Abstract
BACKGROUND: In normal-weight subjects, resting energy expenditure (REE) can be accurately calculated from organ and tissue masses applying constant organ-specific metabolic rates. This approach allows a precise correction for between-subjects variation in REE, explained by body composition. Since a decrease in organ metabolic rate with increasing organ mass has been deduced from interspecies comparison including human studies, the validity of the organ- and tissue-specific REE calculation remains to be proved over a wider range of fat-free mass (FFM).
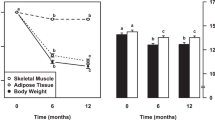
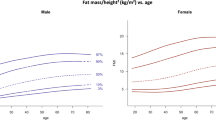
DESIGN: In a cross-sectional study on 57 healthy adults (35 females and 22 males, 19–43 y; 14 underweight, 25 intermediate weight and 18 obese), magnetic resonance imaging (MRI) and dual-energy X-ray absorptiometry (DXA) were used to assess the masses of brain, internal organs, skeletal muscle (MM), bone and adipose tissue. REE was measured by indirect calorimetry (REEm) and calculated from detailed organ size determination by MRI and DXA (REEc1), or in a simplified approach exclusively from DXA (REEc2).
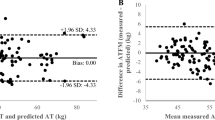
RESULTS: We found a high agreement between REEm and REEc1 over the whole range of FFM (28–86 kg). REE prediction errors were −17±505, −145±514 and −141±1058 kJ/day in intermediate weight, underweight and obese subjects, respectively (n.s.). Regressing REEm on FFM resulted in a significant positive intercept of 1.6 MJ/day that could be reduced to 0.5 MJ/day by adjusting FFM for the proportion of MM/organ mass. In a multiple regression analysis, MM and liver mass explained 81% of the variance in REEm. DXA-derived REE prediction showed a good agreement with measured values (mean values for REEm and REEc2 were 5.72±1.87 and 5.82±1.51 MJ/day; difference n.s.).
CONCLUSION: Detailed analysis of metabolically active components of FFM allows REE prediction over a wide range of FFM. The data provide indirect evidence for a view that, for practical purposes within humans, the specific metabolic rate is constant with increasing organ mass. Nonlinearity of REE on FFM was partly explained by FFM composition. A simplified REE prediction algorithm from regional DXA measurements has to be validated in future studies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Elia M . Organ and tissue contribution to metabolic rate. In: Kinney JM, Tucker HN (eds). Energy metabolism: tissue determinants and cellular corollaries. Raven: New York; 1992. pp 19–59.
Müller MJ, Bosy-Westphal A, Kutzner D, Heller M . Metabolically active components of fat-free mass and resting energy-expenditure in humans: recent lessons from imaging technologies. Obes Rev 2002; 3: 113–122.
Weinsier RL, Schutz Y, Bracco D . Reexamination of the relationship of resting metabolic rate to fat-free mass and to metabolically active components of fat-free mass in humans. Am J Clin Nutr 1992; 55: 790–794.
Ravussin E, Bogardus C . Relationship of genetics, age, and physical fitness to daily energy expenditure and fuel utilisation. Am J Clin Nutr 1989; 49 (Suppl): 968–975.
Sparti A, DeLany JP, de la Bretonne JA, Sander GE, Bray GA . Relationship between resting metabolic rate and the composition of the fat-free mass. Metabolism 1997; 46: 1225–1230.
Gallagher D, Belmonte D, Deurenberg P, Wang Z, Krasnow N, Pi-Sunyer FX, Heymsfield SB . Organ–tissue mass measurement allows modeling of REE and metabolically active tissue mass. Am J Physiol 1998; 275: E249–E258.
Gallagher D, Allen A, Wang Z, Heymsfield SB, Krasnow N . Smaller organ tissue mass in the elderly fails to explain lower resting metabolic rate. Ann NY Acad Sci 2000; 904: 449–455.
Illner K, Brinkmann G, Heller M, Bosy-Westphal A, Müller MJ . Metabolically active components of fat free mass and resting energy expenditure in nonobese adults. Am J Physiol 2000; 278: E308–E315.
Bosy-Westphal A, Eichhorn C, Kutzner D, Illner K, Heller M, Müller MJ . The age-related decline in resting energy expenditure in humans is due to the loss of fat-free mass and to alterations in its metabolically active components. J Nutr 2003; 133: 2356–2362.
Wang ZM, O'Connor TP, Heshka S, Heymsfield SB . The reconstruction of Kleiber's law at the organ-tissue level. J Nutr 2001; 131: 2967–2970.
Müller MJ, Illner K, Bosy-Westphal A, Brinkmann G, Heller M . Regional lean body mass and resting energy expenditure in non-obese adults. Eur J Nutr 2001; 40: 93–97.
Hayes M, Chustek M, Wang ZM, Gallagher D, Heshka S, Spungen A, Baumann W, Heymsfield SB . DXA: potential for creating a metabolic map of organ–tissue resting energy expenditure components. Obes Res 2002; 10: 969–977.
Kirstorp CN, Toubro S, Astrup A, Svendsen OL . Measurement of body composition by dual-energy X-ray absorptiometry improve prediction of energy expenditure. Ann NY Acad Sci 2000; 904: 79–84.
Kim J, Wang Z, Heymsfield SB, Baumgartner RN, Gallagher D . Total-body skeletal muscle mass: estimation by a new dual-energy X-ray absorptiometry method. Am J Clin Nutr 2002; 76: 378–383.
Diagnostic and Statistical Manual of Mental Disorders — Fourth edn. (DSM-IV). American Psychiatric Association: Washington, DC; 1994.
Müller MJ, von zur Mühlen A, Lautz HU, Schmidt FW, Daiber M, Hürter P . Energy expenditure in children with type 1 diabetes: evidence for increased thermogenesis. Br Med J 1989; 299: 487–491.
Goldberg GR, Black AE, Jebb SA, Cole TJ, Murgatroyd PR, Coward WA, Prentice AM . Critical evaluation of energy intake data using fundamental principles of energy physiology: 1. Deviation of cut-off limits to identify underrecording. Eur J Clin Nutr 1991; 45: 569–581.
Souci SW, Fachmann W, Kraut H . Die Zusammensetzung der Lebensmittel — Nährwerttabellen. Wissenschaftliche Verlagsgesellschaft, Stuttgart 6. Auflage, 2000.
Bundesinstitut für Gesundheitlichen Verbraucherschutz und Veterinärmedizin (BgVV) Bundeslebensmittelschlüssel, Version II.3. Berlin, 1999.
Snyder WS, Cook MJ, Nasset ES, Karhausen LR, Howells GP, Tipton IH . Report of the Task Group on Reference Man. Pergamon Press: Oxford; 1975.
Duck FA . Physical Properties of Tissue. Academic: New York; 1990.
Heymsfield SB, Gallagher D, Kotler DP, Wang Z, Allison DB, Heshka S . Body-size dependence of resting energy expenditure can be attributed to non-energetic homogeneity of fat-free mass. Am J Physiol Endocrinol Metab 2002; 282: E132–E138.
Nevill AM, Ramsbottom R, Williams C . Scaling physiological performance measurements for individuals of different body size. Eur J Appl Physiol Occup Physiol 1992; 65: 110–117.
Calder III WA . Size, Function and Life History. Dover: New York; 1996.
Rubner M . Über den Einfluß der Körpergröße auf Stoff- und Kraft-wechsel. Z Biol 1883; 19: 535–562.
Heymsfield SB . Heat and life: the ongoing scientific odyssey. J Parent Ent Nutr 2002; 26: 319–332.
Cunningham JJ . A reanalysis of the factors influencing basal metabolic rate in normal adults. Am J Clin Nutr 1980; 33: 2372–2374.
Kinney JM, Lister J, Moore FD . Relationship of energy expenditure to total exchangeable potassium. Ann NY Acad Sci 1963; 10: 711–722.
Müller MJ, Böttcher J, Selberg O, Weselmann S, Böker KH, Schwarze M, von zur Mühlen A, Manns MP . Hypermetabolism in clinically stable patients with liver cirrhosis. Am J Clin Nutr 1999; 69: 1194–1201.
Cooling J, Blundell J . Differences in energy expenditure and substrate oxidation between habitual high fat and low fat consumers (phenotypes). Int J ObesRelat- Metal Disord. 1998; 22: 612–618.
Acknowledgements
This work was supported by a grant from the Deutsche Forschungsgemeinschaft (DFG Mü 714/8-1) and by Precon, Bickenbach, Germany.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bosy-Westphal, A., Reinecke, U., Schlörke, T. et al. Effect of organ and tissue masses on resting energy expenditure in underweight, normal weight and obese adults. Int J Obes 28, 72–79 (2004). https://doi.org/10.1038/sj.ijo.0802526
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0802526
Keywords
This article is cited by
-
Challenges of considering both extremities of the weight status spectrum to better understand obesity: insights from the NUTRILEAN project in constitutionally thin individuals
International Journal of Obesity (2023)
-
A Step-Wise Multiple Testing for Linear Regression Models with Application to the Study of Resting Energy Expenditure
Statistics in Biosciences (2023)
-
Tissue losses and metabolic adaptations both contribute to the reduction in resting metabolic rate following weight loss
International Journal of Obesity (2022)
-
Effects of functional electro-stimulation combined with blood flow restriction in affected muscles by spinal cord injury
Neurological Sciences (2022)
-
Repository Describing the Anatomical, Physiological, and Biological Changes in an Obese Population to Inform Physiologically Based Pharmacokinetic Models
Clinical Pharmacokinetics (2022)