Abstract
Background
There have been conflicting reports regarding the case-fatality outcomes associated with sepsis and septic shock in patients with severe mental illness (SMI).
Methods
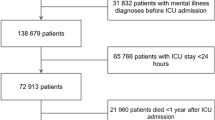
We searched Medline®, Web of Science® and the Cochrane Library® databases (from inception to 4-July-2023) for papers reporting outcomes associated with sepsis and septic shock in adult with (cases) vs. without SMI (controls). The main study outcome was the unadjusted case-fatality rate at hospital discharge, or 30 days if unavailable. Secondary outcomes included the rates of adjusted case-fatality at hospital discharge.
Results
A total of six studies were included in the systematic review, of which four provided data for meta-analysis involving 2,124,072 patients. Compared to controls, patients with SMI were younger and more frequently women. Unadjusted analyses showed that SMI patients had a lower case-fatality rate associated with sepsis and septic shock than their non-SMI counterparts (OR 0.61, 95% CI [0.58–0.65], PI 95% CI [0.49–0.77], I2 = 91%). Meta-regression and subgroup analyses showed that the denominator of the study population (i.e. septic shock or sepsis) was associated with the outcome with an R2 of 59.7%.
Conclusion
In conclusion, our study reveals a survival advantage of SMI patients over their non-SMI counterparts. Further research is needed to fully elucidate the mechanisms involved and to develop targeted interventions that can improve the prognosis of both SMI and non-SMI patients facing sepsis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout





Similar content being viewed by others
Data availability
Data is available in the literature corpus and can be find using the search strategy defined in the manuscript.
References
Lakbar I, Leone M, Pauly V, Orleans V, Srougbo K, Diao S, et al. Association of severe mental illness and septic shock case fatality rate in patients admitted to the intensive care unit: A national population-based cohort study. PLOS Med. 2023;20:e1004202.
Leone M, Lakbar I, Vincent J-L. Sepsis: Actual numbers and uncertainties. Revue d’Épidémiologie. et de Sté Publique. 2023;71:102176.
Ishida T, Nakamura K, Miyazaki K, Yukawa T, Yamagishi T, Sugiyama K, et al. Mortality from sepsis among patients with schizophrenia and mood disorders in an intensive care unit: A chart review. Psychiatry Res. 2019;279:372–3.
Soubani AO, Sharma A, Soubani O, Mishra T. Septic Shock Short-Term Outcomes in Hospitalized Patients With Major Psychiatric Disorders: Analysis From the National Inpatient Sample Database. J Acad Consult Liaison Psychiatry. 2023. https://doi.org/10.1016/j.jaclp.2023.03.003.
Nilsson NH, Bendix M, Öhlund L, Widerström M, Werneke U, Maripuu M. Increased Risks of Death and Hospitalization in Influenza/Pneumonia and Sepsis for Individuals Affected by Psychotic Disorders, Bipolar Disorders, and Single Manic Episodes: A Retrospective Cross-Sectional Study. J Clin Med. 2021;10:4411.
Fond G, Pauly V, Bege T, Orleans V, Braunstein D, Leone M, et al. Trauma-related mortality of patients with severe psychiatric disorders: population-based study from the French national hospital database. Br J Psychiatry. 2020;217:568–74.
Fond G, Pauly V, Leone M, Llorca P-M, Orleans V, Loundou A, et al. Disparities in Intensive Care Unit Admission and Mortality Among Patients With Schizophrenia and COVID-19: A National Cohort Study. Schizophr Bull. 2021;47:624–34.
Fond G, Pauly V, Leone M, Orleans V, Garosi A, Lancon C, et al. Mortality among inpatients with bipolar disorders and COVID-19: a propensity score matching analysis in a national French cohort study. Psychol Med. 2023;53:1979–88.
Davydow DS, Ribe AR, Pedersen HS, Vestergaard M, Fenger-Grøn M. The association of unipolar depression with thirty-day mortality after hospitalization for infection: A population-based cohort study in Denmark. J Psychosom Res. 2016;89:32–38.
Correll CU, Solmi M, Croatto G, Schneider LK, Rohani‐Montez SC, Fairley L, et al. Mortality in people with schizophrenia: a systematic review and meta‐analysis of relative risk and aggravating or attenuating factors. World Psychiatry. 2022;21:248–71.
Solmi M, Fiedorowicz J, Poddighe L, Delogu M, Miola A, Høye A, et al. Disparities in Screening and Treatment of Cardiovascular Diseases in Patients With Mental Disorders Across the World: Systematic Review and Meta-Analysis of 47 Observational Studies. AJP. 2021;178:793–803.
PRISMA-P Group, Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2014. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 13 November 2023.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336:924–6.
Higgins J, Deeks J. Chapter 6: Choosing effect measures and computing estimates of effect. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. editors. Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021), Cochrane. 2021. Available from www.training.cochrane.org/handbook.
Deeks J, Higgins J, Altman D. Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. editors. Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021), Cochrane. 2021. Available from www.training.cochrane.org/handbook.
Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Introduction to Meta-Analysis. vol. 77. Chichester, UK: John Wiley&Sons; 2011.
Rücker G, Schwarzer G, Carpenter J. Arcsine test for publication bias in meta-analyses with binary outcomes. Stat Med. 2008;27:746–63.
Peters JL. Comparison of Two Methods to Detect Publication Bias in Meta-analysis. JAMA. 2006;295:676.
Harbord RM, Egger M, Sterne JAC. A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Stat Med. 2006;25:3443–57.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Sterne JAC, Sutton AJ, Ioannidis JPA, Terrin N, Jones DR, Lau J, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002–d4002.
Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22:153–60.
Oud L, Garza J. Impact of history of mental disorders on short-term mortality among hospitalized patients with sepsis: A population-based cohort study. PLoS One. 2022;17:e0265240.
Arsenović S, Trajković G, Pekmezović T, Gazibara T. Association of health literacy with physical and mental health in people with chronic diseases. Rev Epidemiol Sante Publique. 2023;71:101419.
Salmi L-R, Saillour-Glénisson F, Alla F, Boussat B. Evaluation and research on public health interventions. Rev Epidemiol Sante Publique. 2023;71:101836.
Bonkat N, Fellendorf FT, Dalkner N, Reininghaus EZ. Severe mental disorders and vaccinations – a systematic review. World J Biol Psychiatry. 2022;23:501–16.
Steiner J, Jacobs R, Panteli B, Brauner M, Schiltz K, Bahn S, et al. Acute schizophrenia is accompanied by reduced T cell and increased B cell immunity. Eur Arch Psychiatry Clin Neurosci. 2010;260:509–18.
Tynan RJ, Weidenhofer J, Hinwood M, Cairns MJ, Day TA, Walker FR. A comparative examination of the anti-inflammatory effects of SSRI and SNRI antidepressants on LPS stimulated microglia. Brain Behav Immun. 2012;26:469–79.
Goldsmith DR, Rapaport MH, Miller BJ. A meta-analysis of blood cytokine network alterations in psychiatric patients: comparisons between schizophrenia, bipolar disorder and depression. Mol Psychiatry. 2016;21:1696–709.
Sheth PM, Douchant K, Uyanwune Y, Larocque M, Anantharajah A, Borgundvaag E, et al. Evidence of transmission of Clostridium difficile in asymptomatic patients following admission screening in a tertiary care hospital. PLOS One. 2019;14:e0207138.
Landén M, Larsson H, Lichtenstein P, Westin J, Song J. Respiratory infections during lithium and valproate medication: a within-individual prospective study of 50,000 patients with bipolar disorder. Int J Bipolar Disord. 2021;9:4.
Hoertel N, Sánchez-Rico M, Vernet R, Beeker N, Jannot A-S, Neuraz A, et al. Association between antidepressant use and reduced risk of intubation or death in hospitalized patients with COVID-19: results from an observational study. Mol Psychiatry. 2021;26:5199–212.
Funding
The GERAR (Groupe Education Recherche en Anesthesie Reanimation) funded the use of the Covidence software.
Author information
Authors and Affiliations
Contributions
Conceptualization, ML, GF, LB, IL ; methodology, ML, GF, LB, IL.; software, IL, LD; validation, ML, GF, LB, IL; formal analysis, IL, LD; investigation, IL, EM; data curation, IL, EM.; writing—original draft preparation, IL.; writing—review and editing, ML, GF, LB; visualization, IL, LD.; supervision, ML, GF, LB ; project administration, ML, GF, LB, IL. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lakbar, I., Maakaron, E., Leone, M. et al. Severe mental illness and mortality in sepsis and septic shock: a systematic review and meta-analysis. Mol Psychiatry (2024). https://doi.org/10.1038/s41380-024-02603-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41380-024-02603-8