite.
DESIGN:
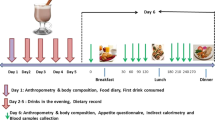
In all, 10 subjects participated in a randomized crossover study of three isocaloric 1-week diets with: low calcium and normal protein (LC/NP: 500 mg calcium, 15% of energy (E%) from protein), high calcium and normal protein (HC/NP: 1800 mg calcium, 15E% protein), and high calcium and high protein (HC/HP: 1800 mg calcium, 23E% protein).
RESULTS:
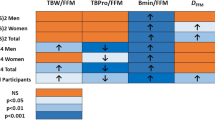
The calcium intake had no effect on 24-h EE or fat oxidation, but fecal fat excretion increased ∼2.5-fold during the HC/NP diet compared with the LC/NP and the HC/HP diets (14.2 vs 6.0 and 5.9 g/day; P<0.05). The HC/NP diet also increased fecal energy excretion as compared with the LC/NP and the HC/HP diets (1045 vs 684 and 668 kJ/day; P<0.05). There were no effects on blood cholesterol, free fatty acids, triacylglycerol, insulin, leptin, or thyroid hormones.
CONCLUSIONS:
A short-term increase in dietary calcium intake, together with a normal protein intake, increased fecal fat and energy excretion by ∼350 kJ/day. This observation may contribute to explain why a high-calcium diet produces weight loss, and it suggests that an interaction with dietary protein level may be important.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Davies KM, Heaney RP, Recker RR, Lappe JM, Barger-Lux MJ, Rafferty K, Hinders S . Calcium intake and body weight. J Clin Endocrinol Metab 2000; 85: 4635–4638.
Zemel MB, Shi H, Greer B, Dirienzo D, Zemel PC . Regulation of adiposity by dietary calcium. FASEB J 2000; 14: 1132–1138.
Zemel MB . Effects of calcium-fortified breakfast cereal on adiposity in a transgenic mouse model of obesity. FASEB J 2001; 15: A598.
Zemel MB, Thompson W, Zemel P, Nocton AM, Milstead A, Morris K, Campbell P . Dietary calcium and dairy products accelerate weight and fat loss during energy restriction in obese adults. Am J Clin Nutr 2002; 70 (Suppl): 342–343.
Heaney RP . Normalizing calcium intake: projected population effects for body weight. J Nutr 2003; 133: 268S–270S.
Papakonstantinou E, Flatt WP, Huth PJ, Harris RBS . High dietary calcium reduces body fat content, digestibility of fat, and serum vitamin D in rats. Obes Res 2003; 11: 387–394.
Denke MA, Fox MM, Schulte MC . Short-term dietary calcium fortification increases fecal saturated fat content and reduces serum lipids in men. J Nutr 1993; 123: 1047–1053.
Shahkhalili Y, Murset C, Meirim I, Duruz E, Guinchard S, Cavadini C, Acheson K . Calcium supplementation of chocolate: effect on cocoa butter digestibility and blood lipids in humans. Am J Clin Nutr 2001; 73: 246–252.
Klausen B, Toubro S, Astrup A . Age and sex effects on energy expenditure. Am J Clin Nutr 1997; 65: 895–907.
Heitmann BL . Prediction of body water and fat in adult Danes from measurement of electrical impedance. A validation study. Int J Obes Relat Metab 1990; 14: 789–802.
Black E, Petersen L, Kreutzer M, Toubro S, Sorensen TI, Pedersen O, Astrup A . Fat mass measured by DXA varies with scan velocity. Obes Res 2002; 10: 69–77.
Astrup A, Thorbek G, Lind J, Isaksson B . Prediction of 24 h energy expenditure and its components from physical characteristics and body composition in normal-weight humans. Am J Clin Nutr 1990; 52: 777–783.
Elia M, Livesey G . Energy expenditure and fuel selection in biological systems: the theory and practice of calculations based on indirect calorimetry and tracer methods. World Rev Nutr Diet 1992; 70: 68–131.
Bligh EG, Dyer WJ . A rapid method of total lipid extraction and purification. Can J Biochem Physiol 1959; 37: 911–917.
Cummings JH, Wiggins HS . Transit through the gut measured by analysis of a single stool. Gut 1976; 17: 219–223.
Welberg JW, Monkelbaan JF, de Vries EG, Muskiet FA, Cats A, Oremus ET, Boersma-van Ek W, van Rijsbergen H, van der Meer R, Mulder NH . Effects of supplemental dietary calcium on quantitative and qualitative fecal fat excretion in man. Ann Nutr Metab 1994; 38: 185–191.
Andersen NL, Fragt S, Groth MV, Hartkopp HB, Moller A, Ovesen L, Warming DL . Danskernes Kostvaner. Levnedsmiddelstyrelsen: Quickly Tryk A/S; 1995.
Economic Research Service US. Department of Agriculture. Diet and Health: Food Consumption and Nutrient Intake Tables, Internet: http://www.ers.usda.gov/Briefing/DietAndHealth/data/nutrients/.
Mikkelsen PB, Toubro S, Astrup A . Effect of fat-reduced diets on 24-h energy expenditure: comparisons between animal protein, vegetable protein, and carbohydrate. Am J Clin Nutr 2000; 72: 1135–1141.
Yuangklang C, Wensing T, Van den Broek L, Jittakhot S, Beynen AC . Fat digestion in veal calves fed milk replacers low or high in calcium and containing either casein or soy protein isolate. J Dairy Sci 2004; 87: 1051–1056.
Kerstetter JE, O'Brien KO, Insogna KL . Dietary protein, calcium metabolism, and skeletal homeostasis revisited. Am J Clin Nutr 2003; 78 (Suppl): 584S–592S.
Bowen J, Noakes M, Clifton PM . A high dairy protein, high-calcium diet minimizes bone turnover in overweight adults during weight loss. J Nutr 2004; 134: 568–573.
Melanson EL, Sharp TA, Schneider J, Donahoo WT, Grunwald GK, Hill JO . Relation between calcium intake and fat oxidation in adult humans. Int J Obes Relat Metab 2003; 27: 196–203.
McCarron DA, Reusser ME . Finding consensus in the dietary calcium–blood pressure debate. J Am Coll Nutr 1999; 18: 398S–405S.
Acknowledgements
We thank John Lind, Inge Timmermann, Helle R Christensen, Kirsten B Rasmussen, Martin Kreutzer, Charlotte Kostecki, Yvonne Rasmussen, and Karina G Rossen for their assistance. This work was financially supported by the Danish Dairy Board, Aarhus, Denmark and The Directorate for Food, Fisheries and Argi Business, the Danish Ministry of Food, Agriculture and Fisheries, Copenhagen, Denmark.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jacobsen, R., Lorenzen, J., Toubro, S. et al. Effect of short-term high dietary calcium intake on 24-h energy expenditure, fat oxidation, and fecal fat excretion. Int J Obes 29, 292–301 (2005). https://doi.org/10.1038/sj.ijo.0802785
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0802785
Keywords
This article is cited by
-
Effect of reduced-calcium and high-calcium cheddar cheese consumption on the excretion of faecal fat: a 2-week cross-over dietary intervention study
European Journal of Nutrition (2023)
-
Healthy beverages may reduce the genetic risk of abdominal obesity and related metabolic comorbidities: a gene-diet interaction study in Iranian women
Diabetology & Metabolic Syndrome (2022)
-
Dietary calcium, phosphorus, and osteosarcopenic adiposity in Korean adults aged 50 years and older
Archives of Osteoporosis (2021)
-
Association between milk intake and childhood growth: results from a nationwide cross-sectional survey
International Journal of Obesity (2020)
-
High phosphorus intake and gut-related parameters – results of a randomized placebo-controlled human intervention study
Nutrition Journal (2018)