Abstract
Background:
This was a retrospective audit, with the aims being to (1) record the use of antibiotics; (2) establish the prevalence of antibiotic-associated diarrhoea (AAD) and Clostridium difficile-associated diarrhoea (CDAD); and (3) assess if there was any seasonal variation in antibiotic use and incidence of AAD.
Methods:
The study was performed at a single spinal cord injury (SCI) centre in the UK. Data were collected using a standardised questionnaire during October 2014 to June 2015. We define AAD as two or more watery stools of type 5, 6 or 7 (Bristol stool scale) over 24 h.
Results:
Three-hundred-and-nineteen adults (mean age: 55.9 years, 29.2% female) with SCI (58.2% tetraplegia; 43.7% complete SCI) were included. Of 70 (21.9%) patients on antibiotics, the top three indications for antibiotics were urinary-tract infections, infected pressure ulcers and other skin infections. Seventeen of 78 (21.8%) developed AAD and three of 319 (0.94%) developed CDAD. AAD was more common in the summer season than in spring, autumn and winter (47.1%, 10.0%, 10.0%, 23.8%, P=0.025). AAD was associated with older adults greater than 65 years (70.6% vs 23.8%, P=0.007). Polypharmacy and the summer season were identified as independent predictors for AAD.
Conclusion:
This survey found that AAD is common in SCI patients and may be a risk factor for a poorer outcome and increased hospital costs. A multicentre study is underway to establish the incidence and risk factors for AAD.
Similar content being viewed by others
Introduction
Antibiotic-associated diarrhoea (AAD) is a common complication of antibiotic treatment. The disturbance of normal gut microbiota, especially after antibiotic use, is thought to predispose patients to pathogenic bacterial colonisation1, 2 It is reported that three predominantly opportunistic pathogens including Clostridium difficile (C. diff), Staphylococcus aureus and Clostridium perfringens were associated with AAD.3 AAD is described as unexplained diarrhoea that occurs in association with antibiotic administration.3 Diarrhoea is thought to be clinically significant if there are more than three loose stools per day,4, 5 although a recent survey in spinal cord injury (SCI) centres found that the definition of diarrhoea and diagnostic criteria of C. diff infection (CDI) vary among SCI centres.6 In addition, diarrhoea after SCI is often complicated by spurious diarrhoea due to underlying constipation.
AAD occurs in about 5–25% of adult patients on administration of antibiotics.4 C. diff-associated diarrhoea (CDAD) occurs most often as a consequence of disruption of the gut microbiota following a broad spectrum of antibiotic treatment. CDAD accounts for 20–30% of AAD, although some estimates are more conservative.3, 7 In the majority of patients,8 full recovery is usual, although particularly elderly and frail patients may suffer loss of dignity, become seriously ill with dehydration as a consequence of diarrhoea and may progress to develop life-threatening pseudomembranous colitis.
Exposure to antibiotics within the previous three months is thought to be one of the most important risk factors for developing CDAD. Other well-recognised risk factors include age,9 hospitalisation,9 severity of underlying illness,9 use of proton pump inhibitors (PPIs),9 malnutrition risk10 and seasonal variation.11 However, this may not be a characteristic that is shared among all patient groups.12 SCI patients are at higher risk of hospital-acquired infections because of longer hospital stay for acute and rehabilitation stay.12 Newly injured SCI patients require anticoagulation therapy to prevent venous thromboembolism. This increases the risk of gastric ulcers; therefore, patients commonly receive a PPI to protect the stomach against this adverse effect. Literature reports show that patients on PPIs have a relative risk of 69% of contracting C. diff against patients who are not taking the medication.13 In addition, increased use of invasive devices such as urinary catheters increases the risks of infections.12 AAD/CDAD can complicate any pressure ulcer management as it contributes moisture and bacteria. Recurrent diarrhoea also depletes the body of electrolytes which are key in wound healing such as potassium, or during chronic episode micronutrients such as magnesium and zinc.14 This is through direct loss, but also via malabsorption. Diarrhoea causes dehydration and malnutrition with further medical consequences.15
The objective of this study was to (1) record the use of antibiotics; (2) establish the prevalence of AAD and CDAD and; (3) assess whether there is any seasonal variation on infections and prevalence of AAD in a UK leading SCI centre.
Materials and methods
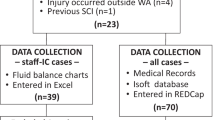
This was a one-year, retrospective, point-prevalence study. The data were collected from the National Spinal Injuries Centre at Stoke Mandeville Hospital, UK during October 2014–June 2015. A 30-item cross-sectional questionnaire was distributed to the SCI centre’s clinicians. The questionnaire consisted of three sections: the first section was collecting individual’s baseline demographics, level and cause of SCI, presence of co-morbidities and routine blood biochemistry. The second section was collecting the number of medications and whether patients are on antibiotics. The indication for starting antibiotics, dose, route and frequency of antibiotics, use of PPI, H2 blocker, laxatives and anti-diarrhoeal agents were also collected. The last section was aimed at occurrence of diarrhoea and C. diff infection.
We define AAD as 2 or more watery stools type 5, 6 or 7 (Bristol stool scale) over 24 h.5 CDAD was diagnosed by a positive C. difficile toxin A and B in stool samples.
Formal ethical permission to conduct the study was not required by the Institution’s review board as this was considered to be a clinical audit not involving active patient participation.16 The questionnaires were approved by the local clinical audit departments. In addition, we tested the pilot questionnaire on three patients to assess the content and time required to complete the questionnaire; feedback from this guided the drafting of the final version of the questionnaire (Supplementary Information). Completed questionnaires were anonymised before data input and analysis.
The intensity of antibiotic exposure was used to categorise patients into those on relatively low-risk antibiotics (metronidazole and parenteral aminoglycosides), those on ‘medium-risk’antibiotics (tetracyclines, sulphonamides, macrolides and quinolones) and those on ‘high-risk’ antibiotics (aminopenicillin and cephalosporins), using the criteria described elsewhere.17
In order to analyse the seasonal variation of AAD, CDAD and infections caused, we collected data from all in-patients from four different time points (1) 1st October 2014: Autumn; (2) 1st February 2015: Winter; (3) 6th April 2015: Spring; and (4) 1st June 2015: Summer.
Statistical analysis
The prevalence of AAD and CDAD was obtained by dividing the total number of patients who had developed AAD/CDAD by the total number of patients studied during the study period. Descriptive statistics were used to calculate response frequency. Data were reported as mean (s.d.) or median (ranges). χ2 tests were used to compare differences in the distribution of qualitative variables. Differences in quantitative variables, according to their distribution, were analysed by the parametric t-test or the non-parametric Mann–Whitney test. Univariate linear regression analysis of the occurrence of AAD was then undertaken. Those which were significant (P<0.05) were entered into a multivariate analysis to determine which made a significant unique contribution to AAD. As only a small number of CDAD, multiple binary logistic regression analysis was used to determine significant predictors for AAD, and effect estimates were presented as the odd ratios (OR) and 95% confidence intervals (CI). For all tests, a P-value of 0·05 or less or when the 95% CI for OR did not exceed 1 was considered as significant. Statistical analysis was performed using the Minitab statistical software (version 15.0; Minitab, Coventry, UK) and SPSS (version 22.0; IBM Corporation, Armonk, NY, USA).
Results
A total of 319 adults (mean age: 55.9 years, 29.2% female) with SCI (58.2% tetraplegia; 43.7% complete SCI) were studied. Seventy (24.3%) patients were on antibiotics; the top five indications for antibiotics were urinary tract infections (n=16, 20.5%), pressure ulcers/wound infections (n=12, 15.6%), skin infection (n=12, 15.6%), nail infection (n=8, 10.4%) and osteomyelitis (n=7, 9.1%; Table 1). Urinary tract infections were found to be more common in the autumn season (50%) when compared with winter (14.3%), spring (5%) and summer (11.8%), respectively (P<0.001; Table 1)
Seventeen of 78 patients on antibiotics (21.8%) developed diarrhoea (AAD). This is significantly higher when compared with those not on antibiotics (5.8%; Table 2). Patients who received antibiotics tended to take more medications (13 vs 10, P<0.01) and had a higher C-reactive protein (18 vs 8.1, P<0.001; Table 2). No significant difference was found in the number of older adults, severity of SCI (number of cervical injury and number of complete SCI), serum albumin level, mean white cell counts, proportions of patients using PPI, H2 blocker, laxatives and anti-diarrhoeal agents (Table 2).
AAD was not significantly associated with longer duration of antibiotic therapy (mean duration, 16 days for patients with AAD vs 14 days for those without AAD, P=0.610; Table 3). A total of 44.2% patients received multiple antibiotics. Patients tended to develop AAD if they were on multiple antibiotics (70.6% in-patients with AAD vs 35.8% for those without AAD, P=0.023). The most frequently used antibiotics regimen that was associated with AAD were tazocin, clindamycin and flucoxacillin. Overall, 52.9% of patients who had developed AAD were found to be on high-risk antibiotics compared with 37.7% of patients on low-risk antibiotics, P=0.397 (Table 3).
AAD was more common in the summer season when compared with spring, autumn and winter. (47.1, 10, 10, 23.8%, P=0.025; Table 1) AAD was associated with older adults aged 65 years or above (70.6% vs 31%, P=0.003) and tetraplegia (76.5% vs 44.4%, P=0.021). In addition, patients with AAD tended to have a lower serum albumin level (24.5 vs 31.5 g l−1, P<0.001).
The binary multivariate logistic regression analysis identified the polypharmacy (OR: 1.17, 95% CI: 1, 1.37) and summer season (OR: 14.45, 95% CI: 1.17, 178.1) as the unique risk factor for AAD (Table 4).
As only a small number of patients developed CDAD (n=3), this form of analysis was deemed inappropriate for the CDAD data.
Discussion
The purpose of this study was to establish the prevalence and assess whether seasonal variation affects the occurrence of AAD and CDAD among SCI patients. The prevalence of AAD was 22.1% and CDAD was 1.3%. This is comparable with the reported prevalence of AAD3 and CDAD7 in general populations and previous studies conducted in SCI centres.15 Our study found that summer season and polypharmacy are unique predictors for AAD.
Antibiotic administration causes alternation in intestinal microbiota, which results in the loss of physiologic processes involving the metabolism of nutrients. Under normal circumstances, non-absorbable carbohydrates are metabolised by anaerobic colonic bacteria as an energy source. As metabolism occurs, lactic acid and short-chain fatty acids (SCFAs) such as butyrate are produced. Fluid, electrolytes, and SCFAs are absorbed, with only small amounts of these organic acids remaining in the colon. Undigested non-absorbable carbohydrates, organic acids and cations accumulate, causing osmotic diarrhoea. Multiple antibiotics have been implicated in reduced colonic bacterial carbohydrate metabolism. Clindamycin has been shown in vitro to decrease faecal carbohydrate metabolism as well as concentrations of SCFA. Ampicillin, metronidazole, dicloxacillin and erythromycin have also been implicated in causing reduced faecal concentrations of SCFA.4 Our data found that a higher proportion of patients who developed AAD were on higher-risk antibiotics, but we failed to find any statistical association.
Another pathway that could be significantly affected by antibiotic administration involves the synthesis of primary bile salts. If bile salts are not absorbed in the small bowel, bile salts will be dehydroxylated to secondary bile acids by bacteria in the colon. These secondary bile acids are potent colonic secretory agents, and presence in the colon can cause secretory diarrhoea. In addition, the increase in colonic pH caused by decreased carbohydrate metabolism results in increased solubility of dehydroxylated secondary bile salts, so these mechanisms may actually work in synergy to cause AAD.4
The present study found the prevalence of CDAD was low in comparison to that in previous reports.6, 10, 11 The fall in CDAD prevalence could be due to the continuing year-on-year fall of overall Clostridium difficile infection cases in British hospitals. Indeed, the overall CDI rate for England in the UK has fallen from 4.85 per 10 000 in 2009 to 2.29 per 10 000 in 2013.18 In addition, the low prevalence of CDAD could be due to short study time period and point-prevalence nature of the study.
Risk factors associated with CDI have been investigated in many studies. Prior antimicrobial use is a well-known risk factor for developing CDI. Antimicrobials alter the healthy faecal microbiome, allowing C. diff to colonise, overgrow and produce toxins if a C. diff exposure occurs before the faecal microbiome is able to return to a healthy state. Traditionally, clindamycin has been associated with CDI, and it remains an important predisposing risk factor today.19 Exposure to gastric acid suppressive agents has also been identified as a risk factor associated with CDI.20 The mechanism of action of gastric acid suppression in the causal pathway of CDI is not fully known. As an obligate anaerobe, the vegetative cells of C. diff die within minutes after exposure to air. Therefore, C. diff acquisition involves the ingestion of C. diff spores, which are resistant to gastric acid. Rather than being in the causal pathway of CDI, gastric acid suppression may be a surrogate marker for patients at increased risk of CDI.21 Because of limited case in the present study, we were not able to analyse potential risk factors for CDAD but, apart from the traditional risk factors, our study found summer season and polypharmacy may be additional risk factors for AAD.
This study has some limitations. First, the present study did not judge whether the use of antibiotic was appropriate; therefore, it may overestimate the use of antibiotic. The selection of the SCI centre (SCIC) was at discretion of the study authors. However, the SCI centre (National Spinal Injuries Centre at Stoke Mandeville Hospital) selected is the largest SCI centre (115 beds) in the UK and represented ~25% of the SCIC’s beds in the UK. Therefore, results derived from this sample of SCICs could be considered representative or at least serve as a pilot study. To include one large SCIC may prevent the differences on antibiotic prescription and bowel management programme between SCICs. Previous research has found that different definitions of diarrhoea have been used in different SCICs in the UK and other European SCI centres.6 Indeed, to use a standardised definition of diarrhoea would not just help in identifying and treating patients with SCI but also allowing bench marking with other SCI centres and to enable future AAD/CDAD research.
Conclusions
The present study found AAD is common in SCI patients and may be a risk factor for poorer outcome and increased hospital cost. A multicenter study is planned to establish the prevalence and risk factors for AAD/CDAD.
Data Archiving
There were no data to deposit.
References
Parvez S, Malik KA, Ah Kang S, Kim YH . Probiotics and their fermented food products are beneficial for health. J Appl Microbiol 2006; 100: 1171–1185.
Dendikuri N, Costa V, McGregor M, Brophy J . Probiotic therapy for the prevention and treatment of Clostridium difficile-associated diarrhoea: a systematic review. CMAJ 2005; 173: 167–170.
Bartlett JG . Antibiotic-associated diarrhea. N Engl J Med 2002; 346: 334–339.
Hogenauer C, Hammer HF, Krejs GJ, Reisinger EC . Mechanisms and management of antibiotic-associated diarrhea. Clin Infect Dis 1998; 27: 702–710.
O’Donnell LD, Virjee J, Heaton KW . Detection of pseudodiarrhoea by simple clinical assessment of intestinal transit time. Br Med J 1990; 300: 4390440.
Wong S, Saif M, O’Driscoll J, Kumar N, Smith E, Roels E et al. Use of probiotics in preventing antibiotic associated diarrhoea and Clostridium difficile associated diarrhoea in spinal injury centres: an international survey of four European countries. Int J Probiotics Prebiotics 2015; 10: 85–90.
McFarland LV . Update on the changing epidemiology of Clostridium difficile-associated disease. Nat Clin Pract Gastroenterol Hepatol 2008; 5: 40–48.
Cohen J, Limbago B, Dumyati G, Holzbauer S, Johnston H, Perlmutter R et al. Impact of changes in Clostridium difficile testing practices on stool rejection policies and C difficile positively rates across multiple laboratories in the United States. J Clin Microbiol 2014; 52: 632–634.
Department of Health/Health Protection Agency. Clostridium difficile infection: how to deal with the problem. Department of Health and Health Protection Agency (2008). Available at https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/340851/Clostridium_difficile_infection_how_to_deal_with_the_problem.pdf. Accessed on 18 September 2016.
Wong SS, O’Driscoll J, Weldon M, Yau CY . Nutritional status predicts hospital length of stay and mortality in patients with Clostridium difficile C. diff infection. Proc Nutr Soc 2010; 69: E175.
Davenport E, Mizrahi-Man O, Michelini K, Barreiro L, Ober C, Gilad Y . Seasonal vatiation in human gut microbiome composition. PLoS ONE 2014; 9: e90731.
Evans CT, LaVela SL, Weaver FM, Priebe M, Sandford P, Niemiec P et al. Epidemiology of hospital-acquired infections in veterans with spinal cord injury and disorders. Infect Control Hosp Epidemiol 2008; 29: 234–242.
Barletta J, Sclar D . Proton pump inhibitors increase the risk for hospital-acquired Clostridium difficile infection in critically ill patients. Crit Care 2014; 18: 714.
Consortium for Spinal Cord Medicine Pressure Ulcer Prevention and Treatment Following Spinal Cord Injury: A Clinical Practice Guideline for Health-Care Providers 2nd edn. Paralyzed Veterans of America: Washington, DC, USA. 2014.
Wong S, Jamous A, O’Driscoll J, Sekhar R, Weldon M, Yau CY et al. A Lactobacillus casei Shirota probiotic drink reduces antibiotic-associated diarrhoea in patients with spinal cord injuries: a randomised controlled trial. Br J Nutr 2014; 111: 672–678.
Health Research Authority Defining Research. NRES guidance to help you decide if your project requires review by a Research Ethics Committee. Available at http://www.hra.nhs.uk/documents/2013/09/defining-research.pdff. Accessed on 10 April 2016.
Kelly CP, LaMont JT . Clostridium difficile infection. Annu Rev Med 1998; 49: 375–390.
Public Health England. Infection report. Vol. 8. Available at: https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/339374/Clostridium_difficile_voluntary_surveillance_2013.pdf (2014). Accessed on 20 December 2015.
Bartlett JG . Clostridium difficile: history and its role as an enteric pathogen and the current state of knowledge about the organism. Clin Infect Dis 1994; 18 (Suppl 4): S265–S272.
Dubberke ER, Reske KA, Yan Y, Olsen MA, MCDonald LC, Fraser VJ . Clostridium difficile-associated disease in a setting of endemicity: identification of novel risk factors. Clin Infect Dis 2007; 45: 1543–1549.
Lowe DO, Mamdani MM, Kopp A, Low DE, Juurlink DN . Proton pump inhibitors and hospitalisation for Clostridium difficile-associated disease: a population-based study. Clin Infect Dis 2006; 43: 1272–1276.
Acknowledgements
All authors contributed to the report. We would like to thank Sunna Aslam, Lydia van Hamel-Parsons and Edmund Chiu for data collection. We are grateful to all medical-staff facilitating the data collection and Janine Turner for proof-reading the manuscript.
Author contributions
SW—Protocol development, questionnaire development, data analysis and manuscript preparation; PS—data input and manuscript revision; JO—data interpretation and manuscript revision; SH—data analysis, data interpretation and manuscript revision; AJ—data interpretation, manuscript revision; MS—questionnaire development, data interpretation and manuscript revision.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Parts of the study data were submitted to present at the BritSpine in April 2016, American Spinal Injury Association annual conference in April 2016 and International Spinal Cord Society meeting in September 2016.
Supplementary Information accompanies this paper on the Spinal Cord website
Supplementary information
Rights and permissions
About this article
Cite this article
Wong, S., Santullo, P., O'Driscoll, J. et al. Use of antibiotic and prevalence of antibiotic-associated diarrhoea in-patients with spinal cord injuries: a UK national spinal injury centre experience. Spinal Cord 55, 583–587 (2017). https://doi.org/10.1038/sc.2016.193
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2016.193
This article is cited by
-
Identifying prescribers of antibiotics in a primary care spinal cord injury cohort
Spinal Cord Series and Cases (2024)
-
Lactobacillus casei Shirota probiotic drinks reduce antibiotic associated diarrhoea in patients with spinal cord injuries who regularly consume proton pump inhibitors: a subgroup analysis of the ECLISP multicentre RCT
Spinal Cord (2024)
-
Study protocol of a double-blind randomised placebo-controlled trial on the effect of a multispecies probiotic on the incidence of antibiotic-associated diarrhoea in persons with spinal cord injury
Spinal Cord (2020)
-
An update on the human and animal enteric pathogen Clostridium perfringens
Emerging Microbes & Infections (2018)