In 1996, Charles Sawyers designed early clinical trials for one of the first drugs aimed at a cancer-specific genetic mutation. The drug was imatinib, the cancer was chronic myeloid leukaemia and Sawyers — a clinical oncologist at the Memorial Sloan Kettering Cancer Center in New York — saw patients who had been debilitated by the disease rapidly improve when given the medicine. “It was unbelievably satisfying,” he says.
Unfortunately, he then saw many of those cancers come roaring back as they became resistant to the drug.
The experience with imatinib has given cancer biologists mixed messages. The medicine, now marketed by Novartis in Basel, Switzerland, as Gleevec or Glivec, highlights the potential of personalized medicine. Figuring out what mutation caused the disease and designing a drug to target it was a technological triumph, and it was followed by two further drugs to combat the emerging drug resistance.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
But treating cancer by chasing mutation after mutation with drug after expensive drug is not a sustainable model — not least because few cancers other than leukaemia have simple, known genetic causes. “When we know the mutations and can get to a treatment strategy it's exciting,” says Sawyers. But so far in the age of gene sequencing, he adds, “we've grabbed the low-hanging fruit”.
Biologists now know a huge amount about cancer — much more than they did even ten years ago. About 500 genes have been implicated in the disease, and the list is growing. There are also about 100 approved cancer drugs, some of which, like imatinib, specifically target mutations in those genes, on top of older therapies such as surgery and radiation.
But all this knowledge is not enough: even in countries where people have access to the newest therapies, improvements in death rates have slowed. Up to half of cancers could be prevented by changes in diet and exercise, encouraging people to stop smoking and eliminating environmental risks such as pollution, but other gains will be harder. To conquer cancer, researchers will need to answer some basic scientific questions. Here, Nature looks at three of the most pressing.
How Can Drug Resistance be Overcome?
To combat resistance, researchers are studying the cancer genome, coming up with new ways to design drugs, concocting combination therapies — and even looking back to Darwin's theory of evolution.
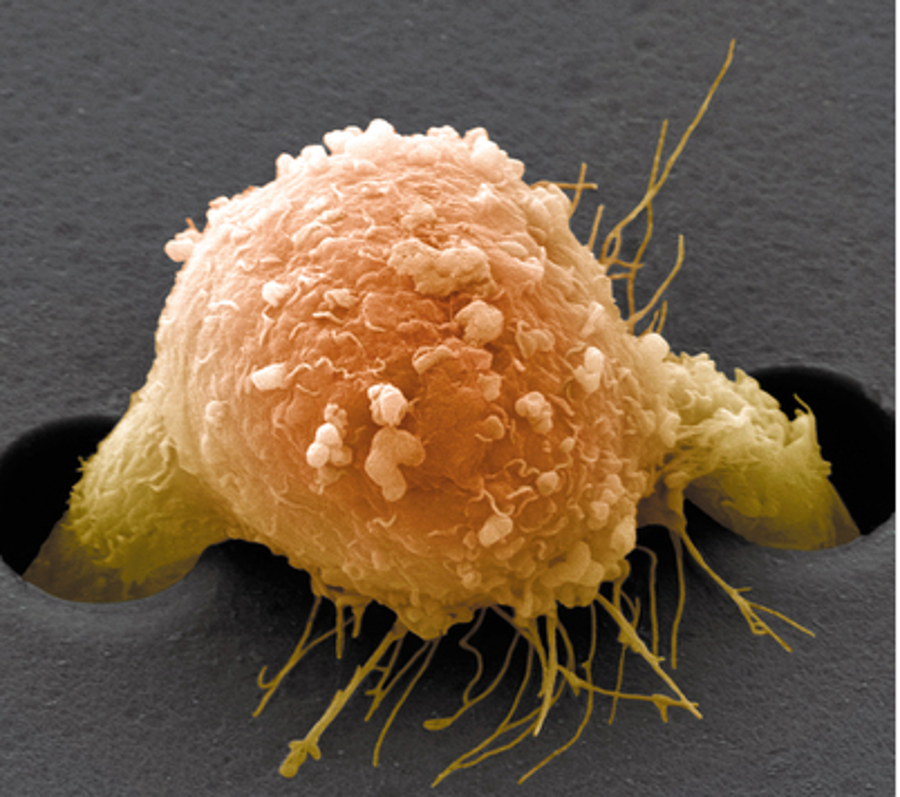
“Seen through a Darwinian lens, the tumour is an ecosystem, a mixture of cells that are continuously mutating,” says Paul Workman, head of cancer therapeutics at the Institute of Cancer Research in London. “You put into that mix a very strong selective pressure, which is the drug.” At that point it becomes survival of the fittest. Many cells die; others use a combination of strategies to survive and thrive. These may include producing protein pumps that flush the drug out, increasing the rate of DNA repair or using an alternative molecular pathway to restore whatever function the drug blocks. Targeted drugs contribute to the genetic complexity: “These therapies themselves may be driving tumours to become more heterogeneous,” says Charles Swanton, a medical oncologist at Cancer Research UK's London Research Institute.
A better understanding of the underlying genetic diversity of tumour cells may help researchers to work out how to tackle drug resistance. Swanton and others are therefore exploiting ever-faster and cheaper DNA-sequencing technologies. So far, Swanton says, it looks as though every tumour has a set of core mutations that are shared by all its cells. He calls these the tumour's ‘trunk’. Subpopulations of cells within the tumour have their own unique sets of shared mutations; he calls these subpopulations ‘branches’. Therapy prunes some branches while sparing others, which then repopulate the tumour.
Researchers are now trying to look at tumour evolution in patients. One study, called TRACERx (Tracking Cancer Evolution through Therapy), will allow Swanton and a large group of collaborators to observe 850 people with lung cancer from diagnosis through therapy. Biopsies are taken from multiple spots within tumours both before and after treatment, then analysed by sequencing the parts of the tumour genomes that code for proteins. Comparing these biopsies should identify which mutations are associated with drug resistance. These kinds of studies may help geneticists to write what Swanton calls “an evolutionary rulebook of cancer” that can be used to predict tumour evolution without having to do repeated sequencing studies to get future patients on the right therapies.
Other researchers caution that genetics will provide only part of the picture of tumour heterogeneity and drug resistance. Variations in how tumours use these genes — the way they are regulated and expressed — also enable tumours to develop drug resistance. “Cells that are not intrinsically resistant to a drug will rewire their circuitry during treatment to become resistant” without any genetic changes at all, says cell biologist Joan Brugge at Harvard Medical School in Boston, Massachusetts.
Even without a full understanding of the way that tumours evolve in the face of chemotherapy, researchers are coming up with ways to overcome resistance. Using a combination of drugs can reduce a tumour's options. Here, scientists take inspiration from the success of the antiretroviral cocktails that keep HIV in check. Like cancer, HIV has tremendous genetic diversity and evolves rapidly, but the right cocktail of drugs has transformed HIV infection from a death sentence for many into a manageable, long-term condition. Cancer presents a tougher challenge. HIV has just nine genes, compared with our approximately 20,000, making human cancer cells much more complex. Researchers are still trying to figure out how to make smart combination therapies that really work.
James Doroshow, head of cancer treatment and diagnosis at the US National Cancer Institute (NCI) in Bethesda, Maryland, believes that the best way to figure out combination therapies is to test the possibilities through brute force. The NCI has been testing 5,000 drug combinations against 60 cancer cell lines in vitro; promising candidates are then screened for toxicity in mice. The results have not yet been published, but Doroshow says that new and unexpected combinations are showing up.
Workman's group is using computer models of gene networks to sort through thousands of possible drug combinations and genes to find likely synergies. He agrees that combination therapy is the only way to overcome resistance, but thinks that new drugs are also needed. He estimates that just 5% of known cancer genes are targeted by drugs. “If we can't make drugs against the other 95%,” he asks, “how on Earth are we going to build the combination therapies that will lead to a cure?”
To make matters more difficult, some cancer-causing mutations work by silencing the tumour-suppressor genes that normally help to stop tumours from forming. Developing a drug to block the absence of something is a major challenge, says Workman. And some of the genes associated with cancer make proteins whose structures are unknown; without the structure, chemists have nothing to go on. Many cancer genes therefore remain, for the time being at least, untargetable.
How are Healthy Tissue and Genes Involved?
Cancer is caused not just by bad cells or bad genes, but also by good ones not doing the right thing — an aspect of cancer that is highly complicated to study and to combat.
Mina Bissell, a bioengineer at the Lawrence Berkeley National Laboratory in California, sees potential in an area that has been largely ignored by the pharmaceutical industry: the supportive structures and non-cancer cells in and around tumours, called the tumour microenvironment. Signals from this microenvironment can stop a cell that has cancer-causing mutations from becoming cancerous, and putting a tumour cell in a different environment can render it benign. “We need to therapeutically fix the microenvironment,” she says.
Jacqueline Lees, associate director of the Koch Institute for Integrative Cancer Research at the Massachusetts Institute of Technology in Cambridge, agrees. It is important, she says, to think not just about killing cancer cells but also about targeting the processes that support them, the interactions between tumour and non-tumour cells and the immune system. Tumours cannot thrive without certain kinds of signalling patterns from their neighbouring cells. “Traditional drug screening has missed that,” Lees says.
Lees is studying a process called cancer dormancy. Some cancer cells are quiescent during the tumour's boom times but can become reactivated if left behind after surgery. Lees is trying to determine how this works, and what role normal cells have in the dormancy and activation process.
Quiescent tumour cells are less vulnerable to chemotherapy because the treatments are aimed at dividing cells, and quiescent ones are not taking part in the normal cell cycle of growth and division.
What signals from the microenvironment are needed to wake these cells? Lees says that inflammation — a sign of activation of the immune system — after surgery and treatment may jump-start quiescent cells. Then, a tumour cell has to warm up its engines. “It has to switch back on a whole protein program that takes 48 hours, and during that time it's taking advantage of interactions with normal surrounding cells,” she says. The right drugs in the right order could help to control this process. Chemotherapy could be preceded by drugs that wake up the quiescent cells. Then drugs that suppress crosstalk could prevent them from restarting a tumour after therapy.
If it can be revved up, the immune system might be able to do this itself. Cancer cells put up many defences against attack from the immune system, including expressing receptors that deactivate an important class of immune cell. In the past few years, drugs that block these receptors have generated much excitement in clinical trials. These drugs, called immune checkpoint inhibitors, seem to let loose the immune system's natural cancer-fighting activity. But they do not work in all patients, and researchers have yet to figure out why, says Sawyers. For these patients, a combination of drugs that target the tumour, the support cells and the immune system “could save the day”, he says.
Lees agrees. Successfully treating cancer may require attacking tumours on multiple fronts, she says, with conventional therapies bolstered by new ones that activate the immune system and silence certain interactions between tumours and their environment.
How Does Cancer Spread?
The cause of most cancer deaths — about 90% — is not the primary tumour, but secondary tumours called metastases that have developed elsewhere in the body. Sometimes these metastatic tumours become apparent decades after a patient was thought to be cured. So a better understanding of metastasis would help to prevent a great deal of cancer deaths. “We need to focus more on secondary tumours,” says Ann Chambers, director of translational breast-cancer research at the London Health Sciences Centre in Canada.
The beginning of the metastatic process is by now pretty well understood, says Robert Weinberg, a cancer biologist at Whitehead Institute for Biomedical Research in Cambridge, Massachusetts. Some cancer cells become motile and aggressive, and enter the bloodstream. Some exit the circulation at distant sites, and a fraction of these can start new tumours there (C. L. Chaffer and R. A. Weinberg Science331, 1559–1564; 2011). What is incredible, says Weinberg, is that any of these cells live, let alone seed new tumours. “The big remaining mystery is how cancer cells are able to adapt and make a living in a distant tissue,” he says. The environment in the brain or bone marrow, say, is very different from that in the prostate or breast, where the tumour may have started its journey. There may be different levels of glucose and oxygen, or the foreign tissue might be more or less acidic. Tumour cells are thought to be dependent on growth factors, protein signals and other encouraging messages in their native tissue. Still, some cells form new tumours at other sites. Weinberg speculates that this involves not mutations, but extensive changes in gene expression.
Perhaps even more puzzling than how cells can thrive in a new place is what they do in the time between their arrival and the growth spurt that initiates secondary disease. “Cancer cells make it to a distant organ, escape the bloodstream — and then they sit there for ten years while nothing happens,” says tumour biologist Klaus Pantel of the University Medical Center Hamburg-Eppendorf in Germany. “Something keeps them from proliferating, and then something activates these cells.”
What those signals are is unknown. And not enough people are studying the problem, says Chambers. “Tumour dormancy is frustrating — like watching paint dry,” she says. “People don't want to watch tumours not grow.”
There are other barriers to studying metastasis. Secondary tumours that have grown large enough to cause health problems and be detected are often not biopsied because patients are in fragile health. And it is difficult to get a picture of the early stages of growth of metastases: they are too small to show up in imaging scans. Furthermore, Chambers notes, even when people have ideas for drugs to prevent or slow tumour spread, today's clinical trials are not designed to show this effect. Trials tend to enrol patients with advanced disease and established metastatic tumours. The potential of a drug to prevent the spread of cancer cannot be seen in this group because it is too late, she says.
To treat cancers that have already spread will require knowing more about the mechanics of metastasis. First, researchers must figure out which of the heterogeneous mix of cells in a tumour are capable of spreading, and how they differ from the other cells.
Brugge has developed a way to find these tumour-initiating cells. Researchers in her lab take about 100 cells from a primary tumour biopsy, separate them, clone them and give each its own genetic bar code. They then maintain one set in vitro and inject another into mice, says Brugge. Cells with metastatic tendencies will grow into tumours, and once they do, the researchers remove them and note, using the bar codes, which cells started the new tumours. Brugge can then go back to the cells in culture to study what differentiates them from cells that did not metastasize.
Another approach involves looking for tumour cells in patients' blood, cancer's metastatic thoroughfare. These circulating tumour cells may hold some answers to the mystery of metastasis — their ranks must include some that will form secondary tumours. Once isolated, they can be sequenced and imaged, and the expression of their genes can be compared with that of the primary tumour's.
Many key details of cancer biology remain elusive, but new technologies are helping researchers to gain access to them. Quickly advancing genomic and bioinformatics techniques are helping to overcome drug resistance by predicting which drugs to use and in what combinations; new models are providing insight into the interactions between normal and cancerous tissues; and metastatic cells can now be found before they make tumours.
Given this progress, veteran researchers find reason for optimism. “Twenty years ago, I would have thought some of these problems were intractable,” says Doroshow. “But now, I don't.”
This article is reproduced with permission and was first published on May 28, 2014.