Abstract
Objective:
Our objective is to assess the frequency of usage, safety and clinical utility of humidified high flow nasal cannula (HHFNC) in two tertiary care hospitals and compare outcomes to a historical control group of premature infants who received nasal continuous positive airway pressure (NCPAP).
Study design:
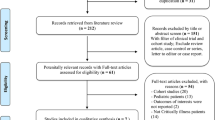
The first part of the study describes the increased HHFNC usage in two tertiary neonatal intensive care units. The second part compares outcomes of infants, born at less than 30 weeks gestation, who received either NCPAP or HHFNC as an early respiratory support mode.
Results:
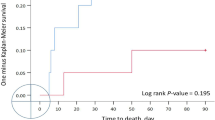
HHFNC usage increased (64%) after its introduction in infants of all gestational ages whereas the usage of NCPAP decreased from 19 to 4%. Ninety-five percent of infants born at less than 30 weeks gestation received HHFNC at some point during their hospital stay whereas only 12% received NCPAP. There were no differences in death or bronchopulmonary dysplasia (BPD), but ventilator-days per patient were decreased (19.4 to 9.9) following introduction of HHFNC. Comparing the cohort of infants who received either NCPAP or HHFNC as an early mode of respiratory support, there were no differences in deaths, ventilator-days, BPD, blood infections or other outcomes. More infants were intubated for failing early NCPAP compared to early HHFNC (40 to 18%).
Conclusions:
HHFNC was well-tolerated by premature infants. Compared to infants managed with NCPAP, there were no apparent differences in adverse outcomes following the introduction of HHFNC. Additional research is needed to better define the utility and safety of HHFNC compared to NCPAP.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Angus DC, Linde-Zwirble WT, Clermont G, Griffen MF, Clark RH . Epidemiology of neonatal respiratory failure in the United States. Am J Resp Crit Care Med 2001; 164: 1154–1161.
Hudson LD . Progress in understanding ventilator-induced lung injury. JAMA 1999; 282: 77–78.
Jobe AH, Ikegami M . Mechanisms initiating lung injury in the preterm infant. Early Hum Dev 1998; 53: 81–94.
Rich W, Finer NN, Vaucher YE . Ten-year trends in neonatal assisted ventilation of very low- birthweight infants. J Perinatol 2003; 28: 660–663.
Jegatheesan P, Keller RL, Hawgood S . Early variable-flow nasal continuous positive pressure in infants < or=1000 grams at birth. J Perinatol 2006; 26: 189–196.
Aly H, Milner JD, Patel K, El-Mohandes AA . Does the experience with the use of nasal continuous positive airway pressure improve over time in extremely low birth weight infants? Pediatrics 2004; 114: 697–702.
Narendran V, Donovan EF, Hoath SB, Akinbi HT, Steichen JJ, Jobe AH . Early bubble CPAP and outcomes in ELBW preterm infants. J Perinatol 2003; 23: 195–199.
Davis PG, Henderson-Smart DJ . Post-extubation prophylactic nasal continuous positive airway pressure in preterm infants: systematic review and meta-analysis. J Paediatr Child Health 1999; 35: 367–371.
Nair G, Karna P . Comparison of the effects of Vapotherm and nasal CPAP in respiratory distress in preterm infants. Pediatr Acad Soc 2005; 57: 2054.
Ovalle OO, Gomez T, Troncoso G, Palacios J, Ortiz E . High flow nasal cannula after surfactant treatment for infant respiratory distress syndrome in preterm infants <30 weeks. Pediatr Acad Soc 2005; 57: 3417.
Ramanathan A, Cayabyab R, Sardesai S, Siassi B, Seri I, Ramanathan R . High flow nasal cannula use in preterm and term newborns admitted to neonatal intensive care unit: A prospective, observational study. Pediatr Acad Soc 2005; 57: 3424.
Sanchez F, Sabato K . Very high nasal cannula-alternative to NCPAP in select ICN patients? Respir Care 2004; 49: 1373.
Holleman-Duray DL, Kaupie DL, Weiss MG . Safety and efficacy of the Vapotherm® high flow humidification system and an early extubation protocol. Pediatr Acad Soc 2006; 59: 517.
Sreenan C, Lemke RP, Hudson-Mason A, Osiovich H . High-flow nasal cannulae in management of apnea of prematurity: a comparison with conventional nasal continuous positive airway pressure. Pediatrics 2001; 107: 1081–1083.
Chang GC, Cox CC, Shaffer TH . Nasal cannula, CPAP, and Vapotherm: effect of flow on temperature, humidity, pressure and resistance. Pediatr Acad Soc 2005; 57: 1231.
Courtney SE, Pyon KH, Saslow JG, Arnold GK, Pandit PB, Habib RH . Lung recruitment and breathing pattern during variable versus continuous flow nasal continuous positive airway pressure in premature infants: an evaluation of three devices. Pediatrics 2001; 107: 304–308.
Finer NN . Nasal cannula use in the preterm infant: oxygen or pressure? Pediatrics 2005; 116: 1216–1217.
Walsh M, Engle W, Laptook A, Kazzi SNJ, Buchter S, Rasmussen M et al. Oxygen delivery through nasal cannulae to preterm infants: can practice be improved? Pediatrics 2005; 116: 857–861.
Saslow JG, Aghai ZH, Nakhla TA, Hart JJ, Lawrysh R, Stahl GE et al. Work of breathing using high-flow nasal cannula in preterm infants. J Perinatol 2006; 26: 476–480.
Locke RG, Wolfson MR, Shaffer TH, Rubenstein SD, Greenspan JS . Inadvertent administration of positive end-distending pressure during nasal cannula flow. Pediatrics 1993; 91: 135–138.
Kubicka Z, Limauro J, Darnall R . High flow nasal cannula therapy with Vapothem: yet another way to deliver CPAP? Pediatr Acad Soc 2006; 59: 5660.344.
Center for Disease Control Convention. Ralstonia associated with Vapotherm oxygen delivery device – United States, 2005. Morb Mortal Wkly Rep 2005; 54: 1052–1053.
Graham III PL, Begg MD, Larson E, Della-Latta P, Allen A, Saiman L . Risk Factors for late onset Gram-negative sepsis in low birth weight infants hospitalized in the neonatal intensive care unit. Pediatr Infect Dis J 2006; 25: 113–117.
Woodhead DD, Lambert DK, Clark JM, Christensen RD . Comparing two methods of delivering high-flow gas therapy by nasal cannula following endotracheal extubation: a prospective, randomized, masked, crossover trial. J Perinatol 2006; 26: 481–485.
Acknowledgements
The opinions expressed are of the authors only and do not necessarily represent those of the Department of the Air Force or the Department of Defense.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on the Journal of Perinatology website (http://www.nature.com/jp)
Supplementary information
Rights and permissions
About this article
Cite this article
Shoemaker, M., Pierce, M., Yoder, B. et al. High flow nasal cannula versus nasal CPAP for neonatal respiratory disease: a retrospective study. J Perinatol 27, 85–91 (2007). https://doi.org/10.1038/sj.jp.7211647
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211647
Keywords
This article is cited by
-
A Systematic Review of the High-flow Nasal Cannula for Adult Patients
Critical Care (2018)
-
Consensus approach to nasal high-flow therapy in neonates
Journal of Perinatology (2017)
-
Heated humidified high flow nasal cannula versus nasal continuous positive airway pressure as primary mode of respiratory support for respiratory distress in preterm infants
Indian Pediatrics (2016)
-
Weaning preterm infants from continuous positive airway pressure: evidence for best practice
World Journal of Pediatrics (2015)
-
Work of breathing indices in infants with respiratory insufficiency receiving high-flow nasal cannula and nasal continuous positive airway pressure
Journal of Perinatology (2014)