Abstract
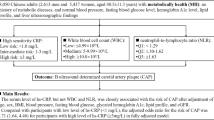
OBJECTIVE: This study sought to determine the relationship between levels of the inflammatory marker, C-reactive protein (CRP), cardiovascular risk factors and oral contraceptive use in young adults.
DESIGN: Cross-sectional study of a community cohort.
SUBJECTS: A total of 822 men and women aged 26 y.
MEASUREMENTS: CRP, body mass index (BMI), blood pressure, lipid and lipoprotein levels, smoking status, socioeconomic status, health status, and hormonal contraceptive use in women.
RESULTS: Multiple regression analysis showed that obesity was independently related to CRP with an increase in ratio CRP of 1.03 (95% CI 1.01, 1.05) for men and 1.07 (1.05, 1.09) for women associated with a 1 kg/m2 increase in BMI. In women, combined oral contraceptive use was associated with a ratio change in CRP of 1.52 (1.27, 1.82) compared with nonusers. Other independent determinants of CRP in men and women were apolipoprotein B level, systolic blood pressure and apolipoprotein A1 in men. Univariate analysis showed that the relationship between CRP and BMI, systolic blood pressure and apolipoprotein B was significantly stronger in women than men.
CONCLUSION: These findings suggest that obesity is associated with inflammation independent of other cardiovascular risk factors that may contribute to an increased risk for cardiovascular disease in men and women. Elevated CRP related to combined oral contraceptive use may influence the rate of cardiovascular events in young women.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Libby P, Ridker PM, Maseri A . Inflammation and atherosclerosis. Circulation 2002; 105: 1135–1143.
Ridker PM . High-sensitivity C-reactive protein: potential adjunct for global risk assessment in the primary prevention of cardiovascular disease. Circulation 2001; 103: 1813–1818.
Ridker PM, Rifai N, Rose L, Buring JE, Cook NR . Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. N Engl J Med 2002; 347: 1557–1565.
Mendall MA, Patel P, Ballam L, Strachan D, Northfield TC . C reactive protein and its relation to cardiovascular risk factors: a population based cross sectional study. BMJ 1996; 312: 1061–1065.
Ridker PM, Buring JE, Cook NR, Rifai N . C-reactive protein, the metabolic syndrome, and risk of incident cardiovascular events: an 8-year follow-up of 14 719 initially healthy American women. Circulation 2003; 107: 391–397.
WHO Consultation on Obesity. Preventing and managing the global epidemic. World Health Organization: Geneva; 1997. pp 1–276.
Rabkin SW, Mathewson FA, Hsu PH . Relation of body weight to development of ischemic heart disease in a cohort of young North American men after a 26 year observation period: the Manitoba Study. Am J Cardiol 1977; 39: 452–458.
Tuomilehto J, Salonen JT, Marti B, Jalkanen L, Puska P, Nissinen A, Wolf E . Body weight and risk of myocardial infarction and death in the adult population of Eastern Finland. BMJ 1987; 295: 623–627.
Visser M, Bouter LM, McQuillan GM, Wener MH, Harris TB . Elevated C-reactive protein levels in overweight and obese adults. JAMA 1999; 282: 2131–2135.
Koenig W, Sund M, Frohlich M, Fischer HG, Lowel H, Doring A, Hutchinson WL, Pepys MB . C-Reactive protein, a sensitive marker of inflammation, predicts future risk of coronary heart disease in initially healthy middle-aged men: results from the MONICA (Monitoring Trends and Determinants in Cardiovascular Disease) Augsburg Cohort Study, 1984 to 1992. Circulation 1999; 99: 237–242.
Yudkin JS, Stehouwer CD, Emeis JJ, Coppack SW . C-reactive protein in healthy subjects: associations with obesity, insulin resistance, and endothelial dysfunction: a potential role for cytokines originating from adipose tissue? Arterioscler Thromb Vasc Biol 1999; 19: 972–978.
Skouby SO, Gram J, Andersen LF, Sidelmann J, Petersen KR, Jespersen J . Hormone replacement therapy: estrogen and progestin effects on plasma C-reactive protein concentrations. Am J Obstet Gynecol 2002; 186: 969–977.
Walsh BW, Paul S, Wild RA, Dean RA, Tracy RP, Cox DA, Anderson PW . The effects of hormone replacement therapy and raloxifene on C-reactive protein and homocysteine in healthy postmenopausal women: a randomized, controlled trial. J Clin Endocrinol Metab 2000; 85: 214–218.
Pradhan AD, Manson JE, Rossouw JE, Siscovick DS, Mouton CP, Rifai N, Wallace RB, Jackson RD, Pettinger MB, Ridker PM . Inflammatory biomarkers, hormone replacement therapy, and incident coronary heart disease: prospective analysis from the Women's Health Initiative observational study. JAMA 2002; 288: 980–987.
Kay DR, Bole Jr GG, Ledger WJ . Antinuclear antibodies, rheumatoid factor and C-reactive protein in serum of normal women using oral contraceptives. Arthritis Rheum 1971; 14: 239–248.
Connell EB, Connell JT . C-reactive protein in pregnancy and contraception. Am J Obstet Gynecol 1971; 110: 633–639.
Kluft C, Leuven JAG, Helmerhorst FM, Krans HMJ . Pro-inflammatory effects of oestrogens during use of oral contraceptives and hormone replacement treatment. Vasc Pharmacol 2002; 39: 149–154.
Engel HJ, Engel E, Lichtlen PR . Coronary atherosclerosis and myocardial infarction in young women: role of oral contraceptives. Eur Heart J 1983; 4: 1–6.
Silva PA, Stanton WR (eds). From child to adult: the Dunedin Multidisciplinary Health and Development Study. Oxford University Press: Auckland; 1996.
Perloff D, Grim C, Flack J, Frohlich ED, Hill M, McDonald M, Morgenstern BZ . Human blood pressure determination by sphygmomanometry. Circulation 1993; 88: 2460–2470.
Elley WB, Irving JC . The Elley–Irving socio-economic index 1981 census revision. N Z J Educ Stud 1985; 29: 115–128.
Larsson B, Svardsudd K, Welin L, Wilhelmsen L, Bjorntorp P, Tibblin G . Abdominal adipose tissue distribution, obesity, and risk of cardiovascular disease and death: 13 year follow up of participants in the study of men born in 1913. BMJ 1984; 288: 1401–1404.
Hubert HB, Feinleib M, McNamara PM, Castelli WP . Obesity as an independent risk factor for cardiovascular disease: a 26-year follow-up of participants in the Framingham Heart Study. Circulation 1983; 67: 968–977.
Despres JP, Lemieux I, Prud'homme D . Treatment of obesity: need to focus on high risk abdominally obese patients. BMJ 2001; 322: 716–720.
Heinrich PC, Castell JV, Andus T . Interleukin-6 and the acute phase response. Biochem J 1990; 265: 621–636.
Ziccardi P, Nappo F, Giugliano G, Esposito K, Marfella R, Cioffi M, D'Andrea F, Molinari AM, Giugliano D . Reduction of inflammatory cytokine concentrations and improvement of endothelial functions in obese women after weight loss over one year. Circulation 2002; 105: 804–809.
Festa A, D'Agostino Jr R, Williams K, Karter AJ, Mayer-Davis EJ, Tracy RP, Haffner SM . The relation of body fat mass and distribution to markers of chronic inflammation. Int J Obes Relat Metab Disord 2001; 25: 1407–1415.
Gallagher D, Visser M, Sepulveda D, Pierson RN, Harris T, Heymsfield SB . How useful is body mass index for comparison of body fatness across age, sex, and ethnic groups? Am J Epidemiol 1996; 143: 228–239.
Godsland IF, Winkler U, Lidegaard O, Crook D . Occlusive vascular diseases in oral contraceptive users. Epidemiology, pathology and mechanisms. Drugs 2000; 60: 721–869.
Tchernof A, Lamarche B, Prud'Homme D, Nadeau A, Moorjani S, Labrie F, Lupien PJ, Despres JP . The dense LDL phenotype: association with plasma lipoprotein levels, visceral obesity, and hyperinsulinemia in men. Diabetes Care 1996; 19: 629–637.
Lamarche B, Tchernof A, Mauriege P, Cantin B, Dagenais GR, Lupien PJ, Despres JP . Fasting insulin and apolipoprotein B levels and low-density lipoprotein particle size as risk factors for ischemic heart disease. JAMA 1998; 279: 1955–1961.
Esposito K, Pontillo A, Di Palo C, Giugliano G, Masella M, Marfella R, Giugliano D . Effect of weight loss and lifestyle changes on vascular inflammatory markers in obese women: a randomized trial. JAMA 2003; 289: 1799–1804.
Acknowledgements
We thank the Dunedin Study members, Unit research staff, Air New Zealand and the study founder Phil Silva. The Dunedin Multidisciplinary Health and Development Research Unit is supported by the New Zealand Health Research Council. Data collection was supported by grants from the National Heart Foundation of New Zealand and the University of Otago (Otago Research Grant).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Williams, M., Williams, S., Milne, B. et al. Association between C-reactive protein, metabolic cardiovascular risk factors, obesity and oral contraceptive use in young adults. Int J Obes 28, 998–1003 (2004). https://doi.org/10.1038/sj.ijo.0802713
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0802713
Keywords
This article is cited by
-
Early age at menarche and metabolic cardiovascular risk factors: mediation by body composition in adulthood
Scientific Reports (2021)
-
Impact of contraception and IVF hormones on metabolic, endocrine, and inflammatory status
Journal of Assisted Reproduction and Genetics (2020)
-
Increased systemic elastase and C-reactive protein in aggressive periodontitis (CLOI-D-00160R2)
Clinical Oral Investigations (2012)
-
Association between serum levels of C-reactive protein and personality traits in women
Behavioral and Brain Functions (2008)
-
Socioeconomic and racial/ethnic differentials of C-reactive protein levels: a systematic review of population-based studies
BMC Public Health (2007)