Abstract
OBJECTIVE: To investigate whether the changes in vascular endothelial growth factor (VEGF) and basic fibroblast growth factor (bFGF) concentrations before and after weight reduction in Japanese overweight men are associated with changes in body mass index (BMI), visceral, subcutaneous fat, VO2 and work rate (WR) at ventilatory threshold (VT).
DESIGN: Cross-sectional and longitudinal clinical intervention study with exercise education.
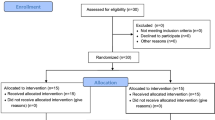
SUBJECTS: In total, 30 Japanese overweight men (BMI, 29.0±2.2 kg/m2) and 31 normal-weight men (BMI, 22.5±1.6 kg/m2) at baseline were enrolled: 30 overweight men (BMI, 29.0±2.2 kg/m2) were further enrolled into a 6-month exercise program.
MEASUREMENTS: Fat distribution evaluated by visceral fat (V) and subcutaneous fat (S) areas measured with computed tomography scanning at umbilical levels, angiogenic peptides including VEGF and bFGF, exercise tests at baseline and after 6 months.
RESULTS: In normal-weight and overweight subjects at baseline, VEGF positively correlated with S area (r=0.350, P=0.007) but not with V area. In contrast, bFGF negatively correlated with BMI (r=−0.619, P<0.001), S (r=−0.457, P<0.001) and V areas (r=−0.466, P<0.001). By intervention with exercise education, 30 overweight subjects showed reduction in BMI (29.0±2.2 to 28.0±2.0, P<0.001), V and S areas, increase in VO2 and WR at VT, increase in bFGF (9.21±5.82–21.2±7.04 ng/ml, P<0.001), and no change in VEGF (1.45±0.72–1.88±0.52 ng/ml, P=0.016). The stepwise multiple regression analysis revealed that ΔBMI (β=−6.052) and ΔVO2 (β=2.806) were independently related to ΔbFGF (P<0.001) and all other variables including ΔS area, and ΔV area, and ΔWR did not enter the equation at significant levels.
CONCLUSION: The present study indicated a negative correlation between serum bFGF levels and BMI at baseline as well as an association of ΔBMI and ΔVO2 with ΔbFGF after exercise intervention. The exercise-induced elevation of bFGF may be beneficial in the prevention of the atherosclerosis in overweight subjects.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Stevens J, Cai J, Pamuk ER, Williamson DF, Thun MJ, Wood JL . The effect of age on the association between body-mass index and mortality. N Engl J Med 1998; 338: 1–7.
Kannel WB, Cupples LA, Ramaswami R, Stokes III J, Kreger BE, Higgins M . Regional obesity and risk of cardiovascular disease; the Framingham Study. J Clin Epidemiol 1991; 44: 183–190.
Rexrode KM, Carey VJ, Hennekens CH, Walters EE, Colditz GA, Stampfer MJ, Willett WC, Manson JE . Abdominal adiposity and coronary heart disease in women. JAMA 1998; 280: 1843–1848.
Funahashi T, Nakamura T, Shimomura I, Maeda K, Kuriyama H, Takahashi M, Arita Y, Kihara S, Matsuzawa Y . Role of adipocytokines on the pathogenesis of atherosclerosis in visceral obesity. Intern Med 1999; 38: 202–206.
Asano A, Kimura K, Saito M . Cold-induced mRNA expression of angiogenic factors in rat brown adipose tissue. J Vet Med Sci 1999; 61: 403–409.
Tonello C, Giordano A, Cozzi V, Cinti S, Stock MJ, Carruba MO, Nisoli E . Role of sympathetic activity in controlling the expression of vascular endothelial growth factor in brown fat cells of lean and genetically obese rats. FEBS Lett 1999; 442: 167–172.
Asano A, Irie Y, Saito M . Isoform-specific regulation of vascular endothelial growth factor (VEGF) family mRNA expression in cultured mouse brown adipocytes. Mol Cell Endocrinol 2001; 174: 71–76.
Mick GJ, Wang X, McCormick K . White adipocyte vascular endothelial growth factor: regulation by insulin. Endocrinology 2002; 143: 948–953.
Carmeliet P . Mechanisms of angiogenesis and arteriogenesis. Nat Med 2000; 6: 389–395.
Teichert-Kuliszewska K, Hamilton BS, Deitel M, Roncari DA . Augmented production of heparin-binding mitogenic proteins by preadipocytes from massively obese persons. J Clin Invest 1992; 90: 1226–1231.
Teichert-Kuliszewska K, Hamilton BS, Deitel M, Roncari DA . Decreasing expression of a gene encoding a protein related to basic fibroblast growth factor during differentiation of human preadipocytes. Biochem Cell Biol 1994; 72: 54–57.
Navre M, Ringold GM . Differential effects of fibroblast growth factor and tumor promoters on the initiation and maintenance of adipocyte differentiation. J Cell Biol 1989; 109(Part 1): 1857–1863.
Hauner H, Rohrig K, Petruschke T . Effects of epidermal growth factor (EGF), platelet-derived growth factor (PDGF) and fibroblast growth factor (FGF) on human adipocyte development and function. Eur J Clin Invest 1995; 25: 90–96.
Cohen B, Barkan D, Levy Y, Goldberg I, Fridman E, Kopolovic J, Rubinstein M . Leptin induces angiopoietin-2 expression in adipose tissues. J Biol Chem 2001; 276: 7697–7700.
Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults—The Evidence Report National Institutes of Health. Obes Res 1998; 6 (Suppl 2): 51S–209S.
Gordon T, Castelli WP, Hjortland MC, Kannel WB, Dawber TR . High density lipoprotein as a protective factor against coronary heart disease. The Framingham Study. Am J Med 1977; 62: 707–714.
Haffner SM, Kennedy E, Gonzalez C, Stern MP, Miettinen H . A prospective analysis of the HOMA model. The Mexico City Diabetes Study. Diabetes Care 1996; 19: 1138–1141.
Kunitomi M, Wada J, Takahashi K, Tsuchiyama Y, Mimura Y, Hida K, Miyatake N, Fujii M, Kira S, Shikata K, Maknio H . Relationship between reduced serum IGF-I levels and accumulation of visceral fat in Japanese men. Int J Obes Relat Metab Disord 2002; 26: 361–369.
Miyatake N, Nonaka K, Fujii M . A new air displacement plethysmograph for the determination of Japanese body composition. Diabetes Obes Metab 1999; 1: 347–351.
Jones NL, Makrides L, Hitchcock C, Chypchar T, McCartney N . Normal standards for an incremental progressive cycle ergometer test. Am Rev Respir Dis 1985; 131: 700–708.
Wasserman K, Whipp BJ, Koyl SN, Beaver WL . Anaerobic threshold and respiratory gas exchange during exercise. J Appl Physiol 1973; 35: 236–243.
Davis JA, Frank MH, Whipp BJ, Wasserman K . Anaerobic threshold alterations caused by endurance training in middle-aged men. J Appl Physiol 1979; 46: 1039–1046.
Beaver WL, Wasserman K, Whipp BJ . A new method for detecting anaerobic threshold by gas exchange. J Appl Physiol 1986; 60: 2020–2027.
Freedman SB, Isner JM . Therapeutic angiogenesis for coronary artery disease. Ann Intern Med 2002; 136: 54–71.
Celletti FL, Hilfiker PR, Ghafouri P, Dake MD . Effect of human recombinant vascular endothelial growth factor165 on progression of atherosclerotic plaque. J Am Coll Cardiol 2001; 37: 2126–2130.
Blann AD, Belgore FM, Constans J, Conri C, Lip GY . Plasma vascular endothelial growth factor and its receptor Flt-1 in patients with hyperlipidemia and atherosclerosis and the effects of fluvastatin or fenofibrate. Am J Cardiol 2001; 87: 1160–1163.
Celletti FL, Waugh JM, Amabile PG, Brendolan A, Hilfiker PR, Dake MD . Vascular endothelial growth factor enhances atherosclerotic plaque progression. Nat Med 2001; 7: 425–429.
Moulton KS, Heller E, Konerding MA, Flynn E, Palinski W, Folkman J . Angiogenesis inhibitors endostatin or TNP-470 reduce intimal neovascularization and plaque growth in apolipoprotein E-deficient mice. Circulation 1999; 99: 1726–1732.
Schulz R, Hummel C, Heinemann S, Seeger W, Grimminger F . Serum levels of vascular endothelial growth factor are elevated in patients with obstructive sleep apnea and severe nighttime hypoxia. Am J Resp Crit Care Med 2002; 165: 67–70.
Schultz A, Lavie L, Hochberg I, Beyar R, Stone T, Skorecki K, Lavie P, Roguin A, Levy AP . Interindividual heterogeneity in the hypoxic regulation of VEGF: significance for the development of the coronary artery collateral circulation. Circulation 1999; 100: 547–552.
Zhang QX, Magovern CJ, Mack CA, Budenbender KT, Ko W, Rosengart TK . Vascular endothelial growth factor is the major angiogenic factor in omentum: mechanism of the omentum-mediated angiogenesis. J Surg Res 1997; 67: 147–154.
Gustafsson T, Puntschart A, Kaijser L, Jansson E, Sundberg CJ . Exercise-induced expression of angiogenesis-related transcription and growth factors in human skeletal muscle. Am J Physiol 1999; 276(Part 2): H679–H685.
Gustafsson T, Sundberg CJ . Expression of angiogenic growth factors in human skeletal muscle in response to a singular bout of exercise. Am J Physiol Heart Circ Physiol 2000; 279: H3144–H3145.
Hiltunen MO, Laitinen M, Turunen MP, Jeltsch M, Hartikainen J, Rissanen TT, Laukkanen J, Niemi M, Kossila M, Hakkinen TP, Kivela A, Enholm B, Mansukoski H, Turunen AM, Alitalo K, Yla-Herttuala S . Intravascular adenovirus-mediated VEGF-C gene transfer reduces neointima formation in balloon-denuded rabbit aorta. Circulation 2000; 102: 2262–2268.
Kawaguchi N, Toriyama K, Nicodemou-Lena E, Inou K, Torii S, Kitagawa Y . De novo adipogenesis in mice at the site of injection of basement membrane and basic fibroblast growth factor. Proc Natl Acad Sci USA 1998; 95: 1062–1066.
Breen EC, Johnson EC, Wagner H, Tseng HM, Sung LA, Wagner PD . Angiogenic growth factor mRNA responses in muscle to a single bout of exercise. J Appl Physiol 1996; 81: 355–361.
Meurice T, Bauters C, Vallet B et al. bFGF restores endothelium-dependent responses of hypercholesterolemic rabbit thoracic aorta. Am J Physiol 1997; 272 (Part 2): H613–H617.
Acknowledgements
This study was approved by Ministry of Health, Labor and Welfare, Japan. This research was supported by Health Science Research Grants for ‘Research on Health Services’ from the Ministry of Health, Labor and Welfare, Japan. It was partly supported by Uehara Memorial Foundation, The Naito Foundation, ONO Medical Foundation to J Wada.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Seida, A., Wada, J., Kunitomi, M. et al. Serum bFGF levels are reduced in Japanese overweight men and restored by a 6-month exercise education. Int J Obes 27, 1325–1331 (2003). https://doi.org/10.1038/sj.ijo.0802408
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0802408
Keywords
This article is cited by
-
Angiogenic Potential, Circulating Angiogenic Factors and Insulin Resistance in Subjects with Obesity
Indian Journal of Clinical Biochemistry (2021)
-
Associations of Plasma FGF2 Levels and Polymorphisms in the FGF2 Gene with Obesity Phenotypes in Han Chinese Population
Scientific Reports (2016)
-
Vaspin gene in rat adipose tissue: relation to obesity-induced insulin resistance
Molecular and Cellular Biochemistry (2013)
-
Elevated Serum Monocyte Chemoattractant Protein‐4 and Chronic Inflammation in Overweight Subjects
Obesity (2006)
-
Angiogenic factors are elevated in overweight and obese individuals
International Journal of Obesity (2005)