If Michelle Boyer had received her diagnosis of advanced and aggressive skin cancer in 2010 instead of 2013, she would almost certainly be dead by now. Melanoma, the most lethal form of skin malignancy, had spread from a mole on her back to her lungs, and she knew her prognosis was grim. But beginning in May 2013, the 29-year-old Seattle resident started a series of revolutionary treatments—some of which first became available in 2011—that prompted her immune system to identify, attack and shrink the tumors. Although Boyer still has cancer and the immune-boosting drugs have taken a toll on her body, she is grateful to be alive and hopes that either her current course of therapy or the next one will eventually give her the kind of miraculous results that other patients have talked about on the Internet. “At this point, this is my life,” she says. “People think it would be really hard to stay positive, but because to me it seems normal, it's not as much effort as you would think.”
Karen Koehler, 59, a retired special education teacher from Park Ridge, N.J., may have won the immunotherapy jackpot on her first try. She has apparently been cured of a different kind of cancer—in her case leukemia—after a single infusion, in early 2015, with some of her own immune cells that had been genetically altered to fight her malignancy more aggressively. The treatment, which lasted a couple of hours, landed her in intensive care for several days because her revved-up immune system shifted so far into overdrive. This setback was followed by weeks in a regular hospital bed. But within a month after her treatment, scans showed no signs of cancer anywhere in her body.
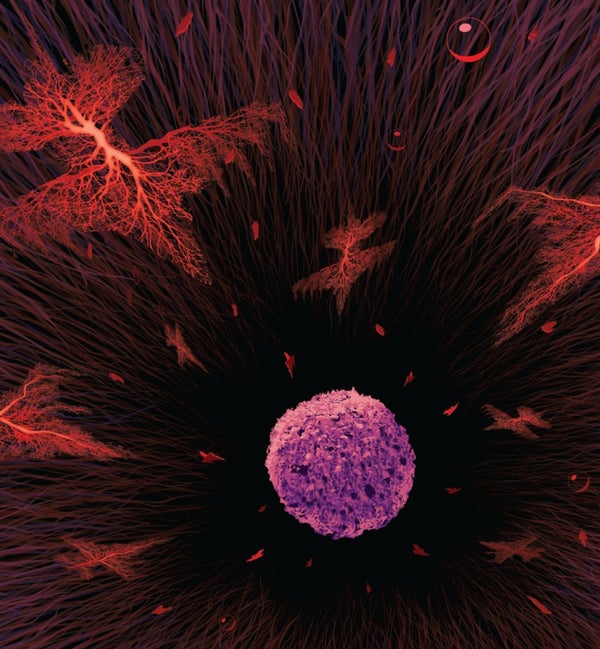
Boyer and Koehler are two of the thousands of cancer patients who have undergone various kinds of immunotherapy over the past five years. Their experiences illustrate both the promise and the challenges of this fundamentally new approach to treating cancer—one that, instead of dousing the body with toxic chemicals or radiation from the outside to kill cancer cells, energizes the complex and highly interactive cells and molecular signals of its defense networks to do the job from the inside. The results so far have been encouraging; immunotherapy is quickly becoming a pillar—along with surgery, radiation and chemotherapy—of treatment for some cancers.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
In clinical trials of a new immunotherapy for a highly aggressive form of leukemia, 90 percent of patients underwent a complete remission: doctors could find no evidence of their disease anywhere in their bodies. Although some may eventually suffer a return of their cancer, for many others the response appears to be a permanent cure. In other trials, more than half of patients with advanced melanoma who received immunotherapy can now count their life expectancy in years instead of months. Immunotherapy, says Gary Gilliland, president and director of the Fred Hutchinson Cancer Research Center in Seattle, “is truly paradigm shifting in our approach to treating cancer.”
These are, admittedly, still early days. Increasing life expectancy to a few years for some cancers still means that patients die of the disease. So scientists continue to experiment with different ways to unleash and boost the immune response, including vaccines, viruses, genetically engineered cells and pills. They are also beginning to combine these approaches to see if they can help more patients, perhaps with fewer side effects. But there is no longer any doubt that physicians can tap the immune system to beat cancer at least some of the time. “[We are at] the end of the beginning” of the immunotherapy story, says Eric Rubin, vice president of global clinical oncology for Merck Research Laboratories.
Liquid Success
The dream of fighting cancer with the immune system dates back at least 125 years to William Coley of New York City, a physician who injected some of his cancer patients with bacteria in an effort to jump-start their body's natural healing powers. Coley's approach was taken up by a few other doctors initially. But it gradually fell out of favor after his death in 1936, to be replaced by advances in chemotherapy and later hormone and antibody treatments, which showed more consistent results on a larger number of patients.
The idea of boosting the immune system, however, has never entirely lost its appeal, promoted in part by the Cancer Research Institute, a New York City–based philanthropy started in 1953 by Coley's daughter. In recent decades, as molecular biology has enhanced researchers' understanding of the immune system, how it works and when it fails, cancer investigators have restocked their arsenal with more potent immunological weapons.
Among the most attractive targets for those weapons have been cancers of the circulatory and lymphatic systems, such as leukemia and lymphoma. These diseases occur when various kinds of progenitor cells called stem cells, which normally give rise to red and white blood cells (among other tissues), instead mutate and grow uncontrollably, crowding out healthy cells and robbing the body of their vital functions. Many of these so-called liquid tumors form when something goes wrong with a part of the immune system called B cells. Normally B cells generate antibodies against bacteria and viruses. (B cells also help to coordinate various other immune responses, along with another group of cells called T cells.) But when B cells become cancerous, they destroy the body from the inside out.
In the late 20th century investigators developed the biological equivalent of a guided missile that attached itself to a B cell protein (CD20) found on the surface of these cells at a specific, late stage of their existence. Dubbed rituximab, this so-called monoclonal antibody signaled the T cells to do something they do not usually do: attack and destroy these older, CD20-bearing B cells.
The problem was that CD20 is not a cancer-specific marker. It appears on normal B cells as well as dangerous ones. So the drug killed both healthy and cancerous B cells. It turns out, however, that most people can live without B cells. (The same is not true of T cells, as the death of millions of people infected with the T cell–targeting AIDS virus tragically demonstrates.) And after the drug wore off, most patients eventually started making B cells on their own again from the stockpile of stem cells in their bone marrow. Clinical trials in the 1990s demonstrated that the combination of chemotherapy and rituximab was particularly effective against B cell–based cancers.
Koehler's leukemia originated with mutated B cells, but rituximab made her very sick and seemed only partially effective, so she stopped taking it. In addition, tests indicated her cancer would resist standard chemotherapy. Because her malignancy was rapidly getting worse, her doctors suggested an experimental immune treatment custom-designed to fight her form of leukemia. She agreed.
The goal of the new treatment was to destroy all of Koehler's B cells, as rituximab would, but with two key differences. A different protein (CD19) on the B cells was the objective. And rather than using an added drug to paint a target on that protein for T cells that were already in Koehler's body, doctors took a more direct approach. They removed some of her T cells and genetically engineered them to attack CD19 automatically, without any prompting.
Investigators call these turbocharged cells chimeric antigen receptor T cells, or CAR-T. They display some of the characteristics of both T cells and B cells in much the same way that ancient mythological creatures called chimeras were supposed to be made up of different animals. CAR-T therapy is still experimental, but the Food and Drug Administration is expected to consider approving the treatment for general use sometime next year.
The CD19-targeting CAR-T cells multiplied so quickly inside Koehler's body that the single bag of modified cells that she received on February 10, 2015, knocked out all her B cells. Unlike other patients, however, her body seems to have forgotten how to make healthy B cells. Fortunately, there is a work-around: every month she gets an hours-long infusion of artificial antibodies, called gamma globulin, to help protect her against infection. The infusions are a time-consuming hassle, she says, but “it's not chemo, so I'll take it.”
CAR-T therapy did hit Koehler with something that can be worse than chemo's nausea—a storm called cytokine release syndrome. This reaction occurs when many more T cells than usual are activated at once—triggering a flood of chemical signals, called cytokines, that the immune system uses to communicate. The result can be a life-threatening frenzy of activity, in which immune cells destroy healthy tissues, causing multiorgan failure.
For Koehler, the storm came on hard and fast. She felt terrible within an hour of receiving her own altered T cells. By that night she was in intensive care where she remained for eight days—half of that time she was in a coma and totally unresponsive. She has no memory of what transpired then but can recall the hallucinations of a few days later, when she asked nurses for help packing lunch for a pair of famous golfers. Koehler has been addicted to golf since 1999, when she took it up as a way to meet men, including the man who later became her husband.
By the time Koehler got out of the hospital in early March 2015, she was incredibly weak but rebounding fast. A bone marrow test showed no evidence of cancer, and three weeks after that she was back on the golf course with her husband. The cytokine storm was terrible, but unlike chemo, the effects subsided within a few weeks and did not cause her to lose her hair. Fortunately, given that cytokine storms are fairly common with CAR-T cell treatments, physicians have begun to learn just how far to push patients like Koehler to get the greatest benefit without risking their lives.
CAR-T cell therapy must be custom-designed and produced for each patient. Manufacturing them for all the leukemia and lymphoma patients who might want them will be a challenge, as well as extraordinarily expensive—although it is too soon to know exactly how much CAR-Ts will cost because they have been used only in academic research so far. Robert Preti, founder of PCT, a CAR-T manufacturer, is working to improve the production process; he believes these are mainly engineering issues that will be solved with a few more years of hard work.
The other major challenge facing CAR-T treatment is translating its success from liquid cancers to solid tumors—the kind that forms lumps in the breast, prostate, lung, skin and other tissues. One stumbling block is that CAR-T cells have a hard time leaving the bloodstream to find a solid tumor, explains Ira Mellman, who is vice president of cancer immunology at Genentech. In the blood, the liquid tumor cells are relatively easy to locate. Even more crucial, whereas CAR-Ts can eliminate B cells in blood and lymph cancers, there is no comparable cell in solid tumors that patients can live without.
Solid State
Solid tumors pose other difficulties for immune treatments. They are often surrounded by a matrix of connective and other tissues, which blocks cells from entering the malignant mass. In addition, the internal pressure of a solid tumor is typically higher than its surroundings, which tends to flush out the chemical signals that the immune system uses to flag aberrant cells—not to mention many drugs.
Yet these tumors have shown some vulnerability. In 2011 the FDA approved a monoclonal antibody called ipilimumab to treat advanced cases of melanoma. Unlike traditional therapy, ipilimumab is not designed to kill tumors directly; rather it releases the biological brakes that some cancers are able to clamp on the immune system, freeing the body's defenses to do a better job.
Melanoma has a nasty habit of defrauding immune system cells. The clumps of cancer cells have an assortment of malformed proteins on the surface, which T cells are supposed to spot, swarm around and destroy before the aberrant growth has a chance to get any bigger. But every now and then a nascent tumor develops a way to send out chemical signals that tell the T cells that all is well and to stand down their attack.
In effect, the cancer cells have hijacked a normal feature of the immune system: a safety mechanism that tamps down the body's rampaging defense cells before they start damaging healthy tissue. More specifically, this safety mechanism consists of a series of checkpoints, or gateways, that either rally defense cells to attack or turn them off, depending on which chemical signals are present. (If the checkpoints ever got stuck in the “open” position, the ensuing immune reaction would likely kill a person faster than any malignant growth could.) By producing proteins that block the checkpoint system, cancer cells prevent the immune system from ever ramping up to fight off cancer. Blocking that false signal with ipilimumab or other so-called checkpoint inhibitors reawakens the immune cells, allowing them once again to zero in on their targets.
Ipilimumab soon proved effective in lung cancer as well as melanoma, and pharmaceutical companies began developing other drugs that used the same strategy. Former U.S. president Jimmy Carter, 91, whose melanoma had spread to his brain, took one such drug, pembrolizumab, and he announced late in 2015 that the drug had cleared all his tumors.
Boyer, on a similar regimen with a similar disease, has not fared as well. And that is a puzzle. Some researchers speculate that Carter's advanced age may have helped him. Older cancer cells have more mutations, so his immune system may have needed just a single nudge to release the T cells that were already there. In some patients, in contrast, the T cells may never have made it into the tumor, and so there was nothing there to unblock. In other patients, the T cells seem to be in the right place, but the drug still does not work—perhaps because multiple steps need to be unjammed. A 2015 study in the New England Journal of Medicine showed that more melanoma patients did better when given two checkpoint inhibitors instead of one.
Still, doctors are not good at predicting who will respond to which checkpoint inhibitor or combination of treatments, and so Boyer and patients like her have to keep experimenting with different therapies. Today just more than 20 percent of advanced melanoma patients in clinical trials get a complete response from checkpoint inhibitors, with slightly more than half having some response. To confuse matters even more, some tumors that appear to attract few T cells still respond to checkpoint inhibitors, whereas the drugs sometimes have no effect on other tumors that contain lots of T cells—suggesting the cancer is playing other tricks.
That has made picking an effective solid tumor treatment for a particular individual a matter of trial and error, as Boyer's experience illustrates. Two years after surgery to remove the cancerous mole from her back, she learned that the melanoma had returned and was spreading throughout her lungs and chest. Because the growths were now too large to be cut out, Boyer agreed with her physicians to take part in a clinical trial at the beginning of 2013 that would inject her with high doses of interleukin-2 (IL-2), one of dozens of different chemical signals that help to boost the immune system's ability to fight cancer. At first the drug seemed to stop the growth of Boyer's tumors, but after three months, scans showed that the cancer was on the move again.
Boyer opted for a second clinical trial, this time pairing the recently approved checkpoint inhibitor ipilimumab with still another immune-signaling molecule known as IL-21. Within a few weeks, however, the side effects of the IL-21 treatment (nausea, diarrhea and unbearable pain) had become so disabling that Boyer had to stop getting the injections, although she continued receiving the ipilimumab. By the end of 2013 some of the cancerous spots had started to expand, and so her medical team opted for radiation to try to limit the growth. By spring of the following year a few of these tumors were smaller, but new ones had appeared on her head and in her breast.
Surgery dispatched the lump in her breast, and two other immune-boosting therapies seemed to hold the rest of her tumors in check for a while. By January 2015, however, it became clear that she needed another plan of action—new spots had begun to grow in her brain, breast and abdomen. A month later she entered a clinical trial, which combined yet another checkpoint inhibitor with a drug that is supposed to slow tumor growth. As this article went to press, Boyer's cancerous spots remain stable, and some of them have even shrunk a little.
There is no denying that so many treatments have battered Boyer's body. She spends her nights and many of her days in a plush loveseat to rest her back. She goes to work as a structural engineer most mornings on the weeks she has off from her sixth and current round of treatment. Otherwise she entertains herself by playing video games—Call of Duty is her favorite. All told, however, she does not regret trying six different immunotherapy regimens so far. “It seems to me that some of these treatments maybe slowed down the growth a little bit,” she says. One of her doctors, Boyer remembers, “said part of the game for melanoma was not necessarily finding the right treatment now, but keeping yourself alive long enough until they find the right treatment.” And so she is and so far accepts her current quality of life.
Looking Ahead
Because Boyer and other patients are living long enough to feel some contentment, Genentech's Mellman is excited. For immunotherapy, possibilities have begun to turn into actual results in patients, he says. Investigators no longer worry about whether their research will eventually help someone; now they can spend their time making effective treatments better. “We need to find the boundaries and limitations and figure out how to get around them,” Mellman says, but “this is an incredibly inspiring and thrilling way to do science.”
Eventually the process of selecting an immune treatment will become more logical, he believes. A patient with a solid tumor might first have the tumor biopsied to look for the presence of T cells. If enough T cells were in the tumor, the person would likely be given a single checkpoint inhibitor or maybe several inhibitors. (At present, the FDA has approved three checkpoint inhibitors, but more than a dozen others are under development.) If the tumor has not already attracted many T cells, doctors may try various other techniques to both drive the immune cells in and call the immune system's attention to the abnormal growth before opening the checkpoints.
Researchers are also considering how to use standard cancer care, including radiation and chemotherapy, to boost the immune response. Killing a number of tumor cells with lower doses of chemotherapy or radiation should release lots of cellular debris from the tumor, thereby alerting the immune system to send T cells to whatever abnormal growth remains. (Getting the balance right may be tricky because too much chemotherapy and radiation have also been shown to suppress parts of the immune system.) Then, the addition of a checkpoint inhibitor might be able to effectively fight the weakened cancer before it has a chance to recover. But scientists have only just begun to test such hypotheses.
Finally, as more and more immunotherapies are approved by the FDA, they present an entirely different, nonmedical challenge: price. Combining therapies raises the cost of what are already quite expensive treatments. The global market for oncology drugs is now approaching $100 billion a year, according to IMS Health, a medical data company, but drug firm executives acknowledge that insurers and the public will not be willing or able to indefinitely combine drugs that can run $150,000 or more per patient. They are looking at manufacturing improvements, lower doses and shorter treatment times, among other approaches, to lower the eventual cost of treatment.
Even today's curative therapies are far from perfect. Koehler still has some lingering effects from her treatment. She tires more easily than she used to. If she goes to lunch with friends, she might not have the energy to take a hike later with her husband. “The toughest part now is how far do I push myself,” she says. But Koehler is able to enjoy the retirement she took when her first therapy did not work. She golfs, hikes or snowshoes when the weather permits. Inspired by the therapy dogs that visited her during her hospital stay, she brings her own golden retriever, CJ, to the local high school to help relieve exam stress among students there. Cancer doctors believe immunotherapy will soon allow them to give many more patients similar opportunities to enjoy a new lease on life.