Abstract
The intensity of left atrial spontaneous echo contrast (LASEC) by transesophageal echocardiography (TEE) has been proposed as an important variable in the stratification of thromboembolic risk, particularly in patients with nonvalvular atrial fibrillation (NVAF). We hypothesized that the quantification of LASEC by ultrasound will improve its utility in predicting subsequent stroke events in patients with NVAF. Patients (n = 206) with definite NVAF receiving TEE were included for this prospective cohort study. Baseline clinical risk factors of stroke, CHADS2 score and CHA2DS2-Vasc, left atrial thrombus (LAT), the five-grades of LASEC and video intensity (VI) value of LASEC were measured. During 2 years follow-up, 20 patients (9.7%) developed stroke. VI value of LASEC in the patients with stroke was higher compared to patients without stroke (25.30 ± 3.61 vs. 8.65 ± 0.81, p < 0.001). On logistic regression analysis, LAT, qualitative LASEC, graded LASEC, VI value of LASEC and CHADS2 and CHA2DS2-Vasc score were independent predictors of stroke. Among them, the highest area under the curve of receiver operating characteristic (ROC) in predicting stroke was VI value of LASEC (p < 0.05). These results show that quantification of LASEC by VI value is the most favorable predictor of stroke in patients with NVAF, and calls for improving the utility of LASEC in predicting subsequent stroke events.
Similar content being viewed by others
Introduction
Nonvalvular atrial fibrillation (NVAF) is a major risk factor for stroke and systemic embolism1,2. The estimated prevalence of atrial fibrillation (AF) in the United States is 2.7 million to 6.1 million3,4. Risk stratification schemes such as the CHADS2 (congestive heart failure, hypertension, age ≥75 years, diabetes mellitus, stroke) and CHA2DS2-Vasc (congestive heart failure, hypertension, age ≥75 years, diabetes mellitus, stroke, vascular disease, age 65–74 years, sex category) have been proposed for identification of NVAF patients at higher thromboembolic risk and are more likely to achieve net clinical benefit from anticoagulation5. However, these score has the limitation of classifying excessive number NVAF patients as at intermediate risk6.
Thrombogenic milieu in the left atrium (LA) is an important factor in the pathogenesis of NVAF-related thromboembolic events7. Presence of thrombus, smoke, or sludge in the LA, and decreased LA appendage emptying velocity has been reported as predictors of systemic embolic events8,9,10. Left atrial spontaneous echo contrast (LASEC) has been a common phenomenon that is detected by transesophageal echocardiography (TEE) in patients with NVAF11. Its formation is attributed to abnormal blood stasis, abnormal hemostasis, platelets, and fibrinolysis12 which are all recognized by Virchow’s triad as the pathogenesis of thrombus formation in AF13. Thus, LASEC has received increasing attention as a marker of thromboembolic risk in NVAF9. Not merely the presence or absence, but also the severity of LASEC by semi-quantitative assessment has been proven to be associated with stroke events in patients with NVAF14,15. While a few studies have attempted to correlate semi-quantitative LASEC (five-grade method) with quantitative video intensity (VI) measurements, the semi-quantitative assessment is largely subjective, influenced by the experience of the operator. Furthermore, there have been no studies to date examining the utility of a quantitative method to evaluate the severity of LASEC in predicting stroke events. Therefore, in this study, we quantified the severity of LASEC with VI value using color-coded technology. Our goal was to prospectively determine the VI value of LASEC as a quantitative stratification method, on the subsequent occurrence of stroke events in patients with NVAF.
Results
Patient population and baseline characteristics
Among the 780 recruited patients, 246 were enrolled in the cohort study based on exclusion criteria. Of 246, 24 patients were lost to follow-up and 16 patients had incomplete data, leaving 206 patients available for analysis (Fig. 1). Table 1 presents the demographic data and clinical characteristics of the patients. Patients in each group were similar with respect to age, gender, and prevalence of hypertension, diabetes, hyperlipidemia and smoking. Twenty patients developed stroke during the 2 years follow-up. Patients who developed stroke had a higher detection rate of LASEC (75% vs. 36.6%, p = 0.001) and left atrial thrombus (LAT) (35% vs. 5.4%, p < 0.001), and higher CHADS2 score (1.5 ± 1.1 vs. 0.87 ± 0.85; p = 0.022, 95% CI 0.10 to 1.16) and CHA2DS2-Vasc (2.65 ± 1.42 vs.1.58 ± 1.25; p < 0.001, 95% CI 0.49 to 1.66).
Among the 206 patients, left atrial thrombus (LAT) was observed in 7 patients with stroke and in 10 without stroke, all of those patients received anticoagulation after the TEE study, if they had not before. Anticoagulation therapy was unchanged in patients without a LAT.
Quantification of LASEC with color-coding and VI value
Examples of 5 grades of LASEC with the use of color-coded method or not are shown in Fig. 2a. Obviously, by using the color-coded method, differences between five grades of LASEC was more visible. There were 123 patients with grade 0, 38 patients with grade 1, 21 patients with grade 2, 13 patients with grade 3, and 11 patients with grade 4, respectively.
Figure 2b shows the VI value of each grade of LASEC. A strong correlation was observed between the quantitative parameter (VI value) and the semi-quantitative grading of LASEC (r2 = 0.857, p < 0.001). From grade 0 to grade 4, the mean VI value was 3.33 ± 2.07 (95% CI 2.96 to 3.96), 9.84 ± 3.98 (95% CI 8.54 to 11.15), 19.71 ± 5.14 (95% CI 17.37 to 22.05), 29.77 ± 7.08 (95% CI 25.05 to 34.04), and 48.27 ± 11.87 (95% CI 40.3 to 56.24), respectively. One-way ANOVA with multiple comparisons showed that there were significant differences in VI value among each grade of LASEC (p < 0.05).
Relation between stroke incidence and grades of LASEC, or its VI value
To understand how LASEC influences stroke risk, we first examined the stroke incidence rates for five grades of LASEC. In participants without LASEC (grade 0), stroke incidence was low (4.1%; Fig. 3a). Stroke incidence significantly increased with the severity of LASEC (7.9% for grade1, 14.3% for grade 2, and 30.8% for grade 3, respectively), reaching an incidence rate of 45.5% for grade 4 (Fig. 3a). The distribution of VI value in the stroke and non-stroke groups is illustrated in Fig. 3b. The stroke group was found to have a tendency toward higher VI values (25.30 ± 3.61 vs. 8.65 ± 0.81, p < 0.001, 95% CI 8.96 to 24.33).
Independent predictors of stroke
Multivariate logistic regression analysis was performed to determine the relative importance of independent predictors of stroke (Table 2). Multiple candidate clinical predictors and echocardiography measurements were assessed as univariate independent predictors for stroke. Qualitative LASEC (p = 0.014, OR 6.59, 95% CI 1.46 to 29.71), LAT (p = 0.007, OR 6.28, 95% CI 1.66 to 23.79) and VI value of LASEC (p = 0.002, OR 1.09, 95% CI 1.03 to 1.15) were independent predictors of stroke. For graded LASEC, grade 3 (p = 0.004, OR 45.32, 95% CI 3.37 to 608.69) and grade 4 (p = 0.002, OR 157.98, 95% CI 6.05 to 4127.14) also were independently predictive of stroke, but grade 0 to 2 were not. For CHADS2, model 1 did not show that the CHADS2 was an independent predictor of stroke (p = 0.09). Both the CHADS2 and a subgroup of a high CHADS2 score of 3 were noted as an independently predictive of stroke (p = 0.044), when LASEC was taken into consideration. If considering CHA2DS2-Vasc instead of CHADS2, the results of multivariate logistic regression analysis was similar to CHADS2 (Supplementary Table S1).
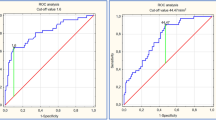
Receiver operating characteristic (ROC) curves
Figure 4 displays the ROC curves of VI value of LASEC, graded LASEC, CHA2DS2-Vasc, qualitative LASEC, LAT and CHADS2 in predicting stroke in patients with NVAF. It shows the superiority of the VI value at predicting stroke compared to the other data (p < 0.05). The sensitivity of VI value in predicting stroke was 80%, while the specificity was 76.3% with a cutoff value of 11.5. The area under the curve was 0.844 with a standard error of 0.041 (Table 3). For graded LASEC, CHA2DS2-Vasc, qualitative LASEC, CHADS2, and LAT, the area under the curve was 0.754, 0.720, 0.692, 0.668 and 0.648, respectively.
Discussion
The present study is the first of its kind to demonstrate that quantification of LASEC by VI value can predict stroke events and that it is an independent predictor of stroke in NVAF patients. Previous studies have evaluated the predictive value of LASEC based on its presence or not. In a prospective study of patients with NVAF, Sydney et al. observed an annual stroke event rate of 9% in patients with LASEC, as compared to only 3% in patients without LASEC9. Similar to our results, the stroke patients had a significant higher incidence of LASEC than the non-stroke patients. However, the intensity of LASEC may vary continuously, from sparse and barely perceptible to dense, and the magnitude of thromboembolic risk may also vary with the severity of LASEC15,16. Thus it became apparent that there is a strong correlation between stroke event rate and the severity of LASEC17,18. This was further corroborated by the development of semi-quantitative methods, including the three-grade method as Beppu et al. proposed and the five-grade method as Fatkin et al. proposed16,19. Their results revealed that denser LASEC was accompanied by a higher risk of left atrial appendage thrombus formation in patients with NVAF. In the current study, we independently demonstrated the stroke risk of five grades of LASEC, and found a strong positive correlation between the severity of LASEC and stroke incidence.
Fatkin et al. had correlated five-grades of LASEC with quantitative VI measurements, and based on their results, we proposed that quantification of LASEC severity could predict stroke outcome in NVAF patients. However, considering that the classification of LASEC into discrete grades of increasing severity may be somewhat arbitrary because of the continuous nature of LASEC (reflected by echogenicity in the LA), and that the semi-quantitative assessment was largely influenced by the experience of the operator14, we quantified the severity of LASEC with VI value using color-coded technology. This method allowed us to prospectively determine the VI value of LASEC, as a quantitative stratification method, on the subsequent occurrence of stroke events in patients with NVAF. Compared with the five-grades of LASEC, we found that VI value is a better quantitative method to evaluate the severity of LASEC. More importantly, color-coded images and VI data were all acquired from the software, thus it should be more objective.
The effect of CHADS2 on predicting stroke was not significant when the LASEC variable was excluded in our present study, whereas when all variables were included, CHADS2 was noted as an independent predictor of stroke. This might be due to the relative small number of patients, particularly on the shortage of the patient with high CHADS2 score of 4. Nevertheless, it is well established that the CHADS2 score is a simple clinical prediction rule for estimating the risk of stroke in patients with NVAF. A high CHADS2 score corresponds to a greater risk of stroke, while a low CHADS2 score corresponds to a lower risk of stroke. The CHADS2 score has been validated by many studies. However, the CHADS2 score may not always be a good predictor of stroke risk, especially in intermediate risk patients and patients with relatively low scores5. In our current study, there was no significance achieved in predicting stroke by a CHADS2 score ≤2 even all variables included. Earlier reports indicate that in patients with non-valvular AF and a low CHADS2 score of 0 or 1, the prevalence of LAT was 3%20. Yet, in another study, 10% of persistent AF patients had LAT confirmed by TEE, and 77% of the patients with LAT had a CHADS2 score ≤218. Thus, further risk stratification is warranted in these “low to intermediate risk” patients according to the CHADS2 score. Our results reveal that the stroke prediction ability of VI value was better than the CHADS2 score in patients with NVAF, especially with low to intermediate risk CHADS2 score patients. Our study also reveals the similar results with the CHA2DS2-Vasc score.
Estimating the risk of stroke for individual NVAF patients is crucial in the decision making to provide anticoagulation therapy. While identification of stroke risk in AF is a continuum, prior qualitative or semi-quantitative stroke risk stratification schemes have been used to “artificially” categorize patients into low, moderate, and high risk stroke strata21. thereby allowing inherent mistakes in the definition of the real low or high risk patients. On the contrary, the intensity of LASEC reflected by VI value is a continuous variable that may fulfill the demand of continuous assessment of stroke risk22. In our study, the quantification of LASEC provided important incremental value in predicting stroke events compared to the CHADS2. In addition, our quantitative method is objective and was not affected by the experience of the operators. Despite the potential for LASEC to identify stroke events, this aspect has not been taken into account in stroke risk stratification. Because CHADS2 score is easy, safe and can be widely adopted, we propose that CHADS2 should be used for all patients with NVAF to define the “high risk” group. Subsequently, for the “low to intermediate risk” patients, we suggest the use of TEE to screen for LASEC, which will further confirm whether an anticoagulant therapy is warranted or not.
Study limitations
This study was performed in a single dedicated AF ablation center. Therefore, a selection bias could be attributed to the findings, and is a recognized limitation of our study. In addition, the number of patients was relatively small and the follow-up period was relatively short. Thus, a larger multi-center trial with longer follow-up data on stroke event rates is required to validate the usefulness of VI value of LASEC in categorizing the stroke risk in patients with NVAF. Patients with factors that would affect the hemostasis were not included in the study. It is known that hemostasis associated factors, such as fibrinogen level, hematocrit and blood flow, could affect LASEC to a large extent, so the validity of our method in those patient populations is unknown. Furthermore, we did not compare VI value with other quantitative measures due to the lack of an adequate gold standard to assess LASEC severity. Finally, we could not distinguish between paroxysmal and persistent/permanent NVAF, but previous studies suggest that the risk of stroke is similar in these subgroups23.
Conclusions
Quantification of the severity of LASEC with VI value using color-coded technology can improve the predictive ability of LASEC for subsequent stroke events in patients with NVAF. Quantification of LASEC by VI value emerged as the most favorable predictor of stroke; it further identifies the patients who are more likely to undergo aggressive anticoagulant therapy following a high VI value LASEC study. Validation of current findings in a prospective multicenter study with a larger number of patients is required.
Methods
This study was performed and reported according to the 2010 Statement of Consolidated Standards of Reporting Trials (CONSORT)24.
Ethical Issues
The study protocol was approved by the ethics committee of Nanfang Hospital in Guangzhou. All study participants provided written informed consent. The methods were carried out in accordance with relevant guidelines and regulations.
Study design and population
This prospective cohort study was conducted during September 2008 to September 2014 at the Nanfang Hospital (Guangzhou, China), a more than 2000 bedded, accredited tertiary care center providing state of the art health care facilities. A total of 780 patients with a diagnosis of NVAF receiving TEE were recruited by searching automated inpatient during September 2008 to September 2012. AF was confirmed by a 12-lead surface electrocardiogram and Holter within a week prior to and during the TEE examination. To reduce the potential selection bias, the exclusion criteria were strictly control. Inclusion criteria were consecutive patients with NVAF undergoing clinically indicated TEE. Exclusion criteria included: (1) a history of rheumatic and congenital heart disease, (2) deep vein thrombosis, (3) patients with mechanical valve, (4) patients with carotid artery plaque, (5) recent (less than four weeks) oral anticoagulant or heparin usage, or (6) patients with conditions such as recent surgery, infection or malignancy, which were likely to affect hemostasis. In addition, patients who underwent radiofrequency ablation or valve replacement surgery after the enrollment were excluded. The cohort was followed up through September 2014, a median follow-up of 2 years (interquartile range 1.4–2.0 years). The follow-up would be ended, if a patient developed stroke. Follow-up information was primarily obtained by telephone interviews.
Outcomes at follow-up
The primary endpoint in this study was defined as incident stroke events during follow-up. The diagnoses were recorded using the National Stroke Association scoring criteria (1995): focal neurological symptoms persist for 24 h or more, or presence of ischemic or hemorrhagic lesions confirmed using CT or MRI.
Clinical risk factors of stroke and CHADS2 and CHA2DS2-Vasc score
During hospitalization we obtained clinical parameters comprised age, gender, smoking, history of hypertension, heart failure, diabetes, and anticoagulant or antiplatelet therapy. Laboratory test results included fibrinogen, C-reactive protein, brain natriuretic peptide, uric acid, low-density lipoprotein, etc. Variables required to calculate the CHADS2 score included age ≥75 years (1), congestive heart failure (1), hypertension (1), diabetes mellitus (1), and stroke/transient ischemic attack (2)25, and the CHA2DS2-Vasc score included Congestive heart failure (1), Hypertension (1), Age ≥75 (2), Diabetes (1), prior Stroke (2), Vascular disease (1), Age 65–74 (1), Sex category (1)25.
Echocardiography
All patients subsequently underwent transthoracic echocardiography (TTE) and TEE with a Siemens Acuson ultrasound system (Siemens Medical Solutions USA, Inc.). For TTE, a 1.7/3.4-MHz harmonic transducer was used. TEE was performed with a 6.7-MHz multiplane V5Ms transducer, as previously reported17. Although higher frequency is associated with more “LASEC”, all images from patients undergoing TEE were recorded at a unified frequency of 6.7 MHz and other ultrasonic parameters were constant through all studies. Measurements were performed off line with syngo® software provided by the manufacturer.
A standardized TTE examination, including the standard imaging planes was performed according to the recommendations of the American Society of Echocardiography26. Left ventricular ejection fraction was calculated using the Simpson method, and the left atrial diameter was measured in the M mode. Mitral valve E wave peak velocity was also measured and analyzed.
TEE was performed in the standard manner27,28,29. Written consent was obtained from all patients. Fasting for at least four hours prior to the examination was required for all patients undergoing TEE. Topical lidocaine spray was used for local anesthesia of the oropharynx and if needed, a light sedation with 2.5–5.0 mg midazolam was given intravenously. The LA and its appendage were closely inspected for the presence of LASEC and thrombi by adjustment of the gain settings to an optimised state, which just to be able to distinguish LASEC from electronic background noise. In order to standardise the detection of LASEC in different degrees, overall gain and compress settings were varied throughout their full range. Acoustic frequency and other settings were constant during each study16,18. Echocardiographic measurements were performed by two independent observers assessing the off-line digitized images. The images were displayed in random order without clinical information of the patient. Inter-observer differences were reconciled by a third observer.
The degree of LASEC was categorized as being either absent (0), mild (1+), mild to moderate (2+), moderate (3+), or severe (4+), on the basis of a grading system described by Fatkin et al.16 Additionally, color-coded images were acquired by offline image analysis software (MCE version 2.7, University of Virginia, USA) according to the LASEC background subtracted signal placed over the aorticroot, following VI quantification of SEC signal within the region of interest.
Statistical analysis
The sample size was calculated by taking into account the objectives of the study. Continuous variables were analyzed using independent-Sample t tests or one-way ANOVA. Chi-square or Fisher's exact tests were used for categorical variables. Bivariate correlation or logistic regression was performed, and ROC curves generated to compare the predictive power of different stroke stratification methods in the study. All tests were two tailed, and a p-value < 0.05 was considered statistically significant. Analyses were performed using SPSS software program version 13.0 (SPSS Inc., Chicago, IL, USA).
Additional Information
How to cite this article: Zhao, Y. et al. Intensity of Left Atrial Spontaneous Echo Contrast as a Correlate for Stroke Risk Stratification in Patients with Nonvalvular Atrial Fibrillation. Sci. Rep. 6, 27650; doi: 10.1038/srep27650 (2016).
References
Wolf, P. A., Abbott, R. D. & Kannel, W. B. Atrial fibrillation as an independent risk factor for stroke: the Framingham Study. Stroke. 22, 983–988 (1991).
Tu, H. T. et al. Pathophysiological determinants of worse stroke outcome in atrial fibrillation. Cerebrovasc Dis. 30, 389–395 (2010).
Hannon, N. et al. Stroke associated with atrial fibrillation–incidence and early outcomes in the north Dublin population stroke study. Cerebrovasc Dis. 29, 43–49 (2010).
Wann, L. S. et al. 2011 ACCF/AHA/HRS focused update on the management of patients with atrial fibrillation (update on dabigatran): a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. J Am Coll Cardiol. 57, 1330–1337 (2011).
Fang, M. C. et al. Comparison of risk stratification schemes to predict thromboembolism in people with nonvalvular atrial fibrillation. J Am Coll Cardiol. 51, 810–815 (2008).
Rietbrock, S., Heeley, E., Plumb, J. & van Staa, T. Chronic atrial fibrillation: Incidence, prevalence, and prediction of stroke using the Congestive heart failure, Hypertension, Age >75, Diabetes mellitus, and prior Stroke or transient ischemic attack (CHADS2) risk stratification scheme. Am Heart J. 156, 57–64 (2008).
Thambidorai, S. K. et al. Utility of transesophageal echocardiography in identification of thrombogenic milieu in patients with atrial fibrillation (an ACUTE ancillary study). Am J Cardiol. 96, 935–941 (2005).
Zabalgoitia, M. et al. Transesophageal echocardiographic correlates of clinical risk of thromboembolism in nonvalvular atrial fibrillation. Stroke Prevention in Atrial Fibrillation III Investigators. J Am Coll Cardiol. 31, 1622–1626 (1998).
Leung, D. Y., Black, I. W., Cranney, G. B., Hopkins, A. P. & Walsh, W. F. Prognostic implications of left atrial spontaneous echo contrast in nonvalvular atrial fibrillation. J Am Coll Cardiol. 24, 755–762 (1994).
Transesophageal echocardiographic correlates of thromboembolism in high-risk patients with nonvalvular atrial fibrillation. The Stroke Prevention in Atrial Fibrillation Investigators Committee on Echocardiography. Ann Intern Med. 128, 639–647 (1998).
Chimowitz, M. I., DeGeorgia, M. A., Poole, R. M., Hepner, A. & Armstrong, W. M. Left atrial spontaneous echo contrast is highly associated with previous stroke in patients with atrial fibrillation or mitral stenosis. Stroke. 24, 1015–1019 (1993).
Black, I. W. et al. Hematologic correlates of left atrial spontaneous echo contrast and thromboembolism in nonvalvular atrial fibrillation. J Am Coll Cardiol. 21, 451–457 (1993).
Watson, T., Shantsila, E. & Lip, G. Y. Mechanisms of thrombogenesis in atrial fibrillation: Virchow’s triad revisited. Lancet. 373, 155–166 (2009).
Klein, A. L. et al. Integrated backscatter for quantification of left atrial spontaneous echo contrast. J Am Coll Cardiol. 28, 222–231 (1996).
Fatkin, D. & Feneley, M. P. Qualitative or quantitative assessment of spontaneous echo contrast? J Am Coll Cardiol. 29, 222–224 (1997).
Fatkin, D., Loupas, T., Jacobs, N. & Feneley, M. P. Quantification of blood echogenicity: evaluation of a semiquantitative method of grading spontaneous echo contrast. Ultrasound Med Biol. 21, 1191–1198 (1995).
Bernhardt, P., Schmidt, H., Hammerstingl, C., Luderitz, B. & Omran, H. Patients with atrial fibrillation and dense spontaneous echo contrast at high risk a prospective and serial follow-up over 12 months with transesophageal echocardiography and cerebral magnetic resonance imaging. J Am Coll Cardiol. 45, 1807–1812 (2005).
Vincelj, J., Sokol, I. & Jaksic, O. Prevalence and clinical significance of left atrial spontaneous echo contrast detected by transesophageal echocardiography. Echocardiography. 19, 319–324 (2002).
Beppu, S. et al. Smoke-like echo in the left atrial cavity in mitral valve disease: its features and significance. J Am Coll Cardiol. 6, 744–749 (1985).
Kleemann, T., Becker, T., Strauss, M., Schneider, S. & Seidl, K. Prevalence and clinical impact of left atrial thrombus and dense spontaneous echo contrast in patients with atrial fibrillation and low CHADS2 score. Eur J Echocardiogr. 10, 383–388 (2009).
Lip, G. Y. Can we predict stroke in atrial fibrillation? Clin Cardiol. 35, Suppl 1, 21–27 (2012).
Stroke Risk in Atrial Fibrillation Working, G. Comparison of 12 risk stratification schemes to predict stroke in patients with nonvalvular atrial fibrillation. Stroke. 39, 1901–1910 (2008).
Go, A. S. et al. Implications of stroke risk criteria on the anticoagulation decision in nonvalvular atrial fibrillation: the Anticoagulation and Risk Factors in Atrial Fibrillation (ATRIA) study. Circulation. 102, 11–13 (2000).
Schulz, K. F., Altman, D. G., Moher, D. & Group, C. CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Obstetrics and gynecology. 115, 1063–1070 (2010).
Lip, G. Y., Nieuwlaat, R., Pisters, R., Lane, D. A. & Crijns, H. J. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 137, 263–272 (2010).
Henry, W. L. et al. Report of the American Society of Echocardiography Committee on Nomenclature and Standards in Two-dimensional Echocardiography. Circulation. 62, 212–217 (1980).
Agmon, Y., Khandheria, B. K., Gentile, F. & Seward, J. B. Echocardiographic assessment of the left atrial appendage. J Am Coll Cardiol. 34, 1867–1877 (1999).
Omran, H. et al. Left atrial appendage function in patients with atrial flutter. Heart. 78, 250–254 (1997).
Seward, J. B. et al. Multiplane transesophageal echocardiography: image orientation, examination technique, anatomic correlations, and clinical applications. Mayo Clin Proc. 68, 523–551 (1993).
Acknowledgements
This work was supported by the National Basic Research Program of China (973 Program) (No. 2013CB733804), National Natural Science Foundation of China (No. 81227801 and No. 81271640), and the Team Program of Natural Science Foundation of Guangdong Province, China (S2011030003134).
Author information
Authors and Affiliations
Contributions
All of the authors have made important contributions to the study and are thoroughly familiar with the original data. J.B., Y.Z. and J.W. conceived and designed the experiments; J.B., J.L., Y.Z., L.J., X.W., R.J., S.S. and S.G. performed the TEE performance and clinical study; J.B., Y.Z., L.J., X.W., G.C., S.S. and S.G. analyzed the data; J.W., J.B., Y.Z., L.J., Y.W., S.S., S.G., W.L., Y.L. and S.K. wrote the manuscript or revised it critically for important intellectual content; All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Zhao, Y., Ji, L., Liu, J. et al. Intensity of Left Atrial Spontaneous Echo Contrast as a Correlate for Stroke Risk Stratification in Patients with Nonvalvular Atrial Fibrillation. Sci Rep 6, 27650 (2016). https://doi.org/10.1038/srep27650
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep27650
This article is cited by
-
Pathophysiology and clinical relevance of atrial myopathy
Basic Research in Cardiology (2024)
-
Impact of D-dimer for pathologic differentiation on transesophageal echocardiography in embolic stroke of undetermined source: a single-center experience
BMC Neurology (2022)
-
Risk Assessment of Stroke in Patients with Atrial Fibrillation: Current Shortcomings and Future Directions
Cardiovascular Drugs and Therapy (2019)
-
Accuracy of cardiac CT in evaluating severity of left atrial appendage spontaneous echo contrast: comparison with transesophageal echocardiography
The International Journal of Cardiovascular Imaging (2018)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.