Abstract
An important interaction between opioid and dopamine systems has been indicated and using opioids may negatively affect cognitive functioning. Memantine, a medication for Alzheimer's disease, increasingly is being used for several disorders and maybe important for cognitive improvement. Opioid-dependent patients undergoing methadone-maintenance-therapy (MMT) and healthy controls (HCs) were recruited. Patients randomly assigned to the experimental (5 mg/day memantine (MMT+M) or placebo (MMT+P) group: 57 in MMT+M, 77 in MMT+P. Those completed the cognitive tasks at the baseline and after the 12-week treatment were analyzed. Thirty-seven age- and gender-matched HCs and 42 MMT+P and 39 MMT+M patients were compared. The dropout rates were 49.4% in the MMT+P and 26.3% in the MMT+M. Both patient groups' cognitive performances were significantly worse than that of the HCs. After the treatment, both patient groups showed improved cognitive performance. We also found an interaction between the patient groups and time which indicated that the MMT+M group's post-treatment improvement was better than that of the MMT+P group. Memantine, previously reported as neuroprotective may attenuate chronic opioid-dependence-induced cognitive decline. Using such low dose of memantine as adjuvant treatment for improving cognitive performance in opioid dependents; the dose of memantine might be a worthy topic in future studies.
Similar content being viewed by others
Introduction
Chronic psychoactive substance users are associated with a wide variety of neuropsychological impairments, although there is no consensus on whether the impairment are permanent or temporary1,2. The chronic opioid users are associated with dysfunctional frontal networks3, which lead to impaired executive function and attention4. In addition, Baldacchnio et al. (2012)5 reviewed 52 articles relative to studying on how opioid affects neuropsychological function in adult patients with chronic opioid use/dependence using meta-analysis. Their analyses suggested that chronic opioid exposure is associated with impairment across variety of neuropsychological domains, including cognitive flexibility.
Current treatment for opioid dependence in practice remains controversial, although agonist maintenance using methadone or buprenorphine is the treatment of choice6,7. Methadone-maintenance-therapy (MMT) although has been suggested as effective for opioid dependence in retaining opioid-addicts in the treatment rather than buprenorphine8 and may ameliorate some of its cognitive deficits9,10,11,12,13. However, contradictory results have also been reported, viz., that patients on MMT have more neuropsychological impairments than do currently abstinent former opioid abusers14,15. Bracken et al.16 found that opioid-dependent patients on MMT exhibited poor performance in psychomotor speed, selective attention and impulsivity, which implies a cognitive impairment caused by MMT. In addition, after MMT is discontinued, patients may relapse to opioid use17. MMT alone may not be sufficient for treating opioid dependency.
Memantine (M), a non-competitive N-methyl-D-aspartate (NMDA) receptor antagonist, has been used for more than 15 years in Europe to treat a variety of neurological diseases. Relatively recently, it has been widely prescribed (usually ≥ 20 mg/day) to treat moderate-to-severe Alzheimer's disease (AD) because of its reported benefits for people with AD18. Memantine, a widely recognized as NMDA antagonist19,20, but its mechanism of action is not fully understood.
Memantine at higher doses (7.5–20 mg/kg; s.c.) attenuates morphine-induced tolerance, physical dependence and drug-seeking effects in animals21,22, its mechanism was believed to be its ability to antagonize NMDA receptors. Moreover, memantine has also benefits on people who display cognitive decline, including brain tumor23, Parkinson's disease24, alcoholism25 and psychiatric disorders26.
Memantine has been suggested to suppress the development, expression and maintenance of opioid dependence and to reduce morphine self-administration in laboratory animals8,21,27. Afterwards, Bisaga et al.28 had a pilot study to demonstrate the effect of memantine attenuating the expression of opioid withdrawal symptoms and lowering the severity of precipitated withdraw in large dosage (60 mg, PO qid) and very small sample (five opioid-addicts with cross-over design). Although, afterwards, Krupitsky et al.29 demonstrated that memantine significantly reduces the withdrawal symptoms in detoxified opiod-dependents and provided a rationale of using the NMDA antagonist memantine to treat opioid addicts. In their study, they used the initial dose of 10 mg/day was gradually increased to the final dose of 30 mg/day over a period of 1 week. Although, significant effective of memantine in previous studies to reduce withdrawal symptoms and severity of opioid dependence, dose-related adverse effects of memantine have been noticed, including dizziness, restlessness, headache, hallucinations, vomiting, hypertonia and a feeling of pressure within the head30. Using such large dose of memantine in the previous study may be considered another issue in the future.
More recently, a relative lower-dose (0.2 mg/kg) of memantine, abolished morphine-induced conditioned-place-preference behavior in rats because of its N-methyl-D-aspartate (NMDA) receptor antagonist was reported31 for the neuroprotective effects. The dose condition could be a very special and highly original finding which is never reported ever for memantine. The extent of memantine dose in treating opioid-addicts remains unspecific and inconsistent, using such large dosage of memantine similar to Bisaga et al. (2001) and Krupitsky et al. (2002) may not only increase side effects but also confuse the detailed mechanism of medication. Using ultra low dosage might be better to demonstrate the specific effect of the memantine in studying its neuroprotective effect.
Since using large dose may increase side effects and might bias the mechanism of therapeutic effect of using memantine. Previously, an addict-animal model using low dose of memantine was reported the ultra-low dose effect, that addictive behavior was changed (Chen et al., unpublished data). Calculating the dosage in the animal to human, the ultra-dose of 5 mg/day memantine was applied in this study. In this study, we proposed to investigate whether a low dose of memantine would attenuate chronic opioid-induced dependent behavior and have beneficial on cognitive improvement. A double-blind, randomly stratified clinical trial with add-on low dose of memantine (5 mg/day, oral) or placebo in opioid-dependent users undergoing MMT for 12 weeks was conducted. We hypothesized that (a) chronic opioid users had worse cognitive performance compared to the health controls; (b) methadone-maintenance-therapy may delay cognitive decline; (c) methadone-maintenance-therapy add-on low-dose of memantine may improve cognitive performance compared to MMT only. To verify the effects and mechanism of memantine, a double-blind, randomly stratified clinical trial was conducted to investigate the effects of low-dose memantine on chronically opioid-dependent patients' cognitive performance and self-reported health condition undergoing MMT.
Results
Demographic data
At the end of this 12-week follow-up study, 81 opioid-dependent participants (MMT+P: n = 42; MMT+M: n = 39) completed tasks and their data were analyzed (Figure 1). Dropout rates of two experimental groups were 26.3% and 49.4%, respectively. The required methadone dose at baseline was not significantly different between the two MMT groups. However, a urine test revealed significantly more amphetamine users in the MMT+P group than in the MMT+M group (Table 1).
Cognitive performance
The HCs performed significantly better than did the MMT+P and MMT+M participants on all cognitive tasks was found in the HCs (Table 2). After 12-weeks of add-on memantine treatment, a repeated measurement of variance analysis with two factors, Group with two levels (MMT+P and MMT+M) × Time with two levels (baseline and 12 weeks), was done to examine whether there was an interaction between Group and Time for each cognitive index (Table 3).
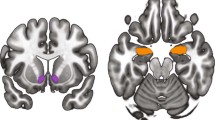
There was a main effect of Time for WCST indices: TNE (F (1, 63) = 14.22, p <0.0005); CLR (F (1, 63) = 17.79, p <0.0005); NCC (F (1, 63) = 11.24, p = 0.001), as well as an interaction between Time and Group in the following indices: TNE (F (1, 63) = 4.39, p = 0.04); CLR (F (1, 63) = 4.16, p = 0.04); NCC (F (1, 63) = 5.19, p = 0.03); TCC (F (1,63) = 4.27, p = 0.04) (Figure 2 (a)–(d)). In addition, for the CPT indices, a significant main effect of Time for the HRT SE T-score (F (1, 69) = 5.89, p = 0.02), Variability T-score (F (1, 69) = 5.37, p = 0.02), HRT ISI Change T-score (F (1,69) = 4.74, p = 0.03) and Hit SE ISI Change T-score (F (1, 69) = 5.89, p = 0.02). There was an interaction between Time and Group for the HRT by Block (F (1, 69) = 5.78, p = 0.02) (Figure 3), but no significant main effect of Group for any cognitive performance index.
Interaction between Group × time in the numbers of total number of errors (TNE), conceptual level response (CLR), number of categories completed (NCC) and trials to complete the first category (TCC) (a) TNE, (b) CLR, (c) NCC and (d) TCC indices of Wisconsin Card Sorting Test (indices of WCST: TNE, total number of errors; CLR, conceptual level response; NCC, number of categories completed; TCC, trials to complete the first category).
Opiate performance index and urinary drug test
After the 12-week MMT treatment, there was no significant difference in the number between the two MMT groups (Table 4). Subsequently, McNemar's test confirmed this result determined using the OTI. The results of the urinary drug test were consistent with the OTI results, that no significantly increase of heroin or other opiate users in the MMT+M group during this 12-week treatment was found. In addition, for the criminality and health indices of the OTI, a trend of improvement was noticed, although not significant (Table 5).
Discussion
Cognitive performance
We found that opioid-dependent patients on MMT were cognitively impaired compared with the HCs on tests of executive function and attention4,32 related to frontal networks3. However, methadone is also an active agonist drug that leads to opioid dependence and opioid abuse. The MMT may cause cognitive impairment, in which previous studies have reported that patients on MMT have more neuropsychological impairments than do currently abstinent former opioid abusers14,15.
We found a larger improvement of cognitive and executive function in the MMT+M group than in the MMT+P group. Moreover, on some of the measures the improvements in the MMT+M group have been taken to the levels of HCs, indicating the effect of memantine. This finding implied an association between memantine and cognitive improvement. For the attention performance tested using CPT, however, only the HRT by Block Change index improved in the MMT+M group. This finding may indicate that memantine protects opioid-dependent patients from slower psychomotor speed and increased impulsivity caused by MMT16.
Although Saab et al.33 reported that memantine affected the cognitive flexibility in mice memory. Wesierska et al.34, who compared the effects of different doses of memantine on working memory training in adult male rats, reported a dose-dependent and therefore suggested that a mild NMDAR blockade using low-dose memantine would improve spatial working memory in drug-naïve rats undergoing a highly challenging task. For these inconsistent results in animal models, the causality between the therapeutic effect of memantine and cognitive domains should be investigated. Moreover, in our study, adding a low dose of memantine (5 mg/day) to MMT improved cognitive performance; therefore, a large dose (60 mg/day by Bisaga et al. (1997) and 10–30 mg/day by Krupitsky et al., 2002) used in previous studies to investigate its effectiveness in improving cognitive performance or opioid tolerance/withdrawal symptoms might not be necessary. Bisaga et al. (1997) reports treating opioid-dependent patients undergoing opiate withdrawal with memantine (37 mg/day) but do not suggest that a dose of 60 mg/kg or less is effective for treating addictive behavior. Different doses of memantine might be another topic when investigating the therapeutic effect of MMT+M on cognitive functions.
MMT and the urinary drug test
About half of the MMT+P group (49.4%) and about one-fifth (ca. 26.3%) of the MMT+M group did not complete the tasks, which indicates a positive effect of MMT+M. A higher dropout rate in the MMT+P group than in the MMT+M group was consistent with a meta-analysis35 on patients with vascular dementia, which implied that memantine had a positive effect on remaining in the treatment. Because methadone is released slowly in unmetabolized metabolized form from liver and I N-demethylated in the chrome P450 enzyme, including CYP2D6 which has been reported tobe varied across different ethnics36,37,38. In addition, MMT program was launched by Taiwan Government in 2006 in response to the HIV/AIDS surge endemic in the Eastern Asia and made it country widely in 200739. Laio et al.27 conducted a study of from the Taiwan's national database of methadone service used from 2006–2008, containing 33, 549 subjects and reported that over half of the patients received methadone less than 45 mg/day and the mean dose was 46.5 ± 20.9 mg/day, which was similar to the average dose in the MMT+P group in our study. In Taiwan, the guideline suggests 5 mg increment of methadone a day for dose adjustment, MMT+M group patients had relatively lower dosage of methadone than did the MMT+P group patients after receiving 12-week MMT program further support the effect of add-on memanting in decreasing the methadone dosage as needed. At the 12-week of MMT treatment, an increase of methadone use was found in the MMT+P not in the MMT+M group, implying an effect of add-on memantine may decrease the dosage of methadone use.
The OTI data showed a decrease in criminality in the MMT+M group.
This study has some limitations. Although used to wean opioid-dependent patients from heroin and morphine, methadone itself is an addictive synthetic opioid. Whether methadone can be replaced by a non-addictive substance requires additional studies. Our total sample size (n = 81) had power> 0.8, which detected a medium effect (effect size = 0.5) for a repeated ANOVA. The dropout rate was higher in the MMT+P group than in the MMT+M group, longer follow-up duration might be needed to confirm the effect of add-on memantine in a longer-term treatment, e.g., 24 or 48 weeks, with a larger sample. The higher dropout rate was found in the MMT+ group which might influence the generalization of our results. Using per protocol analysis may bias the results, for example, participants who experienced sever adverse effect, poor financial support and family support were excluded might make the analysis reach significant level40. Moreover, lacking of craving data and prescription of benzodiazepines, the clinical relevance needs further study. Furthermore, because of relatively lower average methadone dose and shorter clinical experience of methadone use in Taiwan compared to other countries6,41, our finding might not be applicable to other ethnics.
Methods
Study design
This study, a double-blind, randomly clinical trial. The methods were carried out in "accordance" with the approved guidelines. The all experimental protocols were approved by the Institutional Review Board of National Cheng Kung University. The randomization strategy for treatment was simple randomization using excel's random number generator. Signed informed consent was obtained from all participants before they enrolled in this study. Participants who were opioid-dependent or opioid abusers were randomly assigned to one of two groups: methadone-maintenance therapy (MMT) plus add-on placebo (P) (MMT+P: MMT plus one daily placebo capsule) and methadone-maintenance therapy plus add-on memantine (M) (MMT+M: MMT plus one daily 5 mg M sustained-release capsule). Methadone dosage was increased or decreased by 5 mg when necessary in response to each participant's clinical situation. All participants were evaluated before and after the 12-week treatment.
Participants
Opioid-dependent participants who came to the Department of Psychiatry at National Cheng Kung University Hospital were recruited. Each participant, including the healthy controls (HCs), was asked to take the Chinese version of the Mini International Neuropsychiatric Interview (MINI) to screen their psychiatric conditions and confirm that all diagnoses of opioid dependence met the DSM-IV-TR (American Psychiatric Association 2000) diagnostic criteria. The Chinese version of the MINI has been reported as reliable and has been validated42. All potential participants with other major and minor mental illnesses, including alcohol abuse disorder, alcohol dependence disorder and illicit substance-use (other than heroin and morphine) disorders were excluded. All healthy controls were free of any major and minor mental illness.
The pre-MINI exclusion criteria were: being pregnant or nursing an infant; having taken any anti-inflammatory medications within 1 week before the study; having a major Axis-I DSM-IV diagnosis other than morphine dependence; and having a history of uncontrolled major physical increases in aspartate aminotransferase (AST), alanine aminotransferase (ALT), blood urea nitrogen (BUN) and creatinine levels.
Each opioid-dependent participant was given a urine drug test at each visit to determine whether they had used other substances, e.g., amphetamines or morphine and was asked to perform neuropsychological tasks and complete the Opiate Treatment Index (OTI) interview at baseline and at the end of the 12-week follow-up. In addition, each opioid-dependent participant was required to do cognitive tasks before and after the end of this study. The HCs were required to do cognitive tasks only once—at baseline—as a control comparison. All the HCs were interviewed using the Modified Chinese Version of the Modified Schedule of Affective Disorders and Schizophrenia-Lifetime (SADS-L)43 to confirm that they had no mental illness or history of substance dependence or substance abuse. We recruited 134 opioid-dependent Han Chinese outpatients from the methadone therapy clinic in the Department of Psychiatry at National Cheng Kung University Hospital and 37 age- and gender-matched HCs.
Wisconsin Card Sorting Test
The Wisconsin Card Sorting Test (WCST) measures the ability to perform certain types of executive functions: categorization, abstraction reasoning, maintaining sets, set switching, strategic planning and modulating impulsive responding44. The test requires that certain cognitive functions be intact, for example, attention, working memory and visual processing. Participants are required to try out different rules to find a correct method for sorting the cards. The original test used cards that had to be sorted into piles in front of four stimulus cards. The participants were instructed to infer the matching principle from the feedback provided: “correct” or “incorrect”, depending upon whether they correctly guessed the rule. The cards could be matched by number (1, 2, 3, or 4), color (yellow, green, blue, or red), or shape of the symbols (star, triangle, circle, or cross). The rule was applied for a run of trials and then changed without warning (Mei, 1998). The inter-rater liability is 0.88–0.93, within-rater reliability is 0.91–0.96 and test-retest reliability is 0.57. Performance on the WCST was scored in terms of the total number of errors (TNE), perseverative errors (PE), conceptual level responses (CLRs), number of categories completed (NCC) and trials to complete the first category (TCC).
Continuous Performance Test
The Conners' Continuous Performance Test (CPT)45 lasts for several minutes to assess the maintenance of focused attention. Optimal performance requires an adequate level of arousal, combined with an element of executive control to resist distraction and inhibit responses to stimuli resembling targets. Respondents are required to press the space bar on a computer keyboard when any letter other than “X” appears. The inter-stimulus intervals are 1, 2 and 4 seconds, with a display time of 250 ms.
The CPT produces a standard set of performance measures that include the number of errors of omission and errors of commission. (1) Errors of omission occur when the participant fails to respond to the target stimulus. (2) Errors of commission occur when the participant responds to a non-target (X) stimulus. (3) Hit reaction time (HRT) represents the Mean response time (milliseconds) for all target responses over the full six trial blocks. (4) HRT standard error (HRT SE) represents the consistency of response times and expresses the SE response to targets. (5) Detectability (d′) provides information on how well the examinee discriminates between targets and non-targets. (6) HRT by Block (HRT Block Change) measures changes in reaction time across the duration of the test. High scores indicate a substantial slowing in reaction times. (7) HRT Inter-Stimulus Interval (HRT ISI Change) examining changes in average reaction times across the different inter-stimulus intervals when the letters are presented at 1, 2, or 4 second intervals. According to the trade-off effect (Lachman et al., 1979), significant correlations between HRT, d′ and errors suggest the occurrence of a trade-off between speed and accuracy.
Opiate Treatment Index
The OTI is an evaluation tool for treating opiate users46. The original OTI has a multidimensional structure that measures six independent domains: drug use, HIV-risk-taking behavior, social functioning, criminality, health and psychological adjustment. It has good inter-rater reliability47. The Chinese version of OTI contains drug use, criminality and health domains modified by Zhao et al.48.
Statistical analyses
Data are means ± standard deviation. A repeated measurement with a mixed design, Group (MMT+P; MMT+M) × Time at two points during the study (pre-treatment = baseline; post-treatment = after 12 weeks of treatment) was done to determine whether there was an interaction between these sets of two factors. McNemar's test was conducted to explore changes in urine drug test values between baseline and the end of this study in each patient group. Significance was set at p <0.05.SPSS 18.0 was used for all statistical computations.
Additional information
Clinical Trial Registration Number: NCT01189214 (http://clinicaltrials.gov/ct2/show/NCT01189214?id=NCT01189214&rank=1)
How to cite this article: Chang, Y.-H. et al. Low-dose add-on memantine treatment may improve cognitive performance and self-reported health conditions in opioid-dependent patients undergoing methadone-maintenance-therapy. Sci. Rep. 5, 9708; DOI:10.1038/srep09708 (2015).
Change history
15 June 2017
A correction has been published and is appended to both the HTML and PDF versions of this paper. The error has not been fixed in the paper.
References
Davis, P. E., Liddiard, H. & McMillan, T. M. Neuropsychological deficits and opiate abuse. Drug Alcohol Depend 67, 105–108 (2002).
Grant, I., Adams, K. M., Carlin, A. S. & Rennick, P. M. Neuropsychological deficit in polydrug users. A preliminary report of the findings of the collaborative neuropsychological study of polydrug users. Drug Alcohol Depend 2, 91–108 (1977).
Goldstein, R. Z. & Volkow, N. D. Drug addiction and its underlying neurobiological basis: neuroimaging evidence for the involvement of the frontal cortex. Am J Psychiatry 159, 1642–1652 (2002).
Ersche, K. D. et al. Abnormal frontal activations related to decision-making in current and former amphetamine and opiate dependent individuals. Psychopharmacology (Berl) 180, 612–623, 10.1007/s00213-005-2205-7 (2005).
Baldacchino, A., Balfour, D. J., Passetti, F., Humphris, G. & Matthews, K. Neuropsychological consequences of chronic opioid use: a quantitative review and meta-analysis. Neurosci Biobehav Rev 36, 2056–2068, 10.1016/j.neubiorev.2012.06.006 (2012).
Webster, L. R., Reisfield, G. M. & Dasgupta, N. Eight principles for safer opioid prescribing and cautions with benzodiazepines. Postgrad Med 127, 1–6 (2014).
Mattick, R. P., Kimber, J., Breen, C. & Davoli, M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev, CD002207, 10.1002/14651858.CD002207.pub3 (2008).
Mattick, R. P., Breen, C., Kimber, J. & Davoli, M. Buprenorphine maintenance versus placebo or methadone maintenance for opioid dependence. Cochrane Database Syst Rev 2, CD002207, 10.1002/14651858.CD002207.pub4 (2014).
Gruber, S. A. et al. Methadone maintenance improves cognitive performance after two months of treatment. Exp Clin Psychopharmacol 14, 157–164, 10.1037/1064-1297.14.2.157 (2006).
Prosser, J. et al. Neuropsychological functioning in opiate-dependent subjects receiving and following methadone maintenance treatment. Drug Alcohol Depend 84, 240–247, 10.1016/j.drugalcdep.2006.02.006 (2006).
Soyka, M. et al. Cognitive functioning during methadone and buprenorphine treatment: results of a randomized clinical trial. J Clin Psychopharmacol 28, 699–703, 10.1097/JCP.0b013e31818a6d38 (2008).
Soyka, M. et al. A comparison of cognitive function in patients under maintenance treatment with heroin, methadone, or buprenorphine and healthy controls: an open pilot study. Am J Drug Alcohol Abuse 37, 497–508, 10.3109/00952990.2011.600381 (2011).
Soyka, M., Zingg, C., Koller, G. & Hennig-Fast, K. Cognitive function in short- and long-term substitution treatment: are there differences? World J Biol Psychiatry 11, 400–408, 10.1080/15622970902995604 (2010).
Mintzer, M. Z., Copersino, M. L. & Stitzer, M. L. Opioid abuse and cognitive performance. Drug Alcohol Depend 78, 225–230, 10.1016/j.drugalcdep.2004.10.008 (2005).
Verdejo, A., Toribio, I., Orozco, C., Puente, K. L. & Perez-Garcia, M. Neuropsychological functioning in methadone maintenance patients versus abstinent heroin abusers. Drug Alcohol Depend 78, 283–288, 10.1016/j.drugalcdep.2004.11.006 (2005).
Bracken, B. K. et al. Response inhibition and psychomotor speed during methadone maintenance: impact of treatment duration, dose and sleep deprivation. Drug Alcohol Depend 125, 132–139, 10.1016/j.drugalcdep.2012.04.004 (2012).
Joe, G. W., Simpson, D. D. & Sells, S. B. Treatment Process and Relapse to Opioid Use During Methadone Maintenance. The American Journal of Drug and Alcohol Abuse 20, 173–197, 10.3109/00952999409106781 (1994).
Howard, R. et al. Donepezil and Memantine for Moderate-to-Severe Alzheimer's Disease. New England Journal of Medicine 366, 893–903, 10.1056/NEJMoa1106668 (2012).
Morris, R. G., Anderson, E., Lynch, G. S. & Baudry, M. Selective impairment of learning and blockade of long-term potentiation by an N-methyl-D-aspartate receptor antagonist, AP5. Nature 319, 774–776 (1986).
Parsons, C. G., Stoffler, A. & Danysz, W. Memantine: a NMDA receptor antagonist that improves memory by restoration of homeostasis in the glutamatergic system--too little activation is bad, too much is even worse. Neuropharmacology 53, 699–723 (2007).
Popik, P. & Skolnick, P. The NMDA antagonist memantine blocks the expression and maintenance of morphine dependence. Pharmacol Biochem Behav 53, 791–797 (1996).
Ribeiro Do Couto, B., Aguilar, M. A., Manzanedo, C., Rodriguez-Arias, M. & Minarro, J. Effects of NMDA receptor antagonists (MK-801 and memantine) on the acquisition of morphine-induced conditioned place preference in mice. Prog Neuropsychopharmacol Biol Psychiatry 28, 1035–1043, 10.1016/j.pnpbp.2004.05.038 (2004).
Brown, P. D. et al. Memantine for the prevention of cognitive dysfunction in patients receiving whole-brain radiotherapy: a randomized, double-blind, placebo-controlled trial. Neuro Oncol 15, 1429–1437, 10.1093/neuonc/not114 (2013).
Wesnes, K. A., Aarsland, D., Ballard, C. & Londos, E. Memantine improves attention and episodic memory in Parkinson's disease dementia and dementia with Lewy bodies. Int J Geriatr Psychiatry, 10.1002/gps.4109 (2014).
Brown, S., Tapert, S., Granholm, E. & Delis, D. Neurocognitive functioning of adolescents: Effects of protracted alcohol use. Alcohol Clin Exp Res 24, 164–171, 10.1111/j.1530-0277.2000.tb04586.x (2000).
Goldberg, J. F. & Chengappa, K. N. Identifying and treating cognitive impairment in bipolar disorder. Bipolar Disord 11 Suppl 2, 123–137, 10.1111/j.1399-5618.2009.00716.x (2009).
Liao, D. L. et al. Higher methadone doses are associated with lower mortality in patients of opioid dependence in Taiwan. J Psychiatr Res 47, 1530–1534, 10.1016/j.jpsychires.2013.07.001 (2013).
Mattick, R. P., Breen, C., Kimber, J. & Davoli, M. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst Rev, CD002209, 10.1002/14651858.CD002209.pub2 (2009).
Krupitsky, E. M. et al. A Pilot Study of Memantine Effects on Protracted Withdrawal (Syndrome of Anhedonia) in Heroin Addicts. Addictive Disorders & Their Treatment 1, 143–146 (2002).
Jain, K. K. Evaluation of memantine for neuroprotection in dementia. Expert Opinion on Investigational Drugs 9, 1397–1406, 10.1517/13543784.9.6.1397 (2000).
Chen, S. L. et al. Low-dose memantine attenuated morphine addictive behavior through its anti-inflammation and neurotrophic effects in rats. J Neuroimmune Pharmacol 7, 444–453, 10.1007/s11481-011-9337-9 (2012).
Ersche, K. D., Clark, L., London, M., Robbins, T. W. & Sahakian, B. J. Profile of executive and memory function associated with amphetamine and opiate dependence. Neuropsychopharmacology 31, 1036–1047, 10.1038/sj.npp.1300889 (2006).
Saab, B. J., Luca, R. M., Yuen, W. B., Saab, A. M. & Roder, J. C. Memantine affects cognitive flexibility in the Morris water maze. J Alzheimers Dis 27, 477–482, 10.3233/jad-2011-110650 (2011).
Wesierska, M. J., Duda, W. & Dockery, C. A. Low-dose memantine-induced working memory improvement in the allothetic place avoidance alternation task (APAAT) in young adult male rats. Front Behav Neurosci 7, 203, 10.3389/fnbeh.2013.00203 (2013).
Kavirajan, H. & Schneider, L. S. Efficacy and adverse effects of cholinesterase inhibitors and memantine in vascular dementia: a meta-analysis of randomised controlled trials. Lancet Neurol 6, 782–792, 10.1016/S1474-4422(07)70195-3 (2007).
Bradford, L. D. CYP2D6 allele frequency in European Caucasians, Asians, Africans and their descendants. Pharmacogenomics 3, 229–243 (2002).
Kreek, M. J., Bart, G., Lilly, C., Laforge, K. S. & Nielsen, D. A. Pharmacogenetics and Human Molecular Genetics of Opiate and Cocaine Addictions and Their Treatments. Pharmacological Reviews 57, 1–26, 10.1124/pr.57.1.1 (2005).
Smith, H. S. Opioid Metabolism. Mayo Clinic Proceedings 84, 613–624 (2009).
Chen, Y. M. & Kuo, S. H. HIV-1 in Taiwan. Lancet 369, 623–625, 10.1016/S0140-6736(07)60291-8 (2007).
Brody, B. A. et al. Is the use of placebo controls ethically permissible in clinical trials of agents intended to reduce fractures in osteoporosis? J Bone Miner Res 18, 1105–1109, 10.1359/jbmr.2003.18.6.1105 (2003).
D'Aunno, T., Pollack, H. A., Frimpong, J. A. & Wuchiett, D. Evidence-based treatment for opioid disorders: a 23-year national study of methadone dose levels. J Subst Abuse Treat 47, 245–250, 10.1016/j.jsat.2014.06.001 (2014).
Huang, S. Y. et al. Possible interaction of alcohol dehydrogenase and aldehyde dehydrogenase genes with the dopamine D2 receptor gene in anxiety-depressive alcohol dependence. Alcohol Clin Exp Res 28, 374–384, 10.1097/01.ALC.0000117832.62901.61 (2004).
Endicott, J. & Spitzer, R. L. A diagnostic interview: the schedule for affective disorders and schizophrenia. Arch Gen Psychiatry 35, 837–844 (1978).
Mohlman, J. Does executive dysfunction affect treatment outcome in late-life mood and anxiety disorders? J Geriatr Psychiatry Neurol 18, 97–108, 10.1177/0891988705276061 (2005).
Conners, C. & Staff, M. Conners' Continuous Performance Test (CPT-II.). (2000).
Darke, S., Jeff, W., Nick, H. & Alex, W. The Opiate Treatment Index (OTI) Manual. (1991).
Deering, D. E. & Sellman, J. D. An inter-rater reliability study of the Opiate Treatment Index. Drug Alcohol Rev 15, 57–63, 10.1080/09595239600185671 (1996).
Adelekan, M. et al. Reliability and validity of the Opiate Treatment Index among a sample of opioid users in the United Kingdom. Drug Alcohol Rev 15, 261–270, 10.1080/09595239600186001 (1996).
Acknowledgements
This study was supported in part by grant NSC 98-2627-B-006-017 from the Taiwan National Science Council (to RBL) and by a grant from the National Cheng Kung University Project to Promote Academic Excellence and Develop a World Class Research Center.
Author information
Authors and Affiliations
Contributions
Y.C. wrote the draft of this manuscript and designed this study with S.C. and R.L., S.L., P.C., T.W., I.L., K.C. and Y.Y. and managed the patient recruitment and statistical analyses. This study was supervised under R.L. and J.H.
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article's Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder in order to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Chang, YH., Chen, SL., Lee, SY. et al. Low-dose add-on memantine treatment may improve cognitive performance and self-reported health conditions in opioid-dependent patients undergoing methadone-maintenance-therapy. Sci Rep 5, 9708 (2015). https://doi.org/10.1038/srep09708
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep09708
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.