Abstract
Objective: To assess tracking for body weight from childhood to adulthood in obese Japanese children who were treated for obesity, investigate the relation between the changes in body weight status and morbidity, and identify correlates of the changes in body weight status.
Study Design: Twelve-year retrospective cohort study.
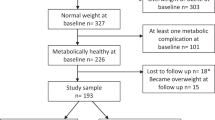
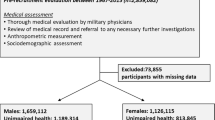
Subjects: A sample of 276 subjects (age 23.9±4.1, 176 males and 100 females) who responded to a questionnaire mailed in 1998 to 1047 children (age 10.6±2.2) treated for obesity at Mie National Hospital in Japan between 1976 and 1992.
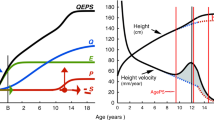
Measurements: Based on height and weight from medical records during childhood, the relative weight (RW; weight expressed as a percentage of the standard body weight for age, height, and sex) was calculated. Degrees of childhood obesity were based on RW: slight obesity (120%≤RW<130%; n=17), moderate obesity (130%≤RW<150%; n=131), and severe obesity (RW≥150%; n=128). Adult body mass index (BMI), which was obtained from the mailed questionnaires, was classified as normal, overweight and obese according to the WHO/NIH criteria. Body weight tracking by degree of obesity was evaluated. Subjects with severe obesity during childhood (n=128) were examined for their weight status in adulthood, prevalence of chronic diseases in adulthood, and factors such as parental obesity, dietary and exercise habits and obesity treatment during childhood.
Results: Childhood obesity tracked into adulthood obesity or overweight in 54.7% of all cases. Severely obese children (36.7%) were more likely to be obese as an adult than moderately obese children (16.8%). The prevalence of adult obesity tended to be greater in boys with moderate childhood obesity than in girls (29.7% in boys vs 14.9% in girls, P=0.058). Among the severely obese children who became normal-weight adults, the prevalence of chronic diseases was about one-fifth of those who remained obese in adulthood (P=0.041). Four factors were associated with changes in body weight status: maternal BMI at entry (P=0.044), the changes in dietary and exercise habits after treatment (P=0.014, P=0.030, respectively), and satisfaction with obesity treatment in childhood (P=0.035).
Conclusions: Severely obese children have a higher risk of becoming obese adults even when they received obesity treatment in childhood. The risk of adulthood obesity was twice as high in moderately obese boys than in girls. On the other hand, many cases of childhood obesity can be corrected with obesity treatment, which in turn can decrease the risk for adult chronic diseases.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Flegal KM . The obesity epidemic in children and adults: current evidence and research issues Med Sci Sports Exerc 1999 31: S509–S514.
Troiano RP, Felgal KM . Overweight children and adolescents: description, epidemiology, and demographics Pediatrics 1998 101: 497–504.
Kotani K, Nishida M, Yamashita S, Funahashi T, Fujioka S, Tokunaga K, Ishikawa K, Tarui S, Matsuzawa Y . Two decades of annual medical examinations in Japanese obese children: do obese children grow into obese adults? Int J Obes Relat Metab Disord 1997 21: 912–921.
Mo-suwan L, Junjana C, Puetpaiboon A . Increasing obesity in school children in a transitional society and the effect of the weight control program Southeast Asian J Trop Med Public Health 1993 24: 590–594.
Ho TF . Eleventh Haridas memorial lecture. Childhood obesity in Singapore primary school children: epidemiological review and anthropometric evaluation J Singapore Paediatr Soc 1985 27: 5–40.
Burton BT, Foster WR, Hirsch J, Van Itallie TB . Health implications of obesity: an NIH Consensus Development Conference Int J Obes 1985 9: 155–170.
NIH Technology Assessment Conference Panel. Methods for voluntary weight loss and control Ann Intern Med 1993 119: 764–770.
Abraham S, Collins G, Nordsieck M . Relationship of childhood weight status to morbidity in adults HSMHA Health Rep 1971 86: 273–284.
Mossberg HO . 40-year follow-up of overweight children Lancet 1989 2: 491–493.
Must A, Jacques PF, Dallal GE, Bajema CJ, Dietz WH . Long-term morbidity and mortality of overweight adolescents. A follow-up of the Harvard Growth Study of 1992 to 1935 New Engl J Med 1992 327: 1350–1355.
Serdula MK, Ivery D, Coates RJ, Freedman DS, Williamson DF, Byers T . Do obese children become obese adults? A review of the literature Prev Med 1993 22: 167–177.
Clarke WR, Lauer RM . Does childhood obesity track into adulthood? Cr Rev Food Sci Nutr 1993 33: 423–430.
Parsons TJ, Power C, Logan S, Summerbell CD . Childhood predictors of adult obesity: a systematic review Int J Obes Relat Metab Disord 1999 23 (Suppl 8): S1–107.
Power C, Lake JK, Cole TJ . Body mass index and height from childhood to adulthood in the 1958 British born cohort Am J Clin Nutr 1997 66: 1094–1101.
Stark O, Atkins E, Wolff OH, Douglas JW . Longitudinal study of obesity in the National Survey of Health and Development Br Med J (Clin Res Edn) 1981 283: 13–17.
DiPietro L, Mossberg HO, Stunkard AJ . A 40-year history of overweight children in Stockholm: life-time overweight, morbidity, and mortality Int J Obes Relat Metab Disord 1994 18: 585–590.
Sungthong R, Mo-suwan L, Chongsuvivatwong V, Junjana C . Secular increases in weight, height and body mass index among school children of Hat Yai, Thailand: a 5 years follow-up study Southeast Asian J Trop Med Public Health 1999 30: 532–538.
Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH . Predicting obesity in young adulthood from childhood and parental obesity New Engl J Med 1997 337: 869–873.
Lake JK, Power C, Cole TJ . Child to adult body mass index in the 1958 British birth cohort: associations with parental obesity Arch Dis Child 1997 77: 376–381.
Twisk JW, Van Mechelen W, Kemper HC, Post GB . The relation between “long-term exposure” to lifestyle during youth and young adulthood and risk factors for cardiovascular disease at adult age J Adolesc Health 1997 20: 309–319.
Epstein LH, Valoski A, Wing RR, McCurley J . Ten-year follow-up of behavioral, family-based treatment for obese children JAMA 1990 264: 2519–2523.
National Institutes of Health and National Heart, Lung, and Blood Institute. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults. The Evidence report Obes Res 1998 6 (Suppl 2).
World Health Organization. Obesity: preventing and managing the global epidemic Report of a WHO consultation on obesity, Geneva, 3–5 June 1997 WHO: Geneva 1998.
Murata M, Kimie Y, Itani A, Inaba M . Standard body weight for age between 5 years and 17 years. (In Japanese.) J Child Health 1980 39: 93–96.
Ministry of Education, Science, Sports and Culture in Japan. Report on School Health Survey 1977.
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH . Establishing a standard definition for child overweight and obesity worldwide: international survey Br Med J 2000 320: 1240–1243.
Katzmarzyk PT, Perusse L, Malina RM, Bouchard C . Seven-year stability of indicators of obesity and adipose tissue distribution in the Canadian population Am J Clin Nutr 1999 69: 1123–1129.
Perusse L, Bouchard C . Role of genetic factors in childhood obesity and in susceptibility to dietary variations Ann Med 1999 31: 19–25.
Matsuura K, Fujimura M, Nozawa Y, Iida Y, Hirayama M . The body shape preferences of Japanese female students Int J Obes Relat Metab Disord 1992 16: 87–93.
Strauss RS . Comparison of measured and self-reported weight and height in a cross-sectional sample of young adolescents Int J Obes Relat Metab Disord 1999 23: 904–908.
Giacchi M, Mattei R, Rossi S . Correction of the self-reported BMI in a teenage population Int J Obes Relat Metab Disord 1998 22: 673–677.
Raitakari OT, Porkka KV, Taimela S, Telama R, Rasanen L, Viikari JS . Effects of persistent physical activity and inactivity on coronary risk factors in children and young adults. The Cardiovascular Risk in Young Finns Study Am J Epidemiol 1994 140: 195–205.
Post GB, Kemper HC, Twisk J, van Mechelen W . The association between dietary patterns and cardiovascular disease risk indicators in healthy youngsters: results covering fifteen years of longitudinal development Eur J Clin Nutr 1997 51: 387–393.
Kemper HC, Post GB, Twisk JW, van Mechelen W . Lifestyle and obesity in adolescence and young adulthood: results from the Amsterdam Growth And Health Longitudinal Study (AGAHLS) Int J Obes Relat Metab Disord 1999 23: S34–S40.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Togashi, K., Masuda, H., Rankinen, T. et al. A 12-year follow-up study of treated obese children in Japan. Int J Obes 26, 770–777 (2002). https://doi.org/10.1038/sj.ijo.0801992
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.0801992
Keywords
This article is cited by
-
The rehabilitation of children and adolescents with severe or medically complicated obesity: an ISPED expert opinion document
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity (2017)
-
High prevalence of overweight and obesity among a representative sample of Puerto Rican children
BMC Public Health (2015)
-
Relationship between obesity and serum reactive oxygen metabolites in adolescents
Environmental Health and Preventive Medicine (2013)
-
Validity of self-reported weight, height and resultant body mass index in Chinese adolescents and factors associated with errors in self-reports
BMC Public Health (2010)