Abstract
Except for histological study, there are currently no suitable techniques available for the detection and identification of primordial follicles in ovary of primary ovarian insufficiency patients who have undetectable AMH levels. Also, the ability to locate and quantify follicles on ovarian cortex strips, without fixation, is valuable for patients who could undergo subsequent successful ovarian tissue transplantation. Although optical coherence tomography (OCT) is a well-established high resolution imaging technique without fixation commonly applied in biomedicine, few reports are available on ovarian tissue imaging. In present study, we established standard OCT follicle images at each developmental stage, including the primordial follicle, and demonstrated the efficacy of OCT to estimate IVF outcome in transplanted mice ovary like ovarian reserve tests. Unfortunately, the current commercial OCT could not be used to accurate follicle count the number of follicles for whole ovary, because the maximum depth of examination was 100 μm. And we demonstrated the safety of OCT examination, it did not affect IVF outcome and birth defect rate, and reproductive ability. Although there is room for improvement, these findings will be first step to bring OCT examination a step closer to clinical application for measuring true ovarian reserve and localizing follicles.
Similar content being viewed by others
Introduction
Reproductive aging is related to both a quantitative and a qualitative reduction of the primordial follicle pool1. The quantitative ovarian reserve may vary substantially between women of the same chronological age2 because the initial endowment of primordial follicles, and rate of follicle loss, are highly variable between individuals3. Besides the age of patients, ovarian reserve tests (ORTs) have been developed to assess ovary function. These tests include basal FSH level, basal inhibin B, basal estradiol level, the clomiphene citrate challenge test (CCCT), the GnRH agonist challenge test (GAST), exogenous FSH ovarian reserve test (EFORT), the ovarian antral follicle count (AFC), and serum level of anti-Müllerian hormone (AMH)4,5. Several of these tests have become part of the standard pretreatment assessment for IVF (in vitro fertilization) designed to assess oocyte yield in response to gonadotropins and the probability of ongoing pregnancy after IVF5,6. In particular, there are strong indications that AMH and AFC may serve as good candidate markers for the determination of the ovarian reserve; for example, the area under the receiver operating curve (AUC) of AMH and AFC were 0.78 and 0.76 respectively7. However, AMH and AFC have limitations in assessing true ovarian reserve for immoderate diminished ovarian reserve patients, despite being reliable tests. In fact, around 100 to 1000 follicles remain in the ovary of patients who have undetectable serum AMH levels4. At this time, there are no tests that can confirm the true number of remaining follicles in the ovary except histological study with formaldehyde fixation. Indeed, knowing the true number of remaining follicles would be helpful for primary ovarian insufficiency patients (POI) in making decisions about continued fertility treatment. Furthermore, knowing the true number and localization of follicles in the ovarian tissue strips would be also helpful for patients who receive ovarian tissue transplantation as fertility treatment after cancer therapy or fertility treatment with in vitro activation (IVA)8,9, because they could receive an ovarian tissue transplantation with most suitable ovarian tissue containing the largest number of follicles.
Optical coherence tomography (OCT) is an emerging high-resolution and non-invasive imaging technique that has many applications in biomedicine10,11. The OCT technique measures back-scattered light from microstructural features within the examined tissues in the scale of several to tens of microns with a penetration depth of 1–3 mm11,12. Recently, OCT has been used to image tissues in the body for clinical examination including areas that can be accessed either directly, or via an endoscope or catheter, such as ophthalmology13,14, dentistry15,16, gastrointestinal tract17,18, coronary blood vessels19,20, colon21, breast22,23, and so forth11,12. In addition, some researchers have attempted OCT technique application in ovary investigation10,12,24,25,26,27.
Using the latest OCT equipment, our study aims to establish a protocol for standardized follicles imaging at each developmental stage, to assess the efficacy of OCT to estimate IVF outcome like ovarian reserve tests, and to investigate the safety of OCT for optimal gamete viability.
Result
Standard OCT images of mice ovary on individual age
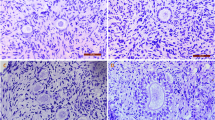
We could detect each developing follicles by OCT examination, including primordial follicles. And also, we established the standard OCT images of each developing stage follicles shown as Fig. 1. It shows a set of OCT images and H&E-stained histology images from healthy ICR mice at various ages. The OCT image from the day 3 mouse shows many primordial follicles consistent with the H&E-stained images (Fig. 1a,b). OCT images from the day 10 mice show primary and early secondary follicles consistent with the H&E-stained images (Fig. 1c,d). Also, 3D imaging of the day 10 mice is shown in Fig. 1e. The OCT images from the day 21 mice (Fig. 1f,g) show the late secondary and antral follicles consistent with the H&E-stained images (Fig. 1h,i). In 30 weeks old mice, some pre-antral follicles and corpus luteum are shown in the OCT images (Fig. 1j) and the H&E-stained images (Fig. 1k). In addition, in the 50 weeks old mice, a no follicles were visible in the OCT images (Fig. 1l,n) and the H&E-stained images (Fig. 1m,o).
OCT images: (a,c,f,h,j,l,n), Histology: (b,d,g,i,k,m,o), 3D OCT image: (e) Histological images: many primordial follicles (white arrows) were seen in (a) day 3 mouse ovaries, primary to early secondary follicles (white arrows) were seen in day 10 mouse ovaries (c), secondary follicles and antral follicles (white arrows) were seen in (f,h) day 21 mouse ovaries. Image (e) is 3D imaging demonstrates the stereoscopic structure of (c). There are many primordial and primary follicles (black arrows) and early secondary follicles (white arrow). There were few secondary follicles (white arrows), however, seen in the OCT images of 30 weeks old mouse (j), and 50 weeks old mice (l,n) corresponding with histology (k,m,o, respectively). Each bar denotes 100 μm.
IVF for ovarian tissue transplantation outcome after OCT examination
Figure 2a and b shows a transplanted ovary pair two weeks after transplantation following OCT examination. No oocytes could be retrieved from 30 or 50 weeks old mice ovaries (n = 5 each). Among the day 3 ovaries transplanted into kidney capsule with (n = 10)/without OCT examination (without OCT examination: control group, n = 15), there was no significant difference between the number of extracted oocytes from the transplanted ovaries (10.8 ± 0.8 and 9.4 ± 0.8, p = 0.29), the mean number of fertilized oocytes (6.9 ± 0.4 and 6.8 ± 0.7, p = 0.81), the fertilization rate (67.9 ± 2.7% and 73.5 ± 6.3%, p = 0.35), the number of blastocysts (5.2 ± 0.3 and 5.9 ± 0.8, p = 0.34), or the blastocyst rate (76.5 ± 4.1% and 87.3 ± 5.8%, p = 0.14) (Fig. 3a–e). Four 10 weeks old female mice received transplants of 48 blastocysts resulting in the Cesarean delivery of 27 normal mice. None of the delivered mice displayed gross deformities or abnormal placentas. The birth and placenta weight from transplanted ovaries with OCT were 1.59 ± 0.02 g and 0.11 ± 0.01 g, respectively. Compared with the control group (32 transplanted blastocysts among two host mice), there was a significant difference only in terms of birth weight (control group: birth weight 1.31 ± 0.03 g, placenta weight 0.12 ± 0.01 g) (Fig. 4a,b). Meanwhile, the delivery rate (control: 59.3 ± 3.1%, with OCT: 53.1 ± 7.9%) and the miscarriage rate (control: 25.0 ± 6.3%, with OCT: 32.9 ± 3.0%) were unchanged (Fig. 4c,d). All 5 mated female mice became pregnant and delivered healthy litters of 11.2 ± 0.4 progeny (female 5.4 ± 0.2 and male 5.8 ± 0.4).
(a) Day 3 ovary was transplanted into left side kidney after OCT examination. On the other hands, aged mice ovary (30 weeks) was transplanted into the right side kidney after OCT examination. (b) Day 3 ovary was transplanted into left side kidney after OCT examination. On the other hands, aged mice ovary (50 weeks) was transplanted into the right side kidney after OCT examination. In contrast, many developed follicles were seen on left side of the ovary (white arrows). Especially, aged mice ovary (50 weeks) was absorbed due to severe follicle loss (black arrow).
Without OCT examination of day 3 ovaries were defined as “control” group (n = 15). And with OCT examination of day 3 ovaries were defined as “with OCT” group (n = 10). Using statistical analysis, there were no significant differences between “control” and “with OCT” groups, in terms of number of extracted oocytes (a) (p = 0.29), fertilized embryos (b) (p = 0.81), blastocyst number (d) (p = 0.34), fertilization rate (c) (p = 0.35) or blastocyst rate (e) (p = 0.14). The level of significance was set at p < 0.05. In addition, there were no extracted oocytes from transplanted 30 and 50 weeks old mice ovaries (n = 5 each).
Discussion
Although it has been demonstrated that OCT could be used for ovarian tissue characterization, we found that traditional OCT equipment had insufficient resolution for detailed visualization of ovarian tissue characteristics such as primordial follicles10,11,12,28. Recently, researchers reported the efficacy of OCT to detect cancer metastasis and to confirm follicle density27. However, there is still little detailed information for standard imaging practice in examining ovarian tissue characteristics with OCT. Therefore, in present study we established more detailed images of ovaries including 3D images using OCT equipment on the mice ovaries. In addition, the present study is the first to report the primordial follicle detection on fresh (rather than fixed and embedded) ovary, which strongly indicates the viability of OCT examination for clinical application in the assessment of ovarian reserve and the localization of primordial follicles.
According to IVF outcomes using transplanted mouse ovaries with OCT examination, we demonstrated a strong correlation between the number of extracted oocytes and the OCT findings. Consistent with earlier reports, OCT findings were well correlated with histological data27. Therefore, we concluded that OCT examination could potentially be used to estimate ovarian reserve and IVF outcome in a similar manner to current tests such as serum AMH and basal follicle stimulation hormone levels and antral follicle counts.
Concerning clinical application, however, OCT examination of a whole human ovary would require prolonged exposure to near-infrared light (NIR) for image acquisition. Another issue is that OCT examination is best suited for flat surfaces as opposed to the round shape of the ovary. In present study, the maximum depth of examination was 100 μm. Therefore, unfortunately, the current commercial OCT could not be used to count the number of developing follicles because they are at a depth of up to 3 mm in the human ovarian cortex29,30; in particular, early human follicles were detected within 0.75 mm from the surface of the ovarian cortices31. Although OCT could assess the ovarian reserve and localization of thin-sliced human ovarian cortex with embedding and fixation27, these issues need resolution before clinical application will be possible to assess entire ovarian reserve of human being.
Currently, ovarian tissue cryopreservation is one of the key strategies in fertility preservation for young cancer patients who face imminent chemotherapy or radiation therapy, such as cyclophosphamide chemotherapy, which have deleterious effect for ovarian reserve32. Although ovarian tissue cryopreservation is still considered to be experimental, it is the only option in girls because there is no standard modality available for fertility preservation in girls33,34. Including our cases, there have been over 60 live births from transplanted ovarian tissues reported8,35. Recently, the first successful case of fertility restoration from ovarian tissue cryopreserved before menarche was reported36. Although accurate information regarding post-transplantation pregnancy rate is still limited, the pregnancy rate for ovarian tissue transplant was reported to be 18.3 to 36.3%32,34,35. While ovarian tissue cryopreservation techniques are advancing, many challenges remain for optimizing them. Remaining challenges include the efficacy of transplanted ovarian tissues, which is related to the ovarian reserve of patient, the method of ovarian tissue preparation, freezing-thawing techniques, the amount of ovarian tissue available for transplantation, transplantation techniques, and graft sites34,37. The present study indicates that OCT may be able to resolve these concerns by clarifying the number and localization of follicles in ovarian tissue. It is possible for OCT to aid in selecting the best ovarian tissue for ovary tissue transplantation. With ovarian tissue transplantation, the greatest concern would be in reintroducing metastatic malignancy following transplantation. To solve this problem, the OCT technique may be able to screen for cancer metastases present in ovarian tissue prior to transplantation27. Also, OCT may advance basic research in the area of ovarian tissue cryopreservation because it allows researchers to accurately count follicles in the ovary before and after ovarian tissue transplantation. Therefore, OCT will promote the development of methodologies for ovarian tissue cryopreservation and transplantation.
There are no reports from standpoint of OCT safety in reproductive health; although, the viability of ovarian tissue has been examined using the glucose uptake assay and neutral red staining27. A previous study investigated the thermal effects of its zona drilling on bovine and murine embryos38, however, heat effects caused of near infrared light exposure is still unknown. Therefore, the use of NIR technology in assisted reproduction is currently being investigated39. Currently, NIR laser-assisted embryo hatching is a common method in the area of assisted reproductive technology that aims to increase implantation and pregnancy rates. Although the clinical efficacy of laser-assisted hatching remains controversial40,41, NIR has been used widely in reproductive medicine and researchers have seen no evidence that the embryos are damaged during the laser hatching procedure42. For IVF applications, lasers now use near infrared light allowing for successful applications and minimizing DNA damage to the blastomeres38. In addition, NIR spectroscopic analysis has been applied to oocyte viability assessment for non-invasive clinical research39. In our study, we demonstrated that successive OCT and IVF protocols were not a detriment to the numbers of extracted oocytes, fertilization rate, or the blastocyst rate compared with IVF without OCT examination. Also, OCT examination was not harmful the placenta or offspring weight. Although there was significant difference on the birth weight, there was no difference on placenta weight. It is a just speculation, increasing of birth weight was due to some individual difference. In addition, OCT examination did not increase birth defects in offspring, and the offspring from transplanted ovaries had normal reproductive capacity. Certainly, our study alone is not sufficient to prove the absolute safety of NIR exposure used in OCT examination, but present study is the first to report evidence for reproductive safety in the application of OCT examination. If OCT examination is to be used in clinical application, the safety of longer exposure NIR times must be investigated.
In conclusion, OCT is a new and likely safe tool for assessing ovarian reserve without the need for fixation. With optimization for use in human ovarian tissue, it may eventually be used to directly count the number of primordial and developing follicles, which are different from currently available indirect methods such as serum AMH level, basal follicle stimulation hormone level, and antral follicle count. Lastly, the ability to know the accurate number and localization of developing follicles via OCT will allow for its use in ovarian tissue transplantation procedures, and be very helpful for patients who receive ovarian tissue transplantation for future pregnancy.
Materials and Methods
Experimental animals
Day 3, 10, and 21, and 30 and 50 week old female ICR mice (CLEA Japan and Japan SLC, Tokyo, Japan) were housed under a 12 hours light/dark cycle at 22 °C and fed ad libitum for ovarian tissue harvest. Under these housing conditions, 6 weeks old female ICR mice (Japan SLC, Tokyo, Japan) acted as ovarian transplantation recipients, and 10 weeks old female ICR mice acted as host mothers (Japan SLC, Tokyo, Japan). The experimental protocols and animal-handling procedures were performed with the approval of the Institutional Animal Care and Use Committee (IACUC) of St. Marianna University School of Medicine. Dissection, ovarian tissue transplantation, and in vitro fertilization were performed according to IACUC approved protocols.
Preparation of mouse ovaries
Mice ovaries were obtained from mice of various ages as outlined above. Harvested ovaries were stored for 8–9 hours prior to OCT examination and ovarian tissue transplantation on ice in DMEM culture medium (Gibco, Thermo Fisher Scientific, MA, USA) supplemented with 10% FBS (Foetal Bovine Serum; Bovogen Biologicals, Melbourne, Australia) and 1% of antibiotics (Anti-Anti; Gibco, Thermo Fisher Scientific, MA, USA).
Optical coherence tomography examination
The latest OCT system (Light-CT scanner; LL Tech, Paris, France) was used in present study. The mechanical characteristic of Light-CT scanner included images with 1 μm resolution in all three dimensions and 3D views that can be manipulated using a standard DICOM viewer. The wavelength of the OCT examination was 700 nm, the width of the wave was 125 nm, and the area of examination was 800 μm2.
To compare standard histological with OCT images of the ovary, mouse ovaries from each age group (day 3, 10, 21 and 30 weeks and 50 weeks) were examined using the OCT system. And ovaries for transplantation to kidney (as stated below) were also examined by same system. Images were taken up to a depth of 100 μm which was maximum depth at which high resolution images can be taken. The average exposure time during the OCT examination was 4–5 min.
Histological study of mouse ovary
Ovaries examined with OCT were fixed by Bouin’s solution (Polysciences inc., PA, USA) and embedded in paraffin wax for sectioning (5 μm thick) followed by standard hematoxylin-and-eosin staining for later comparison.
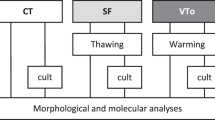
Ovary tissue transplantation
To verify the accuracy of OCT ovarian reserve estimation, ovarian tissue transplantation and IVF were performed, thereafter we compared the relationship between OCT images and outcome of in vitro fertilization (IVF). According to our previous study43, ovarian tissue transplantation must be performed within 8 hours of ovary extraction to maintain a normal IVF outcome.
Paired ovaries (day 3, 30 weeks, or 50 weeks old) examined by OCT were inserted, one under each kidney capsule, into the same 6 weeks old host mouse that had been ovariectomized to increase endogenous gonadotropin levels. To conform ovarian tissue transplantation efficiency, ovaries of 30 weeks old mice were cut into half, and the 50 weeks old mice ovaries were cut into pieces of the same size as that of day3 mice ovaries. And also, ovaries of day3 mice without OCT examination were prepared and transplanted to serve as a control group.
In vitro fertilization and embryo transfer, breeding
In addition, to confirm the safety of OCT examination, IVFs were performed after ovarian tissue transplantation. To retrieve the first wave of oocytes from the ovaries, host mice were treated with 5 IU Serotropin (ASKA Pharmaceutical Co., Ltd, Tokyo, Japan) injections two weeks after ovarian tissue transplantation, followed by an intraperitoneal injection of 10 IU human chorionic gonadotrophin (hCG, Gonatropin; ASKA Pharmaceutical Co., Ltd, Tokyo, Japan) 48 hours later. Cumulus oocyte complexes (COCs) were collected from the ovaries and fallopian tube ampulla 14 hours hCG injection to compare the number of retrieved oocytes between day 3 mouse ovaries versus 30 weeks or 50 weeks old mouse ovaries. Later, retrieved oocytes were inseminated and cultured to the blastocyst stage for implantation into 10 weeks old ICR host mice. After embryo transfer and resultant pregnancy, newborn mice were delivered by Cesarean section. These resulting progeny were bred to screen for anomalies resulting from OCT examination.
Statistical analysis
The JMP Pro version 12 program (SAS Institute Inc., NC, USA) was used for statistical analysis. The extracted oocyte number from transplanted ovaries, number of fertilized oocytes and blastocysts, and the fertilization and blastocyst rates were expressed as the mean + standard error (SE). A student t-Test test was performed and a P value of p < 0.05 was considered significant.
Additional Information
How to cite this article: Takae, S. et al. Accuracy and safety verification of ovarian reserve assessment technique for ovarian tissue transplantation using optical coherence tomography in mice ovary. Sci. Rep. 7, 43550; doi: 10.1038/srep43550 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Faddy, M. J. & Gosden, R. G. A model conforming the decline in follicle numbers to the age of menopause in women. Human reproduction 11, 1484–1486 (1996).
Broekmans, F. J., Faddy, M. J., Scheffer, G. & te Velde, E. R. Antral follicle counts are related to age at natural fertility loss and age at menopause. Menopause 11, 607–614 (2004).
Broekmans, F. J., Soules, M. R. & Fauser, B. C. Ovarian aging: mechanisms and clinical consequences. Endocrine reviews 30, 465–493, doi: 10.1210/er.2009-0006 (2009).
Hansen, K. R., Hodnett, G. M., Knowlton, N. & Craig, L. B. Correlation of ovarian reserve tests with histologically determined primordial follicle number. Fertility and sterility 95, 170–175, doi: 10.1016/j.fertnstert.2010.04.006 (2011).
Hendriks, D. J. et al. Repeated clomiphene citrate challenge testing in the prediction of outcome in IVF: a comparison with basal markers for ovarian reserve. Human reproduction 20, 163–169, doi: 10.1093/humrep/deh553 (2005).
Sills, E. S., Alper, M. M. & Walsh, A. P. Ovarian reserve screening in infertility: practical applications and theoretical directions for research. Eur J Obstet Gynecol Reprod Biol 146, 30–36, doi: 10.1016/j.ejogrb.2009.05.008 (2009).
Broer, S. L. et al. Added value of ovarian reserve testing on patient characteristics in the prediction of ovarian response and ongoing pregnancy: an individual patient data approach. Human reproduction update 19, 26–36, doi: 10.1093/humupd/dms041 (2013).
Kawamura, K. et al. Hippo signaling disruption and Akt stimulation of ovarian follicles for infertility treatment. Proceedings of the National Academy of Sciences of the United States of America 110, 17474–17479, doi: 10.1073/pnas.1312830110 (2013).
Suzuki, N. Ovarian tissue cryopreservation using vitrification and/or in vitro activated technology. Human reproduction 30, 2461–2462, doi: 10.1093/humrep/dev212 (2015).
Yang, Y., Wang, T., Brewer, M. & Zhu, Q. Quantitative analysis of angle-resolved scattering properties of ovarian tissue using optical coherence tomography. J Biomed Opt 17, 90503–90501, doi: 10.1117/1.JBO.17.9.090503 (2012).
Wang, T., Brewer, M. & Zhu, Q. An overview of optical coherence tomography for ovarian tissue imaging and characterization. Wiley Interdiscip Rev Nanomed Nanobiotechnol 7, 1–16, doi: 10.1002/wnan.1306 (2015).
Yang, Y. et al. Integrated optical coherence tomography, ultrasound and photoacoustic imaging for ovarian tissue characterization. Biomed Opt Express 2, 2551–2561, doi: 10.1364/BOE.2.002551 (2011).
Yu, L. & Chen, Z. Doppler variance imaging for three-dimensional retina and choroid angiography. J Biomed Opt 15, 016029, doi: 10.1117/1.3302806 (2010).
Li, P. et al. Extended imaging depth to 12 mm for 1050-nm spectral domain optical coherence tomography for imaging the whole anterior segment of the human eye at 120-kHz A-scan rate. J Biomed Opt 18, 16012, doi: 10.1117/1.JBO.18.1.016012 (2013).
Otis, L. L., Everett, M. J., Sathyam, U. S. & Colston, B. W. Jr. Optical coherence tomography: a new imaging technology for dentistry. J Am Dent Assoc 131, 511–514 (2000).
Holtzman, J. S. et al. Ability of optical coherence tomography to detect caries beneath commonly used dental sealants. Lasers Surg Med 42, 752–759, doi: 10.1002/lsm.20963 (2010).
Testoni, P. A. & Mangiavillano, B. Optical coherence tomography in detection of dysplasia and cancer of the gastrointestinal tract and bilio-pancreatic ductal system. World J Gastroenterol 14, 6444–6452 (2008).
Cobb, M. J. et al. Imaging of subsquamous Barrett’s epithelium with ultrahigh-resolution optical coherence tomography: a histologic correlation study. Gastrointest Endosc 71, 223–230, doi: 10.1016/j.gie.2009.07.005 (2010).
Tearney, G. J. et al. Quantification of macrophage content in atherosclerotic plaques by optical coherence tomography. Circulation 107, 113–119 (2003).
Barlis, P. et al. Assessment of culprit and remote coronary narrowings using optical coherence tomography with long-term outcomes. Am J Cardiol 102, 391–395, doi: 10.1016/j.amjcard.2008.03.071 (2008).
Shen, B. et al. In vivo colonoscopic optical coherence tomography for transmural inflammation in inflammatory bowel disease. Clin Gastroenterol Hepatol 2, 1080–1087 (2004).
Boppart, S. A., Luo, W., Marks, D. L. & Singletary, K. W. Optical coherence tomography: feasibility for basic research and image-guided surgery of breast cancer. Breast Cancer Res Treat 84, 85–97, doi: 10.1023/B:BREA.0000018401.13609.54 (2004).
Curatolo, A. et al. Ultrasound-guided optical coherence tomography needle probe for the assessment of breast cancer tumor margins. AJR Am J Roentgenol 199, W520–522, doi: 10.2214/AJR.11.7284 (2012).
Yang, Y. et al. Optical scattering coefficient estimated by optical coherence tomography correlates with collagen content in ovarian tissue. J Biomed Opt 16, 090504, doi: 10.1117/1.3625247 (2011).
Boppart, S. A. et al. High resolution imaging of endometriosis and ovarian carcinoma with optical coherence tomography: feasibility for laparoscopic-based imaging. Br J Obstet Gynaecol 106, 1071–1077 (1999).
Pitris, C. et al. High-resolution imaging of gynecologic neoplasms using optical coherence tomography. Obstet Gynecol 93, 135–139 (1999).
Peters, I. T. et al. Non-invasive detection of metastases and follicle density in ovarian tissue using full-field optical coherence tomography. Clin Cancer Res, doi: 10.1158/1078-0432.CCR-16-0288 (2016).
Watanabe, Y., Takakura, K., Kurotani, R. & Abe, H. Optical coherence tomography imaging for analysis of follicular development in ovarian tissue. Applied optics 54, 6111–6115, doi: 10.1364/AO.54.006111 (2015).
Gonzalez, C. et al. Combined strategy for fertility preservation in an oncologic patient: vitrification of in vitro matured oocytes and ovarian tissue freezing. Journal of assisted reproduction and genetics 28, 1147–1149, doi: 10.1007/s10815-011-9628-3 (2011).
Imesch, P. et al. Developmental potential of human oocytes matured in vitro followed by vitrification and activation. J Ovarian Res 6, 30, doi: 10.1186/1757-2215-6-30 (2013).
Kagawa, N., Silber, S. & Kuwayama, M. Successful vitrification of bovine and human ovarian tissue. Reproductive biomedicine online 18, 568–577 (2009).
Oktay, K., Bedoschi, G., Pacheco, F., Turan, V. & Emirdar, V. First pregnancies, live birth, and in vitro fertilization outcomes after transplantation of frozen-banked ovarian tissue with a human extracellular matrix scaffold using robot-assisted minimally invasive surgery. Am J Obstet Gynecol 214, 94 e91–99, doi: 10.1016/j.ajog.2015.10.001 (2016).
Loren, A. W. et al. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 31, 2500–2510, doi: 10.1200/JCO.2013.49.2678 (2013).
Practice Committee of American Society for Reproductive, M. Ovarian tissue cryopreservation: a committee opinion. Fertility and sterility 101, 1237–1243, doi: 10.1016/j.fertnstert.2014.02.052 (2014).
Donnez, J. & Dolmans, M. M. Ovarian cortex transplantation: 60 reported live births brings the success and worldwide expansion of the technique towards routine clinical practice. Journal of assisted reproduction and genetics 32, 1167–1170, doi: 10.1007/s10815-015-0544-9 (2015).
Demeestere, I. et al. Live birth after autograft of ovarian tissue cryopreserved during childhood. Human reproduction 30, 2107–2109, doi: 10.1093/humrep/dev128 (2015).
Kim, S. S. Assessment of long term endocrine function after transplantation of frozen-thawed human ovarian tissue to the heterotopic site: 10 year longitudinal follow-up study. Journal of assisted reproduction and genetics 29, 489–493, doi: 10.1007/s10815-012-9757-3 (2012).
Douglas-Hamilton, D. H. & Conia, J. Thermal effects in laser-assisted pre-embryo zona drilling. J Biomed Opt 6, 205–213, doi: 10.1117/1.1353796 (2001).
Nagy, Z. P. et al. Metabolomic assessment of oocyte viability. Reproductive biomedicine online 18, 219–225 (2009).
Sagoskin, A. W., Levy, M. J., Tucker, M. J., Richter, K. S. & Widra, E. A. Laser assisted hatching in good prognosis patients undergoing in vitro fertilization-embryo transfer: a randomized controlled trial. Fertility and sterility 87, 283–287, doi: 10.1016/j.fertnstert.2006.07.1498 (2007).
Makrakis, E. et al. Laser versus mechanical assisted hatching: a prospective study of clinical outcomes. Fertility and sterility 86, 1596–1600, doi: 10.1016/j.fertnstert.2006.05.031 (2006).
Wong, B. C., Boyd, C. A. & Lanzendorf, S. E. Randomized controlled study of human zona pellucida dissection using the zona infrared laser optical system: evaluation of blastomere damage, embryo development, and subsequent hatching. Fertility and sterility 80, 1249–1254 (2003).
Kamoshita, K. et al. Investigation of in vitro parameters and fertility of mouse ovary after storage at an optimal temperature and duration for transportation. Human reproduction 31, 774–781, doi: 10.1093/humrep/dew023 (2016).
Acknowledgements
This research was partially supported by Keio Gijuku Fukuzawa Memorial Fund for the Advancement of Education and Research.
Author information
Authors and Affiliations
Contributions
S.T., K.T., N.S. designed research S.T., K.T., T.K., N.O., Y.S. performed experiments S.T., Y.S. analyzed data S.T., Y.S., N.S. manuscript drafting and figure creation S.T., K.T., N.S. critical discussion.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Takae, S., Tsukada, K., Sato, Y. et al. Accuracy and safety verification of ovarian reserve assessment technique for ovarian tissue transplantation using optical coherence tomography in mice ovary. Sci Rep 7, 43550 (2017). https://doi.org/10.1038/srep43550
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep43550
This article is cited by
-
Quantification and visualization of metastatic lung tumors in mice
Toxicological Research (2022)
-
Preliminary human application of optical coherence tomography for quantification and localization of primordial follicles aimed at effective ovarian tissue transplantation
Journal of Assisted Reproduction and Genetics (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.