Abstract
Visceral obesity is a key risk factor for type 2 diabetes (T2D). Whereas gut dysbiosis appears to be instrumental for this relationship, whether gut-associated signatures translocate to extra-intestinal tissues and how this affects host metabolism remain elusive. Here we provide a comparative analysis of the microbial profile found in plasma, liver and in three distinct adipose tissues of individuals with morbid obesity. We explored how these tissue microbial signatures vary between individuals with normoglycaemia and those with T2D that were matched for body mass index. We identified tissue-specific signatures with higher bacterial load in the liver and omental adipose tissue. Gut commensals, but also environmental bacteria, showed tissue- and T2D-specific compartmentalisation. T2D signatures were most evident in mesenteric adipose tissue, in which individuals with diabetes displayed reduced bacterial diversity concomitant with fewer Gram-positive bacteria, such as Faecalibacterium, as opposed to enhanced levels of typically opportunistic Gram-negative Enterobacteriaceae. Plasma samples of individuals with diabetes were similarly enriched in Enterobacteriaceae, including the pathobiont Escherichia–Shigella. Our work provides evidence for the presence of selective plasma and tissue microbial signatures in individuals with severe obesity and identifies new potential microbial targets and biomarkers of T2D.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
Sequencing data was deposited to the European Nucleotide Archive, https://www.ebi.ac.uk/ena, with accession number: PRJEB36477. Secondary accession: ERP119674.
References
Zhang, Y., Niu, J. & Choi, H. K. Excess mortality among persons with type 2 diabetes. N. Engl. J. Med. 374, 788 (2016).
Seshasai, S. R., Kaptoge, S., Thompson, A., Di Angelantonio, E. & Gao, P. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N. Engl. J. Med. 364, 829–841 (2011).
American Diabetes Association Diagnosis and classification of diabetes mellitus. Diabetes Care 37, S81–S90 (2014).
Locke, A. E. et al. Genetic studies of body mass index yield new insights for obesity biology. Nature 518, 197–206 (2015).
Ridaura, V. K. et al. Gut microbiota from twins discordant for obesity modulate metabolism in mice. Science 341, 1241214 (2013).
Delzenne, N. M., Cani, P. D., Everard, A., Neyrinck, A. M. & Bindels, L. B. Gut microorganisms as promising targets for the management of type 2 diabetes. Diabetologia 58, 2206–2217 (2015).
Janesick, A. S., Shioda, T. & Blumberg, B. Transgenerational inheritance of prenatal obesogen exposure. Mol. Cell. Endocrinol. 398, 31–35 (2014).
Pedersen, H. K. et al. Human gut microbes impact host serum metabolome and insulin sensitivity. Nature 535, 376–381 (2016).
Paisse, S. et al. Comprehensive description of blood microbiome from healthy donors assessed by 16S targeted metagenomic sequencing. Transfusion 56, 1138–1147 (2016).
Lluch, J. et al. The characterization of novel tissue microbiota using an optimized 16S metagenomic sequencing pipeline. PLoS One 10, e0142334 (2015).
Amar, J. et al. Intestinal mucosal adherence and translocation of commensal bacteria at the early onset of type 2 diabetes: molecular mechanisms and probiotic treatment. EMBO Mol. Med. 3, 559–572 (2011).
Lelouvier, B. et al. Changes in blood microbiota profiles associated with liver fibrosis in obese patients: a pilot analysis. Hepatology 64, 2015–2027 (2016).
Alvarez-Silva, C. et al. Compartmentalization of immune response and microbial translocation in decompensated cirrhosis. Front. Immunol. 10, 1–11 (2019).
Schertzer, J. D. et al. NOD1 activators link innate immunity to insulin resistance. Diabetes 60, 2206–2215 (2011).
Cani, P. D. et al. Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes 56, 1761–1772 (2007).
Blasco-Baque, V. et al. Periodontitis induced by porphyromonas gingivalis drives periodontal microbiota dysbiosis and insulin resistance via an impaired adaptive immune response. Gut 66, 872–885 (2017).
Cavallari, J. F. et al. Muramyl dipeptide-based postbiotics mitigate obesity-induced insulin resistance via IRF4. Cell Metab. 25, 1063–1074.e3 (2017).
Denou, E. et al. Defective NOD2 peptidoglycan sensing promotes diet-induced inflammation, dysbiosis, and insulin resistance. EMBO Mol. Med. 7, 259–274 (2015).
Verma, R. et al. Cell surface polysaccharides of Bifidobacterium bifidum induce the generation of Foxp3+ regulatory T cells. Sci. Immunol. 3, eaat6975 (2018).
Schierwagen, R. et al. Trust is good, control is better: technical considerations in blook microbiome analysis. Gut https://gut.bmj.com/content/early/2019/06/15/gutjnl-2019-319123 (2019).
Schierwagen, R. et al. Circulating microbiome in blood of different circulatory compartments. Gut 68, 578–580 (2019).
Le Chatelier, E. et al. Richness of human gut microbiome correlates with metabolic markers. Nature 500, 541–546 (2013).
Zeevi, D. et al. Personalized nutrition by prediction of glycemic responses. Cell 163, 1079–1094 (2015).
Thingholm, L. B. et al. Obese individuals with and without type 2 diabetes show different gut microbial functional capacity and composition. Cell Host Microbe 26, 252–264.e10 (2019).
Sokol, H. et al. Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn disease patients. Proc. Natl Acad. Sci. USA 105, 16731–16736 (2008).
Salomäki-Myftari, H. et al. Neuropeptide Y overexpressing female and male mice show divergent metabolic but not gut microbial responses to prenatal metformin exposure. PLoS One 11, e0163805 (2016).
Verdam, F. J. et al. Human intestinal microbiota composition is associated with local and systemic inflammation in obesity. Obesity (Silver Spring). 21, E607–E615 (2013).
Natividad, J. M. et al. Bilophila wadsworthia aggravates high fat diet induced metabolic dysfunctions in mice. Nat. Commun. 9, 2802 (2018).
Jensen, B. A. H. et al. Lysates of Methylococcus capsulatus Bath induce a lean-like microbiota, intestinal FoxP3+RORγt+IL-17+ Tregs and improve metabolism. Preprint at bioRxiv https://doi.org/10.1101/855486 (2019).
de Goffau, M. C. et al. Human placenta has no microbiome but can contain potential pathogens. Nature 572, 329–334 (2019).
Salter, S. J. et al. Reagent and laboratory contamination can critically impact sequence-based microbiome analyses. BMC Biol. 12, 1–12 (2014).
Glassing, A., Dowd, S. E., Galandiuk, S., Davis, B. & Chiodini, R. J. Inherent bacterial DNA contamination of extraction and sequencing reagents may affect interpretation of microbiota in low bacterial biomass samples. Gut Pathog. 8, 1–12 (2016).
Mowat, A. M. & Agace, W. W. Regional specialization within the intestinal immune system. Nat. Rev. Immunol. 14, 667–685 (2014).
Thaiss, C. A. et al. Hyperglycemia drives intestinal barrier dysfunction and risk for enteric infection. Science 359, 1376–1383 (2018).
Park, C. et al. Obesity modulates intestinal intraepithelial T cell persistence, CD103 and CCR9 expression, and outcome in dextran sulfate sodium–induced Colitis. J. Immunol. 203, 3427–3435 (2019).
Petersen, C. et al. T cell-mediated regulation of the microbiota protects against obesity. Science 365, eaat9351 (2019).
Luck, H. et al. Gut-associated IgA+ immune cells regulate obesity-related insulin resistance. Nat. Commun. 10, 3650 (2019).
Castillo, D. J., Rifkin, R. F., Cowan, D. A. & Potgieter, M. The healthy human blood microbiome: fact or fiction?. Front. Cell. Infect. Microbiol. 9, 148 (2019).
Brunt, E. M., Janney, C. G., Di Bisceglie, A. M., Neuschwander-Tetri, B. A. & Bacon, B. R. Nonalcoholic steatohepatitis: a proposal for grading and staging the histological lesions. Am. J. Gastroenterol. 94, 2467–2474 (1999).
Forslund, K. et al. Disentangling type 2 diabetes and metformin treatment signatures in the human gut microbiota. Nature 528, 262–266 (2015).
Escudie, F. et al. FROGS: find, rapidly, OTUs with Galaxy solution. Bioinformatics 34, 1287–1294 (2018).
Acknowledgements
This study was supported by a bariatric care team grant (TB2-138776) and a Canadian Microbiome Initiative team grant (MRT-168045) from the Canadian Institutes of Health Research (CIHR) and by a CIHR Foundation Scheme grant to A.M. (FDN-143247). A.M. was supported by a CIHR and Pfizer research chair in the pathogenesis of insulin resistance and cardiovascular diseases. F.F.A. holds a CIHR postdoctoral fellowship and Diabetes Canada incentive funding. B.A.H.J. was supported by awards from the Lundbeck Foundation (R232-2016-2425) and Novo Nordisk Foundation (NNF17OC0026698).
Author information
Authors and Affiliations
Contributions
A.M., A.T., F.F.A. and B.A.H.J. conceived and planned the study. A.T., B.A.H.J. and F.F.A. identified and selected the patient cohort. S.M. and L.B. conducted tissue biopsies. B.L. led tissue 16S rRNA gene quantification and sequencing. F.S., S.V.B. and T.V.V. carried out bioinformatic analysis. F.F.A. and T.V.V. generated the figures. F.F.A. and B.A.H.J. integrated the data and wrote the manuscript. F.F.A, B.A.H.J., T.V.V., F.S., S.V.B., D.R., S.M., M.S., L.B., B.L., J.D.S., A.T. and A.M. contributed to data analysis and discussion and agreed upon the submitted manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Peer review information Primary Handling Editors: Christoph Schmitt; Pooja Jha.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
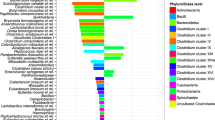
Extended Data Fig. 1 Genera distribution in the liver, plasma and mesenteric, omental and subcutaneous adipose tissue of obese subjects.
Filtered genera were plotted in a heatmap whereby genus abundance is depicted for each sample within each tissue analyzed. Dendograms on the left of heatmaps are based on correlations of abundance profile.
Extended Data Fig. 2 Principal Coordinate Analysis on generalized UniFrac distances of 16S sequences from negative controls.
Permutational multivariate analysis of variance (PERMANOVA), with subsequent Bonferroni-Holm P adjustment, was used to assign statistical significance to the differences between clusters of 16S sequences. The number of independent biological samples tested was: Air-Liver (n=3), Air-OAT (n=2), Air-SAT (n=3). The number of technical replicates tested was: Air-Lab (n=3), Air-Biobank (n=3), Swab-Biobank (n=3), Ext-Wa (n=6). Each dot represents a sample. All statistical testes were two-sided, and differences were considered statistically significant at P<0.05.
Extended Data Fig. 3 Validation with negative controls of tissue-specific taxa different between participants who were normoglycemic or type 2 diabetic.
Tissue-specific bacterial targets found to discriminate between disease state were identified by LefSe analysis. The relative abundance of these taxa (at family and genus level) in liver (a, b), mesenteric (MAT – c, d), omental (OAT – e, f) and subcutaneous (SAT – g, h) adipose tissue and plasma (i, j) was analyzed, without accounting for disease state distribution, against negative controls (NCs) using Mann-Whitney U test. P values are indicated at the top of each graph. Left side panels show the relative abundance of taxa, whereas right side panels depict relative abundance normalized by 16S rRNA gene count (that is, relative abundance x 16S count). Box plots depict the first and the third quartile with the median represented by a vertical line within the box; the whiskers extend from the first and third quartiles to the highest and lowest observation, respectively, not exceeding 1.5 x IQR. Each circle (Non-diabetic, ND) and triangle (Type 2 Diabetic, T2D) represents a sample, and their tissue-specific dispersion is presented using a log10 scale. The number of independent biological replicates tested was: Liver (n=39), MAT (n=40), OAT (n=40), SAT (n=40), Plasma (n=39), NC (n=23). All statistical tests were two-sided, and differences were considered statistically significant at P<0.05.
Supplementary information
Supplementary Table 1
List of medication use divided into columns of targeted disease indication
Rights and permissions
About this article
Cite this article
Anhê, F.F., Jensen, B.A.H., Varin, T.V. et al. Type 2 diabetes influences bacterial tissue compartmentalisation in human obesity. Nat Metab 2, 233–242 (2020). https://doi.org/10.1038/s42255-020-0178-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s42255-020-0178-9
This article is cited by
-
Effects of dietary fibre on metabolic health and obesity
Nature Reviews Gastroenterology & Hepatology (2024)
-
Gut microbiota in overweight and obesity: crosstalk with adipose tissue
Nature Reviews Gastroenterology & Hepatology (2024)
-
Cross-alteration of murine skin and tick microbiome concomitant with pathogen transmission after Ixodes ricinus bite
Microbiome (2023)
-
The gut microbiota in obesity and weight management: microbes as friends or foe?
Nature Reviews Endocrinology (2023)
-
The visceral adipose tissue bacterial microbiota provides a signature of obesity based on inferred metagenomic functions
International Journal of Obesity (2023)