Abstract
Autoimmune hepatitis (AIH) and primary biliary cholangitis (PBC) are liver-specific autoimmune conditions that are characterized by chronic hepatic damage and often lead to cirrhosis and hepatic failure. Specifically, the protein tyrosine phosphatase N22 (PTPN22) gene encodes the lymphoid protein tyrosine phosphatase, which acts as a negative regulator of T-cell receptor signaling. A missense single nucleotide polymorphism (SNP) (rs2476601) in PTPN22 has been linked to numerous autoimmune diseases in Caucasians. In the present series, nine SNPs in the PTPN22 gene were analyzed in 166 patients with AIH, 262 patients with PBC, and 322 healthy controls in the Japanese population using TaqMan assays. Although the functional rs3996649 and rs2476601 were non-polymorphic in all subject groups, the frequencies of the minor alleles at rs1217412, rs1217388, rs1217407, and rs2488458 were significantly decreased in AIH patients as compared with controls (all Pc < 0.05). There were no significant relationships with PTPN22 SNPs in PBC patients. Interestingly, the AAGTCCC haplotype was significantly associated with resistance to both AIH (odds ratio [OR] = 0.58, P = 0.0067) and PBC (OR = 0.58, P = 0.0048). SNPs in the PTPN22 gene may therefore play key roles in the genetic resistance to autoimmune liver disease in the Japanese.
Similar content being viewed by others
Introduction
Autoimmune diseases are characterized by an aberrant immune response to self-antigens. Although genetic factors contribute to disease susceptibility and severity, the mechanisms of disease initiation and persistence remain poorly understood. Autoimmune hepatitis (AIH)1,2 and primary biliary cholangitis (PBC)3,4 are prominent autoimmune diseases of the liver. Mutations in the human leukocyte antigen (HLA) region have been implicated in multiple autoimmune diseases, among which the HLA-DRB1*04:05-DQB1*04:01 and HLA-DRB1*08:03-DQB1*06:01 haplotypes were linked with susceptibility to AIH5,6 and PBC7 in Japanese populations. Polymorphisms of cytotoxic T-lymphocyte antigen 4 have also been identified as susceptibility determinants in PBC8, but not in AIH9. Furthermore, there is overlap among polymorphic loci identified by genome-wide association studies and linkage studies in several autoimmune diseases between Caucasians and the Japanese10,11,12,13.
The protein tyrosine phosphatase N22 gene (PTPN22) located on chromosome 1p13.3-13.1 encodes a lymphoid-specific protein tyrosine phosphatase (Lyp) that is important in the negative control of T-cell activation and in T-cell development. A missense single nucleotide polymorphism (SNP) known as rs2476601 in PTPN22 has been consistently associated with a variety of autoimmune diseases in populations of European ancestry, including rheumatoid arthritis (RA), type I diabetes, and systemic lupus erythematosus (SLE)14,15,16,17,18, but this functional SNP was non-polymorphic and no relationships were found in studies from Japan19,20,21,22.
Genome-wide association studies have confirmed that PTPN22 is associated with RA and type 1 diabetes23,24,25. Two SNPs, rs2488457 in the promoter region of PTPN22 and rs1217412 in the 3′-untranslated region, have also been linked to the onset of acute type 1 diabetes in Japanese and Korean populations18, and another amino acid substitution, rs33996649 within the catalytic domain of the enzyme, was related to the development of autoimmune diseases26. Meanwhile, several studies have implicated PTPN22 SNPs with autoimmune disorders independently of rs2488457, suggesting that such polymorphisms play a general role in autoimmunity. We therefore hypothesized that PTPN22 SNPs may also be associated with autoimmune liver disease and investigated for relationships between PTPN22 SNPs and AIH or PBC in Japanese patients.
Results
PTPN22 Genotyping in Patients and Controls
The functional rs3996649 and rs2476601 SNPs were not polymorphic in any study group, which was in agreement with previous studies19,20,21,22, and were therefore excluded from further analysis. The genotype frequencies of the remaining seven tested PTPN22 gene SNPs were in Hardy-Weinberg equilibrium in patients with AIH or PBC and in controls.
The minor allele frequencies at rs1217412, rs1217388, rs1217407, rs3765598, rs2488458, rs3789612, and rs2488457 were all significantly decreased among AIH patients as compared with healthy subjects (Table 1). Genotype frequencies also differed significantly between AIH patients and controls for rs1217412, rs1217388, rs1217407, rs3765598, rs2488458, and rs2488457 by a dominant model of inheritance (Table 2). The statistical power of this study was high at 0.999 when calculated as α = 0.05, β = 0.95, and sample number = 488.
The frequency of the minor T allele at rs3765598 was decreased in PBC patients as compared with healthy subjects (Table 1), as was positivity for the major C allele (CT+TT) at rs3765598 and rs3789612, but this difference was not significant after correction for multiple testing (Table 2).
PTPN22 Haplotypes in Patients and Controls
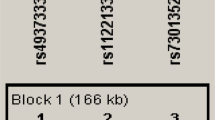
Pairwise linkage disequilibrium (LD) mapping confirmed that the seven tested alleles were in strong LD over a narrow range, with an LD index >0.9 (Table 3). Strong LD was indicated in the same block for AIH and PBC patients and controls. Nine unique SNP haplotypes were found altogether, of which four had frequencies of >5% (Table 4). Association analysis of haplotypes calculated by EM algorithms showed that haplotype 3, which was the only rs3765598 T, was significantly associated with resistance to both AIH (OR = 0.58, 95% CI 0.39–0.86, P = 0.0067) and PBC (OR = 0.58, 95% CI 0.40–0.85, P = 0.0048).
Association Between PTPN22 SNPs and Clinical Outcome
AIH and PBC patients were stratified according to disease progression. However, no SNP or haplotype in the PTPN22 gene was associated with either cirrhosis in AIH or a history of orthotopic transplantation and disease progression of PBC (data not shown).
Discussion
In recent studies on the PTPN22 gene, the rs2476601 missense substitution SNP has been associated with multiple autoimmune diseases in Caucasians, including RA, SLE, Graves’ disease, and Addison’s disease. rs2476601 was also proposed to be functionally involved in interactions between Lyp and Csk kinase13,14,27. Another functional SNP that is located in the catalytic domain of Lyp, rs33996649, leads to reduced phosphatase activity and has been highlighted as an important genetic risk factor for RA and SLE26. The present analysis showed that both of these SNPs were non-polymorphic (rs2476601: C, rs33996649: G) among all subject groups, in accordance with earlier studies from Asia19,20,21,22. Our data confirmed that the rs2476601 and rs33996649 SNPs were not associated with Japanese autoimmune liver disease.
This study revealed a striking association between SNPs in the PTPN22 gene and resistance to AIH. Although a genome-wide association study showed that PTPN22 was not related to AIH in patients of European descent13, there have been no data regarding PTPN22 SNPs in Japanese AIH. Hence, our results raise several possibilities on an association between PTPN22 loci and AIH protection in the Japanese population. First, among the five significantly associated SNPs in PTPN22, rs2488457 in the promoter region might be an important factor in Asian populations, as seen in case-control studies where it increased the risk of RA28,29 and ankylosing spondylitis30. Second, other potentially functional variants may be engaged in susceptibility to AIH as there are nine non-synonymous substitutions in addition to rs2476601 in exon 14 of PTPN22. Lastly, it is possible that the PTPN22 locus contains another, undefined functional variant in LD with rs3996649 or rs2476601. To address these prospects, we sequenced exon 14 of PTPN22 in 12 patients with AIH and 12 healthy controls whose genotypes were GG, AG, and AA at rs1217388 adjacent to rs2476601. No missense substitutions were detected in any sample, and all alleles were wild type (Fig. 1). However, the strong LD across this region as evidenced by pairwise D’ values near 1 (Table 3) made it difficult to ascertain whether these associated SNPs were independent protective factors of AIH. We compared haplotype frequencies between patients and controls to address this problem. Haplotype 3 containing AAGTCCC was less frequent in AIH and significantly associated with disease resistance (P = 0.0067, OR = 0.58). This novel haplotype contained minor and protective alleles concerning AIH susceptibility.
Alignments of Bases (A) and Amino Acids (B) of Exon 14 in PTPN22. SNPs in bold type are polymorphic. 1; rs554195846 (A/G: Thr/Thr), 2; rs138223016 (C/A: Ala/Ser), 3; rs765535869 (C/T: Arg/Arg), 4; rs759881801 (T/C: Ile/Met), 5; rs764275349 (G/A: Pro/Leu), 6; rs2476601 (G/T: Arg/Trp), 7; rs201811041 (C/T: Arg/Gln), 8; rs74163660 (C/G: Pro/Arg), 9; rs768160390 (A/G: Ire/Thr), 10; rs368086285 (C/T: Val/Met), 11; rs775140391 (A/G: Val/Ala), 12; rs569454620 (C/T: Ala/Thr).
Although various autoimmune disorders have been associated with rs2476601, negligible relationships were found for systemic sclerosis, celiac disease, ulcerative colitis, Crohn’s disease, multiple sclerosis, and psoriasis in a meta-analysis31. The study defined two groups of diseases with regard to their targeted tissues, and showed that most autoimmune diseases possessing an insignificant association with rs2476601 manifested in the skin, gastrointestinal tract, bile duct, or immune privileged sites. Such results indicated that the relationship of individual PTPN22 SNPs with autoimmune diseases depended on the localization of the affected tissues and suggested a role of targeted organ variation in disease manifestations. Regarding autoimmune liver disease, only one association study on PBC has been conducted that showed no relationship with rs2476601 in Canada32. No genome-wide association studies have demonstrated a link between PTPN22 and PBC susceptibility10,11,12,33,34, which was supported by our data. PBC is characterized by slow, progressive destruction of the small bile ducts within the liver. Primary sclerosing cholangitis is another autoimmune disease targeting the bile ducts that is complicated by ulcerative colitis. Primary sclerosing cholangitis was also not associated with SNPs in rs247660135. Interestingly, we witnessed that haplotypes containing the rs3765598 T allele were significantly associated with a 0.6 times less likelihood to develop PBC, which suggested that this haplotype may play an important role in protection from PBC in Japan. The limitations of this study are a small number of cases and controls and a narrow focus on few SNPs in this era of genome-wide association studies. Further investigation is needed to validate this association in other Asian countries.
In conclusion, the present study revealed PTPN22 gene SNP and haplotype associations with protection against AIH or PBC in a Japanese population. This gene may therefore play a crucial role in the pathogenesis of Japanese autoimmune liver disease, and further studies are warranted to clarify its role in AIH and PBC.
Patients and Methods
Subjects
The clinical and biochemical features of the 166 patients with AIH and 262 patients with PBC enrolled in this study between January 2001 and August 2015 are summarized in Table 5. We also recruited 322 volunteer control subjects from hospital staff who had indicated the absence of any major illnesses in a standard questionnaire. The racial background of all individuals was Japanese. All AIH patients had been diagnosed according to the scoring system of the International Autoimmune Hepatitis Group36 and were classified as having type 1 AIH based on antibody profiles. The diagnosis of PBC was made according to criteria from the American Association for the Study of Liver Diseases37. Anti-nuclear antibody titers were determined by immunofluorescence using HEp-2 cells, for which a titer of ≥1:80 was considered a positive result38. Anti-mitochondrial antibody-M2 was measured by the enzyme-linked immunosorbent assay as reported previously8. All patients were negative for the hepatitis B surface antigen and antibodies to the hepatitis B core antigen, hepatitis C virus, and human immunodeficiency virus. Overlap syndromes were excluded. Liver cirrhosis was diagnosed by histological examination and/or characteristic clinical signs of advanced liver disease39. This study was reviewed and approved by the Institutional Review Board of Shinshu University Hospital (Matsumoto, Japan), and written informed consent was obtained from all participating subjects. The investigation was conducted according to the principals of the Declaration of Helsinki.
PTPN22 Genotyping
Genomic DNA from patients and controls was isolated from whole blood samples using QuickGene-800 assays (Fujifilm, Tokyo, Japan).
We evaluated nine SNPs (rs1217412, rs1217388, rs2476601, rs1217407, rs3765598, rs33996649, rs2488458, rs3789612, and rs2488457) spanning a 58 kb region in the PTPN22 gene. The SNPs were selected from previous reports14,15,19,22 and had minor allele frequencies of >5% according to HapMap Japanese data (http://hapmap.ncbi.nlm.nih.gov/). Genotyping of all SNPs was performed with a TaqMan 5′ exonuclease assay using primers supplied by Applied Biosystems (Foster City, CA, USA). The probe’s fluorescence signals were detected with the StepOne Plus Real-Time PCR System (Applied Biosystems) according to the manufacturer’s instructions.
Statistical Analysis
Allele, genotype, and haplotype frequencies along with Hardy-Weinberg equilibrium and LD were assessed using SNPStats software (Catalan Institute Oncology, Barcelona, Spain; http://bioinfo.iconcologia.net/SNPstats)40 and Haploview 4.1 software41. For analysis of genotype data, we adopted the multiple inheritances model to assess each minor allele, including codominant 1 (AB vs. BB, assuming that A is the minor allele), codominant 2 (AA vs. BB), dominant (AA+AB vs. BB), recessive (AA vs. AB+BB), over-dominant (AB vs. AA+BB), and log-additive (AA vs. AB vs. BB) models. Akaike’s information criterion was used to determine the most suitable inheritance model42. P values were subjected to Bonferroni correction by multiplication by the number of different SNPs. A P value of less than 0.05 was considered to be statistically significant.
Additional Information
How to cite this article: Umemura, T. et al. Genetic Association of PTPN22 Polymorphisms with Autoimmune Hepatitis and Primary Biliary Cholangitis in Japan. Sci. Rep. 6, 29770; doi: 10.1038/srep29770 (2016).
References
Krawitt, E. L. Autoimmune hepatitis. N Engl J Med. 354, 54–66 (2006).
Heneghan, M. A., Yeoman, A. D., Verma, S., Smith, A. D. & Longhi, M. S. Autoimmune hepatitis. Lancet. 382, 1433–1444 (2013).
Kaplan, M. M. & Gershwin, M. E. Primary biliary cirrhosis. N Engl J Med. 353, 1261–1273 (2005).
Carey, E. J., Ali, A. H. & Lindor, K. D. Primary biliary cirrhosis. Lancet. 386, 1565–1575 (2015).
Seki, T. et al. HLA class II molecules and autoimmune hepatitis susceptibility in Japanese patients. Gastroenterology. 103, 1041–1047 (1992).
Umemura, T. et al. Human leukocyte antigen class II haplotypes affect clinical characteristics and progression of type 1 autoimmune hepatitis in Japan. PLoS One. 9, e100565 (2014).
Umemura, T. et al. Human leukocyte antigen class II molecules confer both susceptibility and progression in Japanese patients with primary biliary cirrhosis. Hepatology. 55, 506–511 (2012).
Joshita, S. et al. Association analysis of cytotoxic T-lymphocyte antigen 4 gene polymorphisms with primary biliary cirrhosis in Japanese patients. J Hepatol. 53, 537–541 (2010).
Umemura, T. et al. Association of cytotoxic T-lymphocyte antigen 4 gene polymorphisms with type 1 autoimmune hepatitis in Japanese. Hepatol Res. 38, 689–695 (2008).
Hirschfield, G. M. et al. Variants at IRF5-TNPO3, 17q12-21 and MMEL1 are associated with primary biliary cirrhosis. Nat Genet. 42, 655–657 (2010).
Liu, X. et al. Genome-wide meta-analyses identify three loci associated with primary biliary cirrhosis. Nat Genet. 42, 658–660 (2010).
Mells, G. F. et al. Genome-wide association study identifies 12 new susceptibility loci for primary biliary cirrhosis. Nat Genet. 43, 329–332 (2011).
de Boer, Y. S. et al. Genome-wide association study identifies variants associated with autoimmune hepatitis type 1. Gastroenterology. 147, 443–452 e445 (2014).
Bottini, N. et al. A functional variant of lymphoid tyrosine phosphatase is associated with type I diabetes. Nat Genet. 36, 337–338 (2004).
Begovich, A. B. et al. A missense single-nucleotide polymorphism in a gene encoding a protein tyrosine phosphatase (PTPN22) is associated with rheumatoid arthritis. Am J Hum Genet. 75, 330–337 (2004).
Ladner, M. B., Bottini, N., Valdes, A. M. & Noble, J. A. Association of the single nucleotide polymorphism C1858T of the PTPN22 gene with type 1 diabetes. Hum Immunol. 66, 60–64 (2005).
Hinks, A. et al. Association between the PTPN22 gene and rheumatoid arthritis and juvenile idiopathic arthritis in a UK population: further support that PTPN22 is an autoimmunity gene. Arthritis Rheum. 52, 1694–1699 (2005).
Orozco, G. et al. Association of a functional single-nucleotide polymorphism of PTPN22, encoding lymphoid protein phosphatase, with rheumatoid arthritis and systemic lupus erythematosus. Arthritis Rheum. 52, 219–224 (2005).
Mori, M., Yamada, R., Kobayashi, K., Kawaida, R. & Yamamoto, K. Ethnic differences in allele frequency of autoimmune-disease-associated SNPs. J Hum Genet. 50, 264–266 (2005).
Ban, Y., Tozaki, T., Taniyama, M., Tomita, M. & Ban, Y. The codon 620 single nucleotide polymorphism of the protein tyrosine phosphatase-22 gene does not contribute to autoimmune thyroid disease susceptibility in the Japanese. Thyroid. 15, 1115–1118 (2005).
Kawasaki, E. et al. Systematic search for single nucleotide polymorphisms in a lymphoid tyrosine phosphatase gene (PTPN22): association between a promoter polymorphism and type 1 diabetes in Asian populations. Am J Med Genet A. 140, 586–593 (2006).
Ikari, K. et al. Haplotype analysis revealed no association between the PTPN22 gene and RA in a Japanese population. Rheumatology (Oxford). 45, 1345–1348 (2006).
Thomson, W. et al. Rheumatoid arthritis association at 6q23. Nat Genet. 39, 1431–1433 (2007).
Barrett, J. C. et al. Genome-wide association study and meta-analysis find that over 40 loci affect risk of type 1 diabetes. Nat Genet. 41, 703–707 (2009).
Tomer, Y. et al. Genome wide identification of new genes and pathways in patients with both autoimmune thyroiditis and type 1 diabetes. J Autoimmun. 60, 32–39 (2015).
Orru, V. et al. A loss-of-function variant of PTPN22 is associated with reduced risk of systemic lupus erythematosus. Hum Mol Genet. 18, 569–579 (2009).
Fiorillo, E. et al. Autoimmune-associated PTPN22 R620W variation reduces phosphorylation of lymphoid phosphatase on an inhibitory tyrosine residue. J Biol Chem. 285, 26506–26518 (2010).
Feng, X. et al. Association of the PTPN22 gene (-1123G > C) polymorphism with rheumatoid arthritis in Chinese patients. Tissue Antigens. 76, 297–300 (2010).
Huang, J. J. et al. A PTPN22 promoter polymorphism -1123G>C is associated with RA pathogenesis in Chinese. Rheumatol Int. 32, 767–771 (2012).
Huang, C. H. et al. Associations of the PTPN22 and CTLA-4 genetic polymorphisms with Taiwanese ankylosing spondylitis. Rheumatol Int. 34, 683–691 (2014).
Zheng, J., Ibrahim, S., Petersen, F. & Yu, X. Meta-analysis reveals an association of PTPN22 C1858T with autoimmune diseases, which depends on the localization of the affected tissue. Genes Immun. 13, 641–652 (2012).
Milkiewicz, P. et al. The PTPN22 1858T variant is not associated with primary biliary cirrhosis. Tissue Antigens. 67, 434–437 (2006).
Nakamura, M. et al. Genome-wide association study identifies TNFSF15 and POU2AF1 as susceptibility loci for primary biliary cirrhosis in the Japanese population. Am J Hum Genet. 91, 721–728 (2012).
Cordell, H. J. et al. International genome-wide meta-analysis identifies new primary biliary cirrhosis risk loci and targetable pathogenic pathways. Nat Commun. 6, 8019 (2015).
Viken, M. K. et al. Association analysis of the 1858C>T polymorphism in the PTPN22 gene in juvenile idiopathic arthritis and other autoimmune diseases. Genes Immun. 6, 271–273 (2005).
Alvarez, F. et al. International Autoimmune Hepatitis Group Report: review of criteria for diagnosis of autoimmune hepatitis. J Hepatol. 31, 929–938 (1999).
Lindor, K. D. et al. Primary biliary cirrhosis. Hepatology. 50, 291–308 (2009).
Umemura, T. et al. Immunoglobin G4-hepatopathy: association of immunoglobin G4-bearing plasma cells in liver with autoimmune pancreatitis. Hepatology. 46, 463–471 (2007).
Umemura, T. et al. Serum Wisteria floribunda Agglutinin-Positive Mac-2-Binding Protein Level Predicts Liver Fibrosis and Prognosis in Primary Biliary Cirrhosis. Am J Gastroenterol. 110, 857–864 (2015).
Sole, X., Guino, E., Valls, J., Iniesta, R. & Moreno, V. SNPStats: a web tool for the analysis of association studies. Bioinformatics. 22, 1928–1929 (2006).
Barrett, J. C., Fry, B., Maller, J. & Daly, M. J. Haploview: analysis and visualization of LD and haplotype maps. Bioinformatics. 21, 263–265 (2005).
Akaike, H. A new look at the statistical model iddentification. IEEE Transactions on Automatic Control. 19, 716–723 (1974).
Acknowledgements
This work was supported by Japan Society for the Promotion of Science KAKENHI Grant Number 26460996. The authors thank Yuki Akahane and Asami Yamazaki for their technical assistance and Trevor Ralph for his editorial assistance.
Author information
Authors and Affiliations
Contributions
T.U. and M.O. conceived and designed the experiments. Y.K. performed the experiments. T.U., Y.K. and M.O. analyzed the data. T.U., T.Y., S.J., M.K., K.Y. and E.T. contributed reagents, materials, and analytic tools. T.U. and M.O. wrote the manuscript. All the authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Umemura, T., Joshita, S., Yamazaki, T. et al. Genetic Association of PTPN22 Polymorphisms with Autoimmune Hepatitis and Primary Biliary Cholangitis in Japan. Sci Rep 6, 29770 (2016). https://doi.org/10.1038/srep29770
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep29770
This article is cited by
-
The Asian Pacific Association for the Study of the Liver clinical practice guidance: the diagnosis and management of patients with autoimmune hepatitis
Hepatology International (2021)
-
No association of HLA–DRB1 and TNF alleles in Mexican patients with autoimmune hepatitis
Genes & Immunity (2019)
-
Role of deleterious single nucleotide variants in the coding regions of TNFAIP3 for Japanese autoimmune hepatitis with cirrhosis
Scientific Reports (2019)
-
Serum Autotaxin Is a Useful Disease Progression Marker in Patients with Primary Biliary Cholangitis
Scientific Reports (2018)
-
A cis-eQTL of HLA-DPB1 Affects Susceptibility to Type 1 Autoimmune Hepatitis
Scientific Reports (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.