Abstract
As tooth loss is the high end of periodontal problems and edentulous individuals are at higher risk of nutritional problems like obesity, understanding the association between tooth loss and hypertension is important for improving cardiovascular health. We searched for publications from the last two decades using three electronic databases (PubMed, Web of Science and Scopus) and conducted a systematic review and meta-analysis on the association between tooth loss and hypertension according to PRISMA-P guidelines. Quality assessments were performed using the Newcastle–Ottawa Scale and the GRADE approach. Twenty-four studies (20 cross-sectional, and 4 cohort) met the inclusion criteria for this review. Most cross-sectional studies showed that subjects with more tooth loss exhibited a greater proportion of hypertension and higher systolic blood pressure than those with less tooth loss. Meta-analyses revealed a statistically significant association between tooth loss and hypertension. The pooled odds ratios of hypertension for having tooth loss with no tooth loss and for edentulous with dentate were 2.22 (95% CI 2.00–2.45) and 4.94 (95% CI 4.04–6.05), respectively. In cohort studies, subjects with more tooth loss had a greater incidence of hypertension than those with less tooth loss during the follow-up period. The present systematic review and meta-analysis suggests that tooth loss is associated with an increased risk of hypertension and higher systolic blood pressure.
Similar content being viewed by others
Introduction
Background
Hypertension is a medical condition in which blood pressure is chronically 140/90 mmHg or higher1. The worldwide prevalence of hypertension has increased two-fold from 1990 to 2019, to more than 30% for both men and women aged 30–792. Although high blood pressure does not typically cause symptoms, long-term high blood pressure is a major risk factor for coronary artery disease, stroke, heart failure, atrial fibrillation, peripheral arterial disease, vision loss, chronic kidney disease, and dementia3,4,5,6.
Risk factors for hypertension include obesity7, excessive intake of salt8,9, heavy alcohol consumption10,11, insufficient physical activity12,13, psycho-social stress14,15 and smoking16.
Several studies in dentistry have reported that patients with periodontitis have higher blood pressure17,18,19. It is estimated that severe periodontal diseases are prevalent in around 14% of the global adult population, representing more than one billion cases over the world20. Possible mechanisms for the association between periodontitis and hypertension are as follows: (1) periodontitis may elicit vascular inflammation which leads to endothelial dysfunction21; (2) periodontopathogens may stimulate local and systematic host immune responses, resulting in development of atherosclerosis22 and activate endothelial cells23; (3) the production of ROS increases in response to periodontal inflammation; subsequently ROS enter the systemic circulation24.
Tooth loss is the endpoint of progression of periodontitis. Tooth loss results in impaired mastication, which, in turn, makes it difficult to chew hard foods, consequently leads to deteriorated dietary habits25. Decline in masticatory function brings insufficient intake of vegetables and fruit and increased intake of fatty foods, which could cause obesity. The association between impaired mastication including tooth loss and obesity was suggested in a systematic review26. The relationship between obesity and hypertension has been demonstrated. It was reported that about half of new hypertension case attributed to overweight or obesity27. A meta-analysis showed that loss of body weight reduced blood pressure28. Although the impact of tooth loss on hypertension is estimated to be significant, no study has systematically reviewed articles that analyzed this association.
Objective
The aim of this study was to systematically review the relationship between tooth loss/number of teeth and hypertension.
Material and methods
This systematic review was structured following the PRISMA checklist. A protocol to address the a priori research questions, comprehensive literature search with inclusion and exclusion criteria for studies, screening methods, data abstraction, scientific study quality, and data analysis were developed to minimize bias.
Literature search
The PICO model29 was used to select eligible studies in the present systematic review. The inclusion criteria were defined according to the population (P; “human adults”), intervention or exposure (I; “impact of tooth loss on hypertension”), comparison (C; “different number of remaining teeth, different number of missing teeth or dentate and edentulous”), and outcome (O; “hypertension”). The eligibility of the studies was assessed by three independent authors (Akio Tada, Rumi Tano and Hiroko Miura) through screening of titles and abstracts, according to the PICO model. The following PICO question was used: “Does tooth loss/number of teeth associate with hypertension?”. The inclusion criteria were defined as followed: (1) written in English, (2) published between 2001 and 2021, (3) investigating the association between tooth loss/number of teeth and hypertension, (4) conducted on adult subjects (age ≥ 18 years), and (5) using quantitative methods of data collection, were included in this review. The exclusion criteria were defined as followed: (1) subjects received oral and maxillofacial surgery or radiotherapy, (2) descriptive studies, reviews or studies with no analyses investigating the association between tooth loss and hypertension.
A literature search of the PubMed, Web of Science and Scopus databases was performed with relevant keywords (Mesh and non-Mesh). The search terms used were (“tooth loss” OR “number of teeth”) AND (“hypertension” OR “blood pressure”).
Assessment of risk of bias in the included studies
For each selected observational study, the risk of bias was evaluated according to the criteria described by the Newcastle–Ottawa Scale (NOS) for cohort studies. This scale encompasses three domains: selection (four items), comparability (one item), and outcome (three items)30. Cross-sectional studies were graded as follows: very good, 9–10; good, 7–8; satisfactory, 5–6; unsatisfactory, 0–431. Cohort studies were graded as follows: very good, 8–9; good, 7; satisfactory, 5–6; unsatisfactory, 0–432.
The overall quality of evidence was evaluated using the Grading of Recommendation, Assessment, Development and Evaluation (GRADE) framework33. In this review, a narrative GRADE was chosen according to the types of studies included. Certainty of the evidence was evaluated in terms of study design, risk of bias, inconsistency, indirectness, and imprecision parameters, with categorization into one of four ratings: high, moderate, low, and very low34. Evidence issued in this review includes observational data, it started at low quality and then other issues within the magnitude of the effect, inconsistency, indirectness, imprecision, and counteracting plausible residual bias or confounding could be used to downgrade the evidence35. However, the quality of evidence can increase if studies strictly meet one of the following criteria: the magnitude of the treatment effect is very large. There is evidence of a dose–response relationship, or all plausible biases would decrease the magnitude of the treatment effect36.
Data extraction
Data were extracted from each eligible study by three independent authors (Akio Tada, Rumi Tano, and Hiroko Miura) using a specifically developed data extraction sheet. Disagreements were resolved by consensus. The following data were extracted from each eligible study: first author, publication year, setting, type of study, number of subjects, confounding factors (demographic factors, socio-economic factors, health habits including smoking and alcohol consumption, and systemic disease such as diabetes, hypercholesterolemia, and obesity), and outcome measures including both adjusted odds ratios and 95% confidence intervals (CIs).
Statistical analysis
Meta-analyses were conducted using a random-effects model. Studies were excluded if they did not report an outcome in each group or did not have enough information available to calculate the OR. The numbers of subjects according to the status of the remaining teeth and the presence of hypertension were extracted from each study. A separate meta-analysis was performed for each outcome variable. Effect sizes were reported as pooled ORs with 95% CIs for categorical outcomes. The heterogeneity of the effect size estimates across these studies was quantified using the I2 statistic. The I2 statistic ranges from 0 to 100% (I2 < 25%, low heterogeneity; I2 = 25–50%, moderate heterogeneity; and I2 ≥ 50%, substantial heterogeneity)37. All data analyses were performed using STATA version 16.
Results
Literature searches and study characteristics
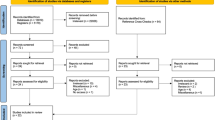
The initial comprehensive literature search identified a total of 294 articles; eligible articles were retrieved through a manual search (Fig. 1). After the removal of duplicates, the titles and abstracts of 233 records were screened. Of these, 194 articles were excluded according to the exclusion criteria written in the “Material and methods”. The remaining 39 articles were screened for further analyses as follows.
Of the 39 potentially relevant articles, 15 were excluded because they did not meet the inclusion criteria. Most of excluded studies did not analyze the association between tooth loss and hypertension. Finally, a total of 24 publications (20 cross-sectional studies38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57, and four cohort studies58,59,60,60) were included in this systematic review, as shown in the flow chart (Fig. 1).
Characteristics of studies are presented in Table 1. Eighteen studies38,41,42,43,44,45,46,48,49,50,52,54,56,57,58,59,60,60 categorized blood pressure into hypertensive and normal according to global criteria62 while six studies39,40,47,51,53,55 used values of systolic blood pressure (SBP) and diastolic blood pressure (DBP) and did not apply these categories. Four studies used self-reported information on hypertensive status42,50,54,60.
In terms of the number of teeth, 14 studies evaluated the number of missing teeth38,39,41,42,43,44,45,47,50,51,55,57,58,59 while 10 studies evaluated the number of remaining teeth40,46,48,49,52,53,54,56,61,60. In the analyses, only four studies used measured values43,44,45,47 while the other 20 categorized measured values. Categorizations were vastly different.
Regarding the age range of subjects, 8 studies included patients < 40 years38,39,42,46,47,48,53,56. Four studies used menopausal women43,45,57,61.
The distribution of countries where the included studies were conducted is as follows: Asia, 12; Central-South America, 5; North America, 4; and Europe 3.
Quality evaluation for each article
The quality of the studies was evaluated using NOS scores (Table 2). Seven studies were classified as “very good”40,45,46,48,55,56,58, 12 as “good”38,39,41,47,48,49,50,51,53,57,61,59, four as “satisfactory”42,43,44,60 and one as “unsatisfactory”54.
Quality evaluation for evidence
The overall certainty of the two pieces of evidence was evaluated using the GRADE system. The certainty of evidences stayed in “Low”, initial rating of observational studies, with no upgrading and downgrading shown as shown in Table 3.
Association between number of remaining/missing teeth and hypertension
The prevalence of hypertension was compared between/among groups with different number of remaining teeth in six cross-sectional studies46,48,49,52,54,56 (Table 1). Four of the six studies showed negatively significant associations between the number of remaining teeth and hypertension after controlling for confounders46,49,52,56. Another study found that the association was slightly below the threshold of statistical significance54. On the other hand, a different study failed to find an association between the number of remaining teeth and hypertension48.
Six cross-sectional studies analyzed the association between number of missing teeth and hypertension38,41,42,43,44,50 (Table 1). Two studies showed that groups with hypertension had higher mean43 or median44 of number of missing teeth than normal blood pressure group. Four of the six studies displayed that positively significant associations after adjusting with confounding factors38,41,45,50. One study showed that menopausal women with hypertension had a higher number of remaining teeth than those without hypertension43. In Dar-Odeh’s study, the association was marginally significant42.
Association between number of remaining/missing teeth and SBP/DBP
Four studies analyzed the associations between number of remaining teeth and SBP/DBP40,52,53,56 (Table 1). Two studies demonstrated that the number of remaining teeth was inversely associated with SBP and DBP even after adjusting for covariates52,53. In Holzke’s study, men with fewer teeth had significantly higher SBP than those with higher teeth was significantly higher, but this association was not observed in women56. Another study showed that the population with a higher number of remaining teeth exhibited a significantly higher SBP than the population with a lower number of remaining teeth, but this association was not observed with DBP40. However, the significance disappeared after adjusting for covariates.
A further six studies analyzed the associations between number of missing teeth and SBP/DBP39,45,47,51,55,57 (Table 1). Two studies reported that populations with a greater number of missing teeth exhibited significantly higher SBP or DBP than those with a smaller number of missing teeth39,51 but this significance disappeared after adjustment for potential confounding factors. On the other hand, two studies found that a population with more missing teeth had significantly higher SBP and DBP than the population with fewer missing teeth after adjusting the confounding factors47,55. In Darnard’s study51, a sub-population with missing teeth > 10 was 1.17 times more likely to have SBP > 140 mmHg than the sub-population with missing teeth ≤10 among adults aged < 65 years. However, this association was not observed among adults aged ≥ 65 years.
Cohort study
Four studies performed cohort study58,59,60 (Table 1). Three studies have compared incidence of hypertension in regard to different number of teeth58,59,60. One study made a comparison between subjects who are edentulous and those who are dentate61. Edentulous participants had a significantly higher risk of incidence of hypertension after adjusting for confounders. Two study analyzed the association between the number of teeth at baseline and the incidence of hypertension during follow-up. A significant higher incidence of hypertension was observed in population with lower number of teeth in one study58 but not in another60 after adjusting for confounders. Kim et al. compared missing teeth between subjects who had hypertension and those who did not at baseline59. In univariate analysis, the hypertension group had a higher risk of tooth loss than the normal group. However, in the multivariable analysis, the opposite result was observed.
Meta-analysis
Separate meta-analyses regarding the risk of hypertension were carried out for “no tooth loss” versus “tooth loss” and for “dentate” versus “edentulous”. Three studies entered in the meta-analysis and found that those with tooth loss have a significantly higher prevalence of hypertension than those with no tooth loss42,46,50. Based on the data of the studies for “no tooth loss” versus “tooth loss”, the pooled summary odds ratio was 2.22 (95% CI 2.00–2.45) in the random-effect model for the group with tooth loss compared to the non-tooth loss group (Fig. 2). In other words, the tooth loss group was 2.22-fold more likely to be diagnosed with hypertension. As for “dentate” versus “edentulous”, two studies found that edentulous subjects had a significantly higher prevalence of hypertension than dentate subjects46,50 and the pooled summary OR was 4.94 (95% CI 4.04–6.05) in the random-effect model for the edentulous group compared to the dentate group (Fig. 3). These findings were statistically significant (p < 0.001). However, the statistical heterogeneity was high across all studies (I2 = 94.8% and 99.1%, respectively).
Discussion
Impact of tooth loss on hypertension
Most of the included studies have demonstrated an association between tooth loss and hypertension with individuals having greater tooth loss exhibiting a higher prevalence of hypertension and higher blood pressure. Only two studies reported no association between tooth loss and hypertension without adjusting for possible confounding factors. Evidence from our literature review suggested that tooth loss is thought to have a significant association with hypertension. However, a few studies reported that this significant association disappeared after adjusting with possible confounding factors and the odds ratios for this association in most studies, which ranges between 1 and 2, are not very large. Therefore, the extent of the association between tooth loss and hypertension may be varied.
There are two possible cascades related to the association between tooth loss and hypertension. It is speculated that progression of periodontitis, a major cause of tooth loss, consequently results in hypertension. The mechanisms by which periodontitis elicits hypertension are complex and not fully elucidated. The major mechanism by which increased blood pressure occurs in patients with periodontitis is likely to be the spread of inflammation and secondary damage to the vascular endothelium63,64,65,66. Periodontal tissue covers a wide area of the oral cavity. The influence of local inflammation of periodontitis occurring in a large proportion of the oral cavity may significantly contribute to systemic inflammation mediated by C-reactive protein and main inflammatory cytokines such as tumor necrosis factor alpha, interleukin 1b and interleukin 667,68. Increases in nitrate-reducing bacteria, which are observed in patients with periodontitis may induce a reduction of nitric oxide, which may consequently lead to an increase in blood pressure69,70,71. It was also reported that an intervention of non-surgical periodontal treatment leads to an improvement of both periodontal status and hypertension72. Another reason is that tooth loss causes a decrease in masticatory function, thereby inducing obesity. There are two possible explanations for the association between mastication and obesity. One is that the eating habits of people with poor masticatory function, and decreased consumption of vegetables and fruits, and higher consumption of high energy food, tend to cause obesity compared to those with adequate mastication73,74,75,76. Another is that a reduction in chewing leads to a decrease in diet-induced thermogenesis and inactivation of neuronal histamine, which may consequently lead to obesity77,78,79.
In patients with metabolic syndrome, other factors, such as diabetes and hyperlipidemia, add to this complex relationship. Obesity is one of the causes of diabetes80 and diabetes and periodontitis have a bidirectional relationship81. In some of the studies reviewed in this article, the association between tooth loss and hypertension disappeared after adjustment for confounders (demographic factors, socio-economic factors, health behavior and general health). This suggests that other factors have a considerable influence on this association. It is thought that various factors interact with each other in a complicated cascade from tooth loss to hypertension.
This systematic review aimed to analyze the association between tooth loss and hypertension by systematically summarizing the scientific evidence from clinical studies during the last two decades. Twenty-four studies were included, with a total of 772,683 adults. To the best of our knowledge, this is the first systematic literature review to examine this association. The results of this review may help elucidate the influence of oral health on blood pressure.
Comparison of the association between tooth loss and hypertension
The association between tooth loss and hypertension was compared for each geographical location. Studies conducted in Central-South America showed a trend for weaker association compared to other areas; one with no association48, one with approaching significance level (p = 0.067)54, and one with disappearance of significance after adjustment with confounders40 in 5 studies. The reason for the difference is unclear. In Central-South America studies, studies from this region showed higher tooth loss than those from other areas’ studies, particularly developed countries. Tooth loss in younger people may not cause hypertension easily. More detailed analysis is needed.
There was a difference in the association between tooth loss and hypertension between men and women. For women, the association between tooth loss and hypertension was marginally or not observed in studies including younger subjects (19–39 years)42,56. On the other hand, significant associations were found in studies with subjects aged 40 or older years after adjusting confounders44,47,49,59. It is thought that younger subjects with tooth loss may have smaller prevalence of hypertension than older subjects with tooth loss. However, in the Völzke’s study including individuals aged 20–79 years, the significant association was found among men unlike among women56. In a Korean study, men aged 40 and older did not show the significant association unlike women49. Various factors may influence this association.
Difference in the association with hypertension between SBP and DBP
Although a significant association between SBP and tooth loss was observed, the association between DBP and tooth loss was not significant. The reasons why SBP exhibits a stronger association with tooth loss than DBP is unclear. The proportion of individuals with diastolic hypertension (systolic–diastolic hypertension [SDH] or isolated diastolic hypertension [IDH]) decreased, while that of those with systolic hypertension increased with age. Accumulation of advanced glycation end products (AGE) with aging leads to increased arterial stiffness and contributes to the development of isolated systolic hypertension82,83. Excessive intake of animal-derived foods which are rich in fat and AGE may increase the risk of hypertension and other chronic disease84,85,86,87. In general, since individuals who suffer from decreased masticatory function due to tooth loss tend to eat foods that are high in fat88,89,90,91, this may induce AGE accumulation, consequently contribution to increased SBP.
Cohort studies
Two prospective cohort studies demonstrated an increased incidence of hypertension in individuals with more tooth loss during the observation period58,61. On the contrary, one study reported that subjects with hypertension experienced lower tooth loss than those without hypertension59. Therefore, the association between tooth loss and hypertension may not be bidirectional. In other words, hypertension may not cause tooth loss.
Quality of studies
Of the 24 included studies, 16 (66.7%) adjusted the association between blood pressure and tooth loss with all possible confounding factors39,40,41,45,46,47,48,49,50,53,55,56,58,59,60,60. Of the remaining eight studies, 4 studies lacked adjustment for only one confounding facto38,42,51,52. The most important confounding factor was obesity, and almost all studies adjusted for this. These adjustments strengthen the reliability of the evidence obtained in this review. However, three studies that investigated patients from university hospitals failed to adjust for socio-economic factors38,42,51. The characteristics of these studies’ settings might make it difficult to obtain data of socio-economic factors.
Eight studies employed self-reported data on the number of teeth and/or hypertension. Some studies have shown strong validity of self-reported number of tooth loss in high-income countries88,89. One study examined in health professionals in the US, expecting high validity against clinically measured results60. However, the validity of the self-reported number of lost teeth has not been evaluated in lower and middle-income countries. Moreover, the validity of self-reported hypertension in developing countries is not high90,91. Since most of the studies that employed self-reported data on the number of teeth and/or hypertension in this review were performed in developing countries, self-reported data may deviate from true values. Since subjective measurements have the possibility to give considerable optimistic results compared with practitioners’ measurements92, self-reported data may often be underestimated.
Strengths and limitations
There are several limitations in this study. First, all studies included in this review were observational studies. Intervention studies are necessary to analyze the causal relationships.
Second, the grouping of participants according to the number of teeth differed among the studies. Due to this problem, only small-scale meta-analyses were performed. Moreover, the only meta-analyses that were carried out were to compare the hypertension rate for tooth loss vs. no tooth loss and for dentate vs. edentulous. Pooled odds ratio data based on a cut-off value for the number of teeth is valuable for estimating the association between the number of remaining teeth and hypertension. Moreover, it may be a rough indication for maintaining oral health to prevent hypertension.
Third, some studies could not be included in meta-analysis because of lack of data for real number of subjects by tooth loss and hypertension. This lack lowers the value of results of meta-analysis. Nonetheless, odds ratios for the association between tooth loss and hypertension of these studies are similar to those of studies included meta-analysis. It is thought that missing of these data would give little influence on pooled ORs.
Forth, several studies have investigated many specialized subjects, including patients from clinics or hospitals38,39,42,44,54, menopausal women43,45,57,61, and male health care specialists60. Although it is problematic to apply the results of these studies to the general population, the large number of subjects in their studies increases the reliability of the study results.
The strength of our study is that it included many studies with a large number of subjects. Eleven of the 24 included studies have investigated large-scale community dwellings of > 1000 individuals40,41,46,49,50,52,53,55,56,58,59, which enhances the credibility of the results of the studies. The greater the sample size, the smaller the error, which makes the results more reliable.
Future direction
Although lost teeth cannot be regenerated, they can be restored by prosthetics. Provision of prosthetics can improve both masticatory function and diet. When decreased mastication elicits obesity and subsequently hypertension, the provision of prosthetics may improve increased blood hypertension. The number of teeth acts only as an anatomical indicator. There is an indicator, functional teeth that is the sum of the number of natural teeth and the number of lost teeth that are restored by prosthetics. It is of interest to investigate the association between the number of functional teeth and hypertension.
The lack of standardized division criteria for tooth loss makes it impossible to compare the strength of associations between tooth loss and hypertension observed in reviewed studies. The unification of division standards for tooth loss should be proposed.
Conclusion
In the present review, we provided an overview and appraisal of studies regarding the relationship between the number of teeth/tooth loss and hypertension. People with fewer remaining teeth or more tooth loss exhibited a higher prevalence of hypertension. Those with more tooth loss had significantly higher SBP but not DBP than those with less tooth loss. Those with more tooth loss showed a higher incidence of hypertension than those with less tooth loss during the observation period (Supplementary Information).
Data availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Naish, J. & Court, D. S. Medical Sciences (2 ed.). p. 562. ISBN 9780702052491 (2014).
NCD Risc Factor Collaboration. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: A pooled analysis of 1201 population-representative studies with 104 million participants. Lancet https://doi.org/10.1016/S0140-6736(21)01330-1 (2021).
Lackland, D. T. & Weber, M. A. Global burden of cardiovascular disease and stroke: Hypertension at the core. Can. J. Cardiol. 31, 569–571. https://doi.org/10.1016/j.cjca.2015.01.009 (2015).
Mendis, S., Puska, P. & Norrving, B. Global Atlas on Cardiovascular Disease Prevention and Control (PDF) 1st edn, 38 (World Health Organization in collaboration with the World Heart Federation and the World Stroke Organization, 2011).
Hernandorena, I., Duron, E., Vidal, J. S. & Hanon, O. Treatment options and considerations for hypertensive patients to prevent dementia. Expert Opin. Pharmacother. 18, 989–1000. https://doi.org/10.1080/14656566.2017.1333599 (2017).
Lau, D. H., Nattel, S., Kalman, J. M. & Sanders, P. Modifiable risk factors and atrial fibrillation. Circulation 136, 583–596 (2017).
Aronow, W. S. Association of obesity with hypertension. Ann. Transl. Med. 5, 350. https://doi.org/10.21037/atm.2017.06.69 (2017).
Grillo, A. et al. Salt recuction to prebent hypertension and cardiovascular disease. JACC State Art Rev. 11, 2019. https://doi.org/10.3390/nu11091970 (1970).
He, F. J., Tan, M., Ma, Y. & MacGregor, G. A. Systematic review of the effect of daily alcohol intake on blood pressure. J. Am. Coll. Cardiol. 75, 632–647. https://doi.org/10.1016/j.jacc.2019.11.055 (2020).
McFadden, C. B., Brensinger, C. M., Berlin, J. A. & Townsend, R. R. Alcohol consumption and the risk of hypertension in women and men. Am. J. Hypertens. 18, 276–286. https://doi.org/10.1016/j.amjhyper.2004.07.020 (2005).
Sesso, H. D., Cook, N. R., Buring, J. E., Manson, J. E. & Gaziano, J. M. Alcohol consumption and the risk of hypertension in women and men. Hypertension 51, 1080–1087. https://doi.org/10.1161/HYPERTENSIONAHA.107.104968 (2008) (Epub 2008 Feb 7).
Egan, B. M. Physical activity and hypertension: Knowing is not enough; we must apply. Willing is not enough. We must do-von Goethe. Hypertension 69, 404–406. https://doi.org/10.1161/HYPERTENSIONAHA.116.08508 (2017).
Börjesson, M., Onerup, A., Lundqvist, S. & Dahlöf, B. Physical activity and exercise lower blood pressure in individuals with hypertension: Narrative review of 27 RCTs. Br. J. Sports Med. 50, 356–361. https://doi.org/10.1136/bjsports-2015-095786 (2016) (Epub 2016 Jan 19).
Liu, M. Y., Li, N., Li, W. A. & Khan, H. Association between psychosocial stress and hypertension: A systematic review and meta-analysis. Neurol. Res. 39, 573–580. https://doi.org/10.1080/01616412.2017.1317904 (2017).
Sparrenberger, F. et al. Does psychosocial stress cause hypertension? A systematic review of observational studies. J. Hum. Hypertens. 23, 12–19. https://doi.org/10.1038/jhh.2008.74 (2009).
Virdis, A., Giannarelli, C., Fritsch Neves, M., Taddei, S. & Ghiadoni, L. Cigarette smoking and hypertension. Curr. Pharm. Des. 16, 2518–2525 (2010).
Lanau, N., Mareque-Bueno, J. & Zabalza, M. Does periodontal treatment help in arterial hypertension control? A systematic review of literature. Eur. J. Dent. 15, 168–173. https://doi.org/10.1055/s-0040-1718244 (2021) (Epub 2020 Oct 8).
MuñozAguilera, E. et al. Periodontitis is associated with hypertension: A systematic review and meta-analysis. Cardiovasc. Res. 116, 28–39. https://doi.org/10.1093/cvr/cvz201 (2020).
Martin-Cabezas, R. et al. Association between periotontitis and arterial hypertension: A systematic review and meta-analysis. Am. Heart. J. 180, 98–112. https://doi.org/10.1016/j.ahj.2016.07.018 (2016) (Epub 2016 Aug 8).
Global Burden of Disease Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019). Seattle: Institute of Health Metrics and Evaluation (IHME); 2020. http://ghdx.healthdata.org/gbd-results-tool.
Amar, S. et al. Periodontal disease is associated with brachial artery endothelial dysfunction and systemic inflammation. Arterioscler. Thromb. Vasc. Biol. 23, 1245–1249 (2003).
Zou, Y. et al. Periodontopathic microbiota and atherosclerosis: Roles of TLR-mediated inflammation response. Oxid. Med. Cell Longev. 2022, 9611362. https://doi.org/10.1155/2022/9611362 (2022).
Assinger, A. et al. Periodontopathogens induce soluble P-selectin release by endothelial cells and platelets. Thromb. Res. 127, e20–e26 (2011).
Sobaniec, H. & Sobaniec-Lotowska, M. E. Morphological examinations of hard tissues of paradontium and evaluation of selected processes of lipid peroxidation in blood serum of rats in the course of experimental periodontitis. Med. Sci. Monit. 6, 875–881 (2000).
Iwasaki, M. et al. Association between dental status and food diversity among older Japanese. Connunity Dent. Health 32, 104–110 (2015).
Tada, A. & Miura, H. Association of mastication and factors affecting masticatory function with obesity in adults: A systematic review. BMC Oral Health 18, 76. https://doi.org/10.1186/s12903-018-0525-3 (2018).
Forman, J. P., Stampfer, M. J. & Curhan, G. C. Diet and lifestyle risk factors associated with incident hypertension in women. JAMA 302, 401–411. https://doi.org/10.1001/jama.2009.1060 (2009).
Mulrow, X. et al. Dieting to reduce body weight for controlling hypertension in adults. Cochrane Database Syst Rev. 2, CD000484 (2000).
Liberati, A. et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. J. Clin. Epidemiol. 2009(62), e1-34. https://doi.org/10.1016/j.jclinepi.2009.06.006 (2009).
Wells, G. A. et al. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Nonrandom-Ised Studies in Meta-Analyses (Ottawa Hospital Research Institute, 2000).
Modesti, P. A. et al. Panethnic differences in blood pressure in Europe: A systematic review and meta-analysis. PLoS One 11, e0147601. https://doi.org/10.1371/journal.pone.0147601 (2016).
Ortolan, A. et al. The genetic contribution to drug response in spondyloarthritis: A systematic literature review. Front. Genet. 20(12), 703911. https://doi.org/10.3389/fgene.2021.703911 (2021).
Ryan, R. How to GRADE the Quality of the Evidence. Version 3.0. (Cochrane Consumers and Communication Group, 2016).
Schünemann, H., Hill, S., Guyatt, G., Akl, E. A. & Ahmed, F. The GRADE approach and Bradford Hill’s criteria for causation. J. Epidemiol. Comm. Health 65, 392–395. https://doi.org/10.1136/jech.2010.119933 (2011).
Movsisyan, A. Applying GRADE in systematic reviews of complex interventions: Challenges and considerations for a new guidance (PhD thesis) (University of Oxford Wolfson College, 2018)
Guyatt, G. H. et al. GRADE guidelines: 9 Rating up the quality of evidence. J. Clin. Epidemiol. 64, 1311–1316. https://doi.org/10.1016/j.jclinepi.2011.06.004 (2011).
Higgins, J. P., Thompson, S. G., Deeks, J. J. & Altman, D. G. Measuring inconsistency in meta-analyses. BMJ 327, 557–560 (2003).
Mendes, J. J. et al. Blood pressure and tooth loss: A large cross-sectional study with age mediation analysis. Int. J. Environ. Res. Public Health 8, 285. https://doi.org/10.3390/ijerph18010285 (2021).
Hosadurga, R., Kyaw Soe, H. H., Peck Lim, A. T., Adl, A. & Mathew, M. Association between tooth loss and hypertension: A cross-sectional study. J. Family Med. Prim. Care 9, 925–932. https://doi.org/10.4103/jfmpc.jfmpc_811_19 (2020) (eCollection 2020 Feb).
Brutto, D. et al. Association between pulsatile components of blood pressure and severe tooth loss in rural Ecuador: The three villages study. J. Prim. Care Community Health 11, 2150132720928670. https://doi.org/10.1177/2150132720928670 (2020).
Da, D. et al. Shanghai Aging Study. Association between tooth loss and hypertension among older Chinese adults: A community-based study. BMC Oral Health 19, 277. https://doi.org/10.1186/s12903-019-0966-3 (2019).
Dar-Odeh, N. et al. Association of dental caries, retained roots, and missing teeth with physical status, diabetes mellitus and hypertension in women of the reproductive age. Int. J. Environ. Res. Public Health 16, 2565. https://doi.org/10.3390/ijerph16142565 (2019).
Al-Ahmad, B. E. M., Kashmoola, M. A., Mustafa, N. S., Hassan, H. & Arzmi, M. H. The relationship between tooth loss, body mass index, and hypertension in postmenopausal female. Eur J Dent. 12, 120–122. https://doi.org/10.4103/ejd.ejd_322_17 (2018).
Delgado-Pérez, V. J. et al. Diabetes or hypertension as risk indicators for missing teeth experience: An exploratory study in a sample of Mexican adults. Niger. J. Clin. Pract. 20, 1335–1341. https://doi.org/10.4103/njcp.njcp_52_17 (2017).
Gordon, J. H. et al. Association of clinical measures of periodontal disease with blood pressure and hypertension among postmenopausal women. J. Periodontol. 89, 1193–1202. https://doi.org/10.1002/JPER.17-0562 (2018).
Shin, H. S. Association between the number of teeth and hypertension in a study based on 13,561 participants. J. Periodontol. 89, 397–406. https://doi.org/10.1002/JPER.17-0413 (2018).
Moghadam, S. A., Fakour, S. R., Moghaddam, A. A. & Abdollahi, Z. A relationship between tooth loss and periodontal disease with increased blood pressure in adults: A population-based study in Iran. Res. J. Pharm. Biol. Chem. Sci. 7, 34–41 (2016).
Laguzzi, P. N. et al. Tooth loss and associated factors in elders: Results from a national survey in Uruguay. J. Public Health Dent. 76, 143–151. https://doi.org/10.1111/jphd.12123 (2016) (Epub 2015 Oct 14).
Kim, S. W. et al. Tooth loss and metabolic syndrome in South Korea: The 2012 Korean National Health and Nutrition Examination Survey. Medicine (Baltimore) 95, e3331. https://doi.org/10.1097/MD.0000000000003331 (2016).
Singh, A. et al. Association between tooth loss and hypertension among a primarily rural middle aged and older Indian adult population. J. Public Health Dent. 76, 198–205. https://doi.org/10.1111/jphd.12136 (2016) (Epub 2015 Nov 24).
Darnaud, C., Thomas, F., Pannier, B., Danchin, N. & Bouchard, P. Oral health and blood pressure: The IPC cohort. Am. J. Hypertens. 28, 1257–1261. https://doi.org/10.1093/ajh/hpv025 (2015) (Epub 2015 Mar 16).
Zhu, Y. & Hollis, J. H. Associations between the number of natural teeth and metabolic syndrome in adults. J. Clin. Periodontol. 42, 113–120. https://doi.org/10.1111/jcpe.12361 (2015) (Epub 2015 Jan 29).
Peres, M. A., Tsakos, G., Barbato, P. R., Silva, D. A. & Peres, K. G. Tooth loss is associated with increased blood pressure in adults—a multidisciplinary population-based study. J. Clin. Periodontol. 39, 824–833. https://doi.org/10.1111/j.1600-051X.2012.01916.x (2012) (Epub 2012 Jun 26).
Islas-Granillo, H. et al. Edentulism risk indicators among Mexican elders 60-year-old and older. Arch. Gerontol. Geriatr. 53, 258–262. https://doi.org/10.1016/j.archger.2010.12.014 (2011) (Epub 2011 Jan 15).
Lee, H. K. et al. More missing teeth are associated with poorer general health in the rural Korean elderly Arch. Gerontol. Geriatr. 50, 30–33. https://doi.org/10.1016/j.archger.2009.01.005 (2010) (Epub 2009 Feb 23).
Völzke, H. et al. Gender differences in the relation between number of teeth and systolic blood pressure. J. Hypertens. 24(7), 1257–1263. https://doi.org/10.1097/01.hjh.0000234104.15992.df (2006).
Taguchi, A. et al. Tooth loss is associated with an increased risk of hypertension in postmenopausal women. Hypertension 43, 1297–1300. https://doi.org/10.1161/01.HYP.0000128335.45571.ce (2004) (Epub 2004 Apr 26).
Woo, H. G., Chang, Y., Lee, J. S. & Song, T. J. Tooth loss is associated with an increased risk of hypertension: A nationwide population-based cohort study. PLoS One 16(6), e0253257. https://doi.org/10.1371/journal.pone.0253257 (2021).
Kim, Y. T., Choi, J. K., Kim, D. H., Jeong, S. N. & Lee, J. H. Association between health status and tooth loss in Korean adults: Longitudinal results from the National Health Insurance Service-Health Examinee Cohort, 2002–2015. J. Periodontal. Implant. Sci. 49, 158–170. https://doi.org/10.5051/jpis.2019.49.3.158 (2013) (eCollection).
Rivas-Tumanyan, S., Spiegelman, D., Curhan, G. C., Forman, J. P. & Joshipura, K. J. Periodontal disease and incidence of hypertension in the health professionals follow-up study. Am. J. Hypertens. 25, 770–776. https://doi.org/10.1038/ajh.2012.32 (2012) (Epub 2012 Apr 5).
Gordon, J. H. et al. Association of periodontal disease and edentulism with hypertension risk in postmenopausal women. Am. J. Hypertens. 32, 193–201. https://doi.org/10.1093/ajh/hpy164 (2019).
National High Blood Pressure Education Program The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and treatment of High Blood Pressure. Bethesda (MD) National Heart lung, and Blood Institute (US) (2004).
Tsioufis, C., Kasiakogias, A., Thomopoluos, C. & Stefanadis, C. Periodontitis and blood pressure: The concept of dental hypertension. Atherosclerosis 219, 1–9 (2022).
Leong, X., Ng, C., Badiah, B. & Das, S. Association between hypertension and periodontitis: Possible mechanisms. Sci. World J. 2014, 768237 (2014).
Ciulla, M. & Vivona, P. Is there an association between periodontitis and arterial hypertension?. Ital. J. Dent. Med. 5, 17–19 (2020).
Paizan, M. & Vilela-Martin, J. Is there an association between periodontitis and hypertension?. Curr. Cardiol. Rev. 10, 355–361 (2014).
Pinto, D. et al. Periodontitis and hypertension: Is the association causal?. High. Blood Press. Cardiovasc. Prev. 27, 281–289 (2020).
Garlet, G. P. Destructive and protective roles of cytokines in periodontitis: A re-appraisal from host defense and tissue destruction viewpoints. J. Dent. Res. 89, 1349–1363 (2010).
Pignatelli, P., Fabietti, B., Ricci, A., Piattellim, A. & Curia, M. How periodontal disease and presence of nitric oxide reducing oral bacteria can affect blood pressure. Int. J. Mol. Sci. 21, 7538 (2020).
Bryan, N., Tribble, G. & Angelov, N. Oral microbiome and nitric oxide: The missing link in the management of blood pressure. Curr. Hypertens. Rep. 19, 33 (2017).
Alzahrani, H. S., Jackson, K. G., Hobbs, D. A. & Lovegrove, J. A. The role of dietary nitrate and the oral microbiome on blood pressure and vascular tone. Nutr. Res. Rev. 20, 1–18. https://doi.org/10.1017/S0954422420000281 (2020).
Czesnikiewicz-Guzik, M. et al. Causal association between periodontitis and hypertension: Evidence from Mendelian randomization and a randomized controlled trial of non-surgical periodontal therapy. Eur. Heart J. 40, 3459–3470 (2019).
Tada, A. & Miura, H. Systematic review of the association of mastication with food and nutrient intake in the independent elderly. Arch. Gerontol. Geriatr. 59, 497–505 (2014).
Tsai, A. C. & Chang, T. L. Association of dental prosthetic condition with food consumption and the risk of malnutrition and follow-up 4-year mortality risk in elderly Taiwanese. J. Nutr. Health Aging 15, 265–270 (2011).
Yoshida, M. et al. Correlation between dental and nutritional status in community-dwelling elderly Japanese. Geriatr. Gerontol. Int. 11, 315–319 (2011).
Lee, J. S. et al. Edentulism and nutritional status in a biracial sample of well-functioning, community-dwelling elderly: The health, aging, and body composition study. Am. J. Clin. Nutr. 79, 295–302 (2004).
Hamada, Y., Kashima, H. & Hayashi, N. The number of chews and meal duration affect diet-induced thermogenesis and splanchnic circulation. Obesity (Silver Spring) 22, E62-69. https://doi.org/10.1002/oby.20715 (2014).
Morton, G. J., Cummings, D. E., Baskin, D. G., Barsh, G. S. & Schwartz, M. W. Central nervous system control of food intake and body weight. Nature 443, 289–295 (2006).
Sakata, T., Yoshimatsu, H. & Kurokawa, M. Hypothalamic neuronal histamine: Implications of its homeostatic control of energy metabolism. Nutrition 13, 403–411 (1997).
Kahn, S. E., Hull, R. L. & Utzschneider, K. M. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature 444, 840–846 (2006).
Stöhr, J., Barbaresko, J., Neuenschwander, M. & Schlesinger, S. Bidirectional association between periodontal disease and diabetes mellitus: A systematic review and meta-analysis of cohort studies. Sci Rep. 11, 13686. https://doi.org/10.1038/s41598-021-93062-6 (2021).
Franklin, S. S. et al. Hemodynamic patterns of age-related changes in blood pressure. Circulation 796, 308–315 (1997).
Vlassara, H. & Palace, M. R. Glycoxidation: The menace of diabetes and aging. Mt. Sinai J. Med. 70, 232–241 (2003).
Diekmann, F. et al. Soluble Receptor for Advanced Glycation End Products (sRAGE) is a sensitive biomarker in human pulmonary arterial hypertension. Int. J. Mol. Sci. 22, 8591. https://doi.org/10.3390/ijms22168591 (2021).
Garay-Sevilla, M. E., Rojas, A., Portero-Otin, M. & Uribarri, J. Dietary AGEs as exogenous Boosters of inflammation. J. Nutr. 13, 2802. https://doi.org/10.3390/nu13082802 (2021).
Velichkova, S., Foubert, K. & Pieters, L. Natural products as a source of inspiration for novel inhibitors or advanced glycation endoproducts (AGEs) formation. Planta Med. 87, 780–801. https://doi.org/10.1055/a-1527-7611 (2021) (Epub 2021 Aug 2).
Kuzan, A. Toxicity of advanced glycation end products (Review). Biomed. Rep. 14, 46. https://doi.org/10.3892/br.2021.1422 (2021) (Epub 2021 Mar 18).
Pitiphat, W., Garcia, R. I., Douglass, C. W. & Joshipura, K. J. Validation of self-reported oral health measures. J. Public Health Dent. 62, 122–128. https://doi.org/10.1111/j.1752-7325.2002.tb03432.x (2002).
Gilbert, G. H., Chavers, L. S. & Shelton, B. J. Comparison of two methods of estimating 48-month tooth loss incidence. J. Public Health Dent. 62, 163–169. https://doi.org/10.1111/j.1752-7325.2002.tb03438.x (2002).
Najafi, F., Moradinazar, M., Hamzeh, B. & Rezaeian, S. The reliability of self-reporting chronic diseases: How reliable is the result of population-based cohort studies. J. Prev. Med. Hyg. 60, E349–E353. https://doi.org/10.15167/2421-4248/jpmh2019.60.4.1118 (2019) (eCollection 2019 Dec).
Onue, I. & Velamuri, M. The gap between self-reported and objective measures of disease status in India. PLoS One 13, e0202786. https://doi.org/10.1371/journal.pone.0202786 (2018) (eCollection).
Slagter, A. P., Olthoff, L. W., Bosman, F. & Steen, W. H. Masticatory ability, denture quality, and oral conditions in edentulous subjects. J. Prosthet. Dent. 68, 299–307 (1992).
Acknowledgements
We would like to thank Editage (www.editage.jp) for English language editing.
Author information
Authors and Affiliations
Contributions
Authors A.T., R.T. and H.M. contributed to the conception, design of the study, acquisition of data, interpretation of data, and manuscript revisions. A.T. contributed to the writing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tada, A., Tano, R. & Miura, H. The relationship between tooth loss and hypertension: a systematic review and meta-analysis. Sci Rep 12, 13311 (2022). https://doi.org/10.1038/s41598-022-17363-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-17363-0
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.