Abstract
Study design:
A retrospective study.
Objectives:
The aim of this study was to investigate the contribution of laser-evoked potentials (LEPs) and quantitative sensory testing (QST) to the diagnosis of neuropathic pain in patients with spinal cord injury (SCI) and inconclusive magnetic resonance imaging (MRI) findings.
Setting:
A multidisciplinary pain center.
Methods:
QST (DFNS protocol) and Tm-YAG-laser stimulation of the skin were applied within the pain site corresponding with dermatomes of altered sensation. Available MRI scans were reviewed.
Results:
Thirteen individuals (50±16 years) with SCI were examined. In four cases with no detectable neural lesion on MRI, all QST but three LEP were abnormal. In four patients with poorly defined spinal lesion on MRI, all QST but three LEP only were abnormal. In four cases where pain was not matching adequately with MRI lesions, all patients had abnormal LEP and QST. In one patient showing a spinal cord atrophy, LEP was normal but QST was abnormal. Findings supported the diagnoses at-level (n=5) and below-level (n=8) SCI pain. Spinothalamic tract function assessed by LEP was normal in three cases, but QST was abnormal in all cases.
Conclusions:
As QST is a psychophysical examination depending on patient cooperation, we suggest that the combination of QST and LEP might be a valuable diagnostic tool to detect lesions of the somatosensory system in a subgroup of patients with neuropathic spinal cord injury pain and inconclusive MRI findings.
Similar content being viewed by others
Introduction
It has been recognized that pain contributes significantly to suffering, poorer rehabilitation outcomes and reduced quality of life in people with spinal cord injury (SCI).1 About one-third of patients with SCI develop severe pain,2 and pain is likely to be present over several years.1 Besides the high prevalence of musculoskeletal pain (59%), at-level and below-level SCI neuropathic pains are found frequently (41% vs 34%) in individuals with SCI consulting a neurorehabilitation center2 and about similar data are reported from a multidisciplinary pain center.3 In general, the treatment of neuropathic pain remains unsatisfactory.4 The diagnosis of neuropathic pain in SCI is particularly challenging. The International Spinal Cord Injury Pain Classification suggests diagnostic criteria of different types of pain including neuropathic pain in SCI based on clinical criteria only.5 According to the definition of neuropathic pain as ‘pain arising as a direct consequence of a lesion or disease affecting the somatosensory system’, diagnostic criteria with a grading system of definite, probable and possible neuropathic pain have been proposed,6, 7 as well as diagnostic criteria for neuropathic pain in patients with SCI.8 These include criteria for SCI as a ‘history of a relevant lesion or disease affecting the spinal cord and/or cauda equina and at least one diagnostic test confirming a lesion or disease of the spinal cord and/or cauda’, criteria for SCI-related neuropathic pain as ‘pain located at or below the neurological level of the SCI, negative or positive sensory signs in the area of pain compatible with the spinal cord or root lesion and other causes of pain, such as nociceptive or peripheral neuropathic pain, excluded or considered highly unlikely’. Magnetic resonance imaging (MRI) is the method of choice to diagnose spinal lesions in patients with SCI.9 In fact, a small number of patients with clinical symptoms of traumatic myelopathy but no radiographic or computed tomographic features of SCI can be found. This constellation is called ‘Spinal Cord Injury Without Radiographic Abnormality’ (SCIWORA) and its prevalence has been reported in children for 6–19% and in adults for 9–14%. SCIWORA is mostly found in the cervical spine and much less frequently in the thoracic or lumbar spine.10 Since the introduction of MRI into the diagnostic of SCI, the term ‘Spinal Cord Injury Without Neuroimaging Abnormality’ (SCIWNA) is suggested.11 In this situation, neurophysiology assessment may add diagnostic information. Several neurophysiological investigations in SCI have been evaluated for afferent (somatosensory-evoked potentials, contact heat-evoked potentials and others) and efferent pathways (motor-evoked potentials).12, 13
Electrophysiological investigations in SCI can complement clinical evaluation by providing improved diagnosis.12 For the diagnosis of neuropathic pain, investigations of the somatosensory system are suggested.6 Laser-evoked potentials (LEPs) are a recognized method to detect subcortical lesions of the A-delta fiber pathway, which are pain and temperature transmitting pathways.14 Data about LEP applications in central lesions in various diseases including those of the spinal cord15 and in several demyelinating diseases of the central nervous system are published.16 Quantitative sensory testing (QST) has been standardized for reference regions17, 18, 19 and is widely used in research on chronic pain.20 In clinical setting, QST can be used to monitor somatosensory deficits20 and in research for pain phenotyping.21, 22 Several data regarding QST in SCI have already been published23, 24, 25, 26, 27 mainly in subacute populations and bedside methods. As shown in a pilot study with four patients with spinal lesions (neurosarcoidosis, multiple sclerosis or neuromyelitis optica), QST, performed according to the protocol of the German Network on Neuropathic pain (DFNS), was less sensitive than LEP to find sensory loss and LEP detected more deficits ‘than any single QST parameter or their combination into somatosensory profiles’.16 These authors recommended larger scale studies combining LEP and QST.16
On the basis of this recommendation, the aim of this study was to evaluate the additional contribution of LEP and QST in diagnosis of neuropathic SCI pain in patients with inconclusive MRI findings and evaluation of the somatosensory system in patients with chronic neuropathic SCI pain.
Materials and methods
Setting and subjects
For this retrospective study, clinical records of patients with the diagnosis of SCI pain referred to a multidisciplinary pain center in Switzerland from January 2011 to December 2013 have been reviewed. Patients had been referred to the center for pain diagnosis and pain management. Inclusion criteria were as follows: (1) injury of the spinal cord related to a traumatic event or degenerative spinal disease, (2) a supposed diagnosis of neuropathic at-level or below-level SCI pain, (3) the presence of combined investigation using LEP and QST, (4) LEP and QST applied to the region affected by suggested neuropathic SCI pain including the presence of impaired or residual sensation and (5) availability of MRI scans (magnetic resonance imaging). Exclusion criteria were (1) other underlying neurological disorders,(2) either LEP or QST investigation only and(3) incomplete data. LEP and QST measurements are established methods in our clinical setting to assist the diagnostics of neuropathic pain.
There was no need for an ethical request for irrevocably anonymized retrospective studies according to the National Human Research Ordinance of Switzerland.28 We certify that all applicable institutional and governmental regulations concerning the ethical use of human were followed during the course of this research.
Demographic, clinical and pain-related data
Demographic data included basic personal data (age, gender) and general questions regarding SCI (cause of injury, time since injury), as well as medication on admission to the pain center. The assessment of neurological function after SCI was performed by a neurologist (G.L.) according to the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI).29 These recommendations include the neurological status according to the American Spinal Injury Association with determination of the neurological level of injury (NLI) and the extent of injury according to the ASIA Impairment Scale (AIS grade). Finally, the diagnosis of suspected at- or below-level SCI pain was clinically done by a neurologist while matching the detailed pain history, patient's pain drawings showing the pain sites and the complete neurological examination including American Spinal Injury Association score with the pain characteristics given by the International Spinal Cord Injury Pain classification.5
According to the policy of our pain center, patient-reported outcomes were collected by the standardized German pain questionnaire, designed by the German Association for the Study of Pain.30 This questionnaire contains parameters such as the time since occurrence of pain, the pain-related disability, the psychological status and general health. The psychological status was assessed by the use of the Hospital Anxiety and Depression Scale. Health-related quality of life was determined by the SF-12 questionnaire.31 It has been validated for patients with SCI.32 Chronic pain severity was assessed using the Graded Chronic Pain Scale.33 Pain intensity was taken from this questionnaire, which is calculated by the average of actual pain, worst pain and average pain. The disability subscale has been validated for people with SCI.34 The grade of pain chronification was defined by the Mainz Pain Staging System.35
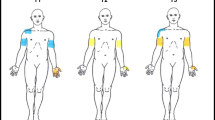
Test sites
In patients with incomplete spinal lesions (AIS B, C and D), the test sites for LEP and QST were chosen according to clinical pain presentation matching with the area of impaired sensation on clinical neurological examination. Patients with a complete SCI lesion (AIS A) could only be examined if pain was present within the zone of partial preservation where sensation is impaired and which lies between NLI and the distal area of abolished sensation. The degree of motor impairment and autonomic impairment had no impact on choosing the test sites.
Although LEP and QST were recorded from right and left body sides, for the analysis of this study one body side was taken into account. For the analysis, according to our daily clinical routine, the side of pain was chosen or if bilateral pain was present the side of worse pain or if pain was equal on both sides, data from the right body side were taken.
Laser-evoked potential
The method was performed as described previously,36 using a Tm-YAG laser machine-type Themis Terminal V.1.0 (StarMedTec GmbH, Starnberg, Germany). At first, laser sensory and laser pain thresholds were obtained using the method of levels. Therefore, patients were asked to rate the stimulus as ‘painful perceived’, ‘perceived, but non painful’ or ‘not perceived’. To familiarize the patient with the method, laser stimuli were applied above the pain threshold, starting from 600 mJ with decreasing steps of 60 mJ until the stimulus was not perceived; subsequently, the intensity was increased until the stimulus was reported as ‘painful’ and then decreased again. This procedure was undertaken three times. The laser sensory threshold was estimated as the average of laser intensity between ‘not perceived’ and ‘first perceived’ and the pain threshold was estimated as the average of laser intensity between ‘painful’ and ‘not painful’. In three patients (nos 1, 4 and 13), sensory thresholds were not determined because of a different investigation protocol.
Cortical LEPs were recorded given a randomized application of two different laser intensities alternating randomly between 480 and 540 mJ for hand and trunk and between 540 and 600mJ for legs and feet. The interstimulus interval was randomized by the machine lasting between 7 and 15s. The impedance was maintained below 5 kΩ and bandpass-filtered data (0.2–100 Hz) acquired simultaneously at a sampling rate of 500 Hz (Nicolet Biomedical Inc., Madison, WI, USA). Patients were asked to lay relaxed, to fix a sign on the ceiling and to avoid eye-blinking. Cortical responses were recorded with Ag/AgCl electrodes from Cz based on the international 10–20 system versus linked earlobes (A1/A2). The laser beam was slightly displaced randomly to avoid sensitization and habituation. The pain intensity of each laser stimulus was noted using numeric rating scale (0–10, with 0=‘no pain’ and 10=‘worst pain imaginable’). Late LEP components as latencies N2 and P2 (ms, measured from stimulus onset to peak) as well as N2/P2 amplitude (μV, peak to peak) were obtained using a neurophysiology machine, type VikingSelect and version 12 (Nicolet Biomedical Inc.). Data were stored on disk for off-line analysis. The time window for analysis was 2500 ms according to laser stimulus onset. All trials containing artifacts were rejected from subsequent analysis after visual inspection. Remaining trials were time averaged. Results were compared with normal values from the literature.36
Quantitative sensory testing
QST was performed in accordance with the protocol of the DFNS17 by an experienced medical technician (L.S.) who underwent a training program certified by DFNS. For thermal parameters, a standardized diagnostic device (TSA-II; Medoc, Ramat Yishai, Israel; temperature range: 0–50 °C, baseline temperature 32 °C) with a 9.0 cm2 contact surface of the thermode and related computer software (version 5.35) was used. Thermal tests were performed, including cold detection threshold (CDT), warm detection threshold (WDT), cold pain threshold (CPT) and heat pain threshold (HPT). Furthermore, the thermal sensory limen (TSL) was obtained, a thermal difference limen using alternating cool and warm stimuli, and the number of reported paradoxical heat sensations (PHS) were recorded. The mechanical testing included the mechanical detection threshold (MDT), using a standardized set of modified von Frey hairs (Opti-hair2-Set; Marstock Nervtest, Schriesheim, Germany), the mechanical pain threshold (MPT), using calibrated pinpricks (MRC Systems, Heidelberg, Germany), the vibration detection threshold (VDT), using a Rydel-Seiffer tuning fork (64 Hz), which was applied over prominent bones near the testing area and the pressure pain threshold (PPT) measured over muscles within or near the investigation area using the pressure algometer (FDN200; Wagner Instruments, Greenwich, CT, USA). On the trunk, PPT was not performed routineously. PPT was not tested over muscles with underlying ribs because of suggested risk of osteoporotic rib fractures during application of pressure or over abdominal muscles with no underlying bone as resistance. Mechanical pain sensitivity (MPS) and dynamic mechanical allodynia (DMA) were assessed by applying pinprick stimuli and slight tactile stimuli (cotton wisp, 3 mN; Q-tip, 100 mN; soft brush, 200–400 mN; Somedic, Hörby, Sweden) in a standardized randomized order. Pain summation to repetitive pinprick stimuli (wind up ratio, WUR) was assessed as a ratio between a single pinprick stimulus and a series of 10 repetitive applications of the same stimulus intensity in a frequency of 1/s. For MPS, DMA and WUR patients were asked to rate the stimuli on a numeric rating scale (0=no pain, pricking, stinging or burning sensation, 100=maximal pain imaginable). The results for each parameter were calculated according to the published recommendation.17 The loss and gain score (LOGA score) was calculated according to Maier et al.,37 but side-to-side differences were not included because of bilateral nerve damage.
Magnetic resonance imaging
Available MRI scans were reviewed by a spine radiologist (M.F.B.). MRI results were assigned to four different groups: (1) ‘no detectable neural lesion’, (2) ‘poorly defined spinal cord or cauda equina lesion with questionable affection of the somatosensory system’, (3) ‘questionable match between MRI lesion and SCI pain site or pain presentation’ or (4) ‘atypical lesion with spinal cord atrophy only’.
Statistical analyses
Data analysis was carried out using the SPSS software (IBM SPSS Statistics for Windows, Version 21.0; IBM Corp., Armonk, NY, USA). A descriptive analysis was performed on the demographic, clinical and SCI characteristics. Data are reported as means and standard deviations. All data were evaluated in an anonymized manner.
Results
Demographic data, clinical data and MRI
A review of medical records of 62 patients with SCI who were referred for pain treatment to our clinic from January 2011 to December 2013 revealed that 13 patients (3 women and 10 men) had evaluations with combined LEP and QST examinations being carried out. The causes of SCI were spinal trauma (n=9), degenerative spinal canal stenosis (n=1) and SCI following perioperative complications (n=3). The summary of the clinical characteristics (age, age at injury, AIS grades, time since injury, pain duration and pain medication) is shown in Table 1, and the outcomes of the self-administered questionnaires are given in Table 2. Here, 12 patients could be included for evaluation only because of missing the questionnaire data set in patient no. 12. The reason to perform LEP and QST was inconclusive MRI findings (see below). After demonstration of a lesion of the somatosensory system by abnormal LEP and/or QST, five of the paraplegic patients could be diagnosed suffering from at-level SCI pain and two from below-level SCI pain, whereas all six tetraplegic patients could be diagnosed having below-level SCI pain. For detailed clinical data of each patient (injury etiology, lesion level, NLI, type of paralysis, AIS, SCI pain subtype, pain site, examination site and MRI result) refer to Table 3.
Laser-evoked potential
Cortical LEP were abnormal in 9/13 patients (absent potential in 8/13, prolonged latencies N2 in 1/13). Laser sensory thresholds were abnormal in 4/13 (absent 2/13, increased 2/13, not performed in 3/13). Laser pain thresholds were abnormal in 5/13 patients (absent 4/13, increased 1/13). Cortical LEP were abnormal in 5/8 patients with below-level SCI pain and in 4/5 with at-level SCI pain. Laser sensory thresholds were abnormal in 3/7 patients (not examined in one) with below-level SCI pain and in 2/3 (in 2 not examined) with at-level SCI pain. Laser pain thresholds were abnormal in 4/8 patients with below-level SCI pain and in 1/5 with at-level SCI pain consistent with loss of function. Considering all laser parameters (including latencies, amplitudes, laser sensory and laser pain thresholds), only 2/13 had completely normal results (2 patients with below-level SCI pain). In one further patient with at-level SCI pain, latencies, amplitude and laser pain threshold were normal but laser sensory threshold was not examined. For this latter patient, the LEP was rated as normal (Table 4).
Quantitative sensory testing
The function of the spinothalamic tract (STT) was assessed for thermal parameters such as CDT, WDT, TSL, PHS, CPT and HPT and for mechanical parameters such as PPT, MPT, MPS, DMA and WUR. All patients showed at least one abnormal STT parameter (Table 4). The most frequently affected STT parameter with loss of function was TSL (8/13), WDT (6/13) and CDT (4/13), whereas CPT, HPT and PPT never showed loss of function. The most frequently affected STT parameter for gain of function were MPT (4/13) followed by PPT and MPS (3/13) and DMA (2/13). CDT, WDT and WUR never showed gain of function. The function of DCS was assessed for mechanical parameters MDT and VDT. Abnormal DCS parameters were found in 11/13 patients. The most affected DCS parameter for loss of function was VDT (11/13), whereas MDT was slightly less affected (8/13). No gain of function for DCS was seen. In three patients, PPT was not tested because in dermatome T6, T8 and T10 there is no appropriate muscle to test. WUR could not be investigated in four patients according to the protocol, because the used 256 mN pinprick was ‘not’ or ‘not painful’ perceived. All QST parameters except WUR were affected in a different degree ranging between 1 (CPT, gain) and 11 times (VDT, loss). Parameters that most frequently showed both loss or gain were MPT (3 loss, 4 gain) and MPS (2 loss, 3 gain). Eight different LOGA scores were estimated. The most frequent LOGA scores were L3G2 and L3G0, which occurred in three, whereas L2G0 occurred in two patients only. Six out of 13 patients showed LOGA scores with loss and gain of function (four different scores). LOGA scores with loss of function only occurred in five patients (L3G0 in 3, L2G0 in 2). LOGA scores with gain of function only occurred in two patients (L0G3 in 1, L0G2 in 1). QST in patients with below-level and at-level SCI pain did not show major differences. In average, patients with below-level SCI pain had 4.9 abnormal parameters and with at-level SCI pain had 4.2 abnormal parameters.
Usefulness of LEP and QST in diagnostic workup
In all four patients (nos 1–4) belonging to the MRI group ‘no detectable neural lesion on MRI’, both LEP (except patient no. 3) and QST were abnormal. This could suggest that LEP and QST have an additional diagnostic contribution to establish the diagnosis of a spinal lesion. On QST in this group, loss and gain signs were found in two patients (L3G1 and L2G2), whereas two had loss only (L2G0). LEP in patient no. 1 was abnormal regarding laser pain threshold only. Four patients were assigned to the MRI group ‘poorly defined spinal cord or cauda equina lesion with questionable affection of somatosensory system’ (nos 5–8). In this group, absent cortical LEP were shown in three patients, whereas LEP (including cortical LEP and thresholds) in one was completely preserved (patient no. 6). QST revealed LOGA scores L3G2 in two, but L3G0 in two patients, also confirming a lesion of the somatosensory system. In four patients with ‘questionable match between MRI lesion and SCI pain site or pain presentation’ (nos 9–12), all patients had abnormal LEP, and on QST, a combination of loss and gain of function was found in two, but loss or gain only in two patients suggesting a lesion of the somatosensory system. In one patient with ‘atypical lesion with spinal cord atrophy only’ (no. 13), LEP was normal but LOGA score was L0G2, suggesting the involvement of somatosensory pathways.
When comparing both techniques, LEP as a test for STT function was abnormal in 10 cases (including cortically evoked potentials and thresholds), but QST showed abnormalities in all cases for STT function.
Discussion
The aim of this study was to evaluate the additional contribution of LEP and QST in diagnosis of neuropathic SCI pain in patients with inconclusive MRI findings and the evaluation of the somatosensory system in patients with chronic neuropathic SCI pain.
We could demonstrate that there might be an indication to apply LEP and QST in patients with inconclusive MRI findings to get further information about the function of the somatosensory system. Indeed, in our study, the application of LEP and QST revealed a lesion within the somatosensory system and therefore the diagnosis of neuropathic at-level or below-level SCI pain could be established in all cases. We were able to demonstrate LEP abnormalities in most of the patients, whereas QST abnormalities were found in all patients. Because QST is a psychophysical examination depending on patient cooperation, we suggest that an objective measurement method should be added, which is in line with guidelines on neuropathic pain assessment.14, 38 Therefore, the combination of QST (abnormal in all cases) and LEP (normal in three cases only) might be a valuable diagnostic tool to detect a lesion of the somatosensory system in a subgroup of patients with SCI pain and inconclusive MRI findings.
Demographic and clinical and pain-related data
The present cohort was comparable regarding mean age to the literature of chronic pain patients39, 40 and in comparison with other SCI cohorts similar25 or older.2 The distribution of sex in our cohort (ca. 75% males) was similar to the general SCI population in Switzerland.41 Four (31%) of our patients showed no detectable neural lesion (spinal cord or cauda equina) on MRI scan, and the lesion site was found more often below the cervical level. Three of those patients had evidence of a vertebra fracture or other pathology. Therefore, the SCIWORA could be applied in one case only. Pain intensity was high in our cohort, although high pain intensity is often observed in patients with SCI.2 In our chronic patients’ cohort, we found high stages of chronicity as well as evidence of depression, anxiety and lower quality of life.
LEP in SCI pain
At present, LEP data in traumatic SCI with or without pain have not been studied systematically yet. Nevertheless, a case report of two patients with SCI showed absent CO2-LEP below MRI confirmed lesion,42 and a case series in patients with different chronic inflammatory spinal diseases also showed Thulium-YAG-LEP abnormalities in nearly all cases,16 which is about similar to our findings. Abnormalities on different anatomical levels of CO2-LEP are reported in patients with syringomyelia without pain showing increased or absent latencies and decreased or absent amplitudes or increased pain thresholds.43 In the majority of patients with syringomyelia and pain, CO2-LEP was also absent or abnormal.44 In comparison with these two studies, in our cohort, absent or abnormal cortical LEP were found in about two-thirds of the patients. This could suggest a different pattern of LEP abnormalities in patients with SCI pain, which may be explained by more affected midline crossing STT pathways in syringomyelia. Another study investigated, with several methods including QST and LEPs, the relationship between sensory symptoms and structural and functional lesions of spinal sensory tracts in patients with syringomyelia, with and without central neuropathic pain. In that study, no significant differences were observed between the two groups of patients neither for QST (thermal/mechanical and vibration thresholds) nor for LEP for all tested areas of the upper limbs (i.e. both shoulders and hands), whether painful or not.45 The observed difference was between patients with both spontaneous and evoked pain and patients with no pain or spontaneous pain only. Indeed, the clinical somatosensory impairment was milder in patients with spontaneous and evoked pain than in patients without pain or with spontaneous pain only. Besides LEP, other cortically evoked responses like contact heat-evoked potentials have also been reported in SCI. In SCI patients without and with pain, contact heat-evoked potential were investigated just below the NLI on trunk showing prolonged latencies in both groups without differences.46 In our series, LEP were obtained on more distal dermatomes than just below the NLI. Contact heat-evoked potentials recorded above the NLI in patients with SCI with and without neuropathic pain were not different to healthy controls.47 Contact heat-evoked potentials in patients with incomplete diffuse SCI were reported abnormal in 92% of cases, whereas in 89% abnormalities were found in patients with central and/or anterior cord damage.48
QST in SCI pain
Although LEPs were able to detect lesions in STT, QST allowed to differentiate between loss (negative sensory signs) and gain (positive sensory signs) of function both in STT and DCS. QST has been applied in SCI with and without pain using various methods and reporting different results.23, 24, 25, 26 Here, we used the standardized German DFNS protocol, which has not been applied in SCI systematically yet, except in a single case report,27 in a large number of patients with different neuropathic pain syndromes including central pain37 and in inflammatory spinal lesions.16 This makes comparisons of the results from different studies difficult and by now it is still impossible to give the best early predictor for the neuropathic pain development after SCI.
In our study, every patient showed an individual QST profile, which could potentially mean different underlying pain mechanism(s) and therefore individual approach for treatment. However, at the same time in more than half of the patients, we could find some parameters in common. For example, the most affected parameter indicating sensory loss for STT was TSL. Further thermal detection parameters such as WDT, CDT and PHS were found to be abnormal as well, but in less than half of the patients. Sensory hypersensitivity was found to the less extent: only several patients had gain in mechanical pain parameters such as MPT, PPT and MPS, pointing toward STT dysfunction. DCS impaired function was detected almost in all patients with sensory loss in MDT and/or VDT parameters.
In summary, chronic pain SCI patients from our study showed both thermal and mechanical abnormalities at the same time, which reflected in frequent LOGA, such as L3G2 and L3GO.
Considerations to perform LEP and QST in SCI
In general, MRI should be used whenever a spinal cord lesion or an occult injury is suspected49, 50 and is suggested as the gold standard in assessing spinal emergencies.51 Furthermore, functional and structural multimodal imaging modalities can identify possible abnormalities in the brain regions participating pain modulation in neuropathic pain in patients with SCI pain.52, 53 In inconclusive imaging findings, both LEP and QST can be useful. However, from our study, several issues need to be considered in patients with SCI pain. First, the investigation and the pain site should match and patients should have residual sensation. Therefore, patients with complete SCI lesions can only be investigated when the neuropathic pain is situated within the zone of partial preservation. Second, for people with particularly limited mobility after SCI, a comfortable position has to be considered for examination. Third, for several tests of the QST battery, a horizontal testing area is mandatory. These are tests that require weighted pinpricks (MPT, MPS, ALL, WUR). Because QST as well as the estimation of laser sensory and pain thresholds are psychophysical examinations, patients need to be cooperative and to understand the procedure.
Influence of current pain medication on LEP and QST
We cannot exclude the influence of medication on LEP and QST because this was a retrospective study and all the patients except one were on pain-modulating medications. Several effects of pain-modulating medication on evoked potentials and LEPs have been reported such as a reduction of LEP amplitudes.54, 55, 56, 57, 58, 59, 60 Medication-related changes on QST parameters are also possible but have not been studied systematically. No significant changes were reported after treatment with pregabalin61 and topical lidocaine,21 but for topical capsaicin62 and opioids.63 A tendency for medication-associated sensory changes was also reported.64
Limitations of LEP an QST in diagnostic workup
This is a retrospective study design. Limitations of our study were the low number of patients and the heterogeneity of the cohort with regard to the lesion level, the completeness of the lesion, the pain site, the type of pain (at-level or below-level), findings on MRI and pain medication.
Data Archiving
There were no data to deposit.
References
Siddall PJ . Management of neuropathic pain following spinal cord injury: now and in the future. Spinal Cord 2009; 47: 352–359.
Siddall PJ, McClelland JM, Rutkowski SB, Cousins MJ . A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain 2003; 103: 249–257.
Mahnig S, Landmann G, Stockinger L, Opsommer E . Pain assessment according to the International Spinal Cord Injury Pain classification in patients with spinal cord injury referred to a multidisciplinary pain center. Spinal Cord 2016; 54: 809–815.
Finnerup NB, Sindrup SH, Jensen TS . The evidence for pharmacological treatment of neuropathic pain. Pain 2010; 150: 573–581.
Bryce TN, Biering-Sorensen F, Finnerup NB, Cardenas DD, Defrin R, Lundeberg T et al. International spinal cord injury pain classification: part I. Background and description Spinal Cord 2012; 50: 413–417.
Treede RD, Jensen TS, Campbell JN, Cruccu G, Dostrovsky JO, Griffin JW et al. Neuropathic pain: redefinition and a grading system for clinical and research purposes. Neurology 2008; 70: 1630–1635.
Finnerup NB, Haroutounian S, Kamerman P, Baron R, Bennett DL, Bouhassira D et al. Neuropathic pain: an updated grading system for research and clinical practice. Pain 2016; 157: 1599–1606.
Finnerup NB, Baastrup C . Spinal cord injury pain: mechanisms and management. Curr Pain Headache Rep 2012; 16: 207–216.
Watts J, Box GA, Galvin A, Van Tonder F, Trost N, Sutherland T . Magnetic resonance imaging of intramedullary spinal cord lesions: a pictorial review. J Med Imag Radiat Oncol 2014; 58: 569–581.
Szwedowski D, Walecki J . Spinal Cord Injury without Radiographic Abnormality (SCIWORA)—clinical and radiological aspects. Pol J Radiol 2014; 79: 461–464.
Yucesoy K, Yuksel KZ . SCIWORA in MRI era. Clin Neurol Neurosurg 2008; 110: 429–433.
Curt A, Ellaway PH . Clinical neurophysiology in the prognosis and monitoring of traumatic spinal cord injury. Handb Clin Neurol 2012; 109: 63–75.
Haefeli J, Curt A . Refined sensory measures of neural repair in human spinal cord injury: bridging preclinical findings to clinical value. Cell Tissue Res 2012; 349: 397–404.
Haanpaa M, Attal N, Backonja M, Baron R, Bennett M, Bouhassira D et al. NeuPSIG guidelines on neuropathic pain assessment. Pain 2011; 152: 14–27.
Treede RD, Lorenz J, Baumgartner U . Clinical usefulness of laser-evoked potentials. Clin Neurophysiol 2003; 33: 303–314.
Geber C, Baumgartner U, Fechir M, Vogt T, Birklein F, Treede RD . Comparison of LEP and QST and their contribution to standard sensory diagnostic assessment of spinal lesions: a pilot study. Neurol Sci 2011; 32: 401–410.
Rolke R, Baron R, Maier C, Tolle TR, Treede RD, Beyer A et al. Quantitative sensory testing in the German Research Network on Neuropathic Pain (DFNS): standardized protocol and reference values. Pain 2006; 123: 231–243.
Magerl W, Krumova EK, Baron R, Tolle T, Treede RD, Maier C . Reference data for quantitative sensory testing (QST): refined stratification for age and a novel method for statistical comparison of group data. Pain 2010; 151: 598–605.
Pfau DB, Krumova EK, Treede RD, Baron R, Toelle T, Birklein F et al. Quantitative sensory testing in the German Research Network on Neuropathic Pain (DFNS): reference data for the trunk and application in patients with chronic postherpetic neuralgia. Pain 2014; 155: 1002–1015.
Backonja MM, Attal N, Baron R, Bouhassira D, Drangholt M, Dyck PJ et al. Value of quantitative sensory testing in neurological and pain disorders: NeuPSIG consensus. Pain 2013; 154: 1807–1819.
Demant DT, Lund K, Finnerup NB, Vollert J, Maier C, Segerdahl MS et al. Pain relief with lidocaine 5% patch in localized peripheral neuropathic pain in relation to pain phenotype: a randomised, double-blind, and placebo-controlled, phenotype panel study. Pain 2015; 156: 2234–2244.
Demant DT, Lund K, Vollert J, Maier C, Segerdahl M, Finnerup NB et al. The effect of oxcarbazepine in peripheral neuropathic pain depends on pain phenotype: a randomised, double-blind, placebo-controlled phenotype-stratified study. Pain 2014; 155: 2263–2273.
Finnerup NB, Johannesen IL, Fuglsang-Frederiksen A, Bach FW, Jensen TS . Sensory function in spinal cord injury patients with and without central pain. Brain 2003; 126 (Part 1): 57–70.
Finnerup NB, Sorensen L, Biering-Sorensen F, Johannesen IL, Jensen TS . Segmental hypersensitivity and spinothalamic function in spinal cord injury pain. Exp Neurol 2007; 207: 139–149.
Finnerup NB, Norrbrink C, Trok K, Piehl F, Johannesen IL, Sorensen JC et al. Phenotypes and predictors of pain following traumatic spinal cord injury: a prospective study. J Pain 2014; 15: 40–48.
Zeilig G, Enosh S, Rubin-Asher D, Lehr B, Defrin R . The nature and course of sensory changes following spinal cord injury: predictive properties and implications on the mechanism of central pain. Brain 2012; 135 (Part 2): 418–430.
Westermann A, Krumova EK, Pennekamp W, Horch C, Baron R, Maier C . Different underlying pain mechanisms despite identical pain characteristics: a case report of a patient with spinal cord injury. Pain 2012; 153: 1537–1540.
The Federal Authorities of the Swiss Confederation. Human Research Ordinance. Available at:https://www.admin.ch/opc/en/classified-compilation/20061313/index.html.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med 2011; 34: 535–546.
Nagel B, Gerbershagen HU, Lindena G, Pfingsten M . Development and evaluation of the multidimensional German pain questionnaire]. Schmerz (Berlin, Germany) 2002; 16: 263–270.
Ware J Jr, Kosinski M, Keller SD . A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med care 1996; 34: 220–233.
Wilson JR, Hashimoto RE, Dettori JR, Fehlings MG . Spinal cord injury and quality of life: a systematic review of outcome measures. Evidence-Based Spine-Care J 2011; 2: 37–44.
Von Korff M, Ormel J, Keefe FJ, Dworkin SF . Grading the severity of chronic pain. Pain 1992; 50: 133–149.
Raichle KA, Osborne TL, Jensen MP, Cardenas D . The reliability and validity of pain interference measures in persons with spinal cord injury. J Pain 2006; 7: 179–186.
Gerbershagen U . Organized treatment of pain. Determination of status. Der Internist 1986; 27: 459–469.
Spiegel J, Hansen C, Treede RD . Clinical evaluation criteria for the assessment of impaired pain sensitivity by thulium-laser evoked potentials. Clin Neurophysiol 2000; 111: 725–735.
Maier C, Baron R, Tolle TR, Binder A, Birbaumer N, Birklein F et al. Quantitative sensory testing in the German Research Network on Neuropathic Pain (DFNS): somatosensory abnormalities in 1236 patients with different neuropathic pain syndromes. Pain 2010; 150: 439–450.
Cruccu G, Sommer C, Anand P, Attal N, Baron R, Garcia-Larrea L et al. EFNS guidelines on neuropathic pain assessment: revised 2009. Eur J Neurol 2010; 17: 1010–1018.
Frettloh J, Maier C, Gockel H, Huppe M . Validation of the German Mainz Pain Staging System in different pain syndromes. Schmerz (Berlin, Germany) 2003; 17: 240–251.
de Andres J, de la Calle JL, Perez M, Lopez V . Clinical characteristics, patient-reported outcomes, and previous therapeutic management of patients with uncontrolled neuropathic pain referred to pain clinics. Pain Res Treat 2014; 2014: 518716.
Fekete C, Siegrist J, Reinhardt JD, Brinkhof MW . Is financial hardship associated with reduced health in disability? The case of spinal cord injury in Switzerland. PLoS ONE 2014; 9: e90130.
Iannetti GD, Truini A, Galeotti F, Romaniello A, Manfredi M, Cruccu G . Usefulness of dorsal laser evoked potentials in patients with spinal cord damage: report of two cases. J Neurol Neurosurg Psychiatry 2001; 71: 792–794.
Kakigi R, Shibasaki H, Kuroda Y, Neshige R, Endo C, Tabuchi K et al. Pain-related somatosensory evoked potentials in syringomyelia. Brain 1991; 114 (Part 4): 1871–1889.
Treede RD, Lankers J, Frieling A, Zangemeister WH, Kunze K, Bromm B . Cerebral potentials evoked by painful, laser stimuli in patients with syringomyelia. Brain 1991; 114 ((Part 4)): 1595–1607.
Hatem SM, Attal N, Ducreux D, Gautron M, Parker F, Plaghki L et al. Clinical, functional and structural determinants of central pain in syringomyelia. Brain 2010; 133: 3409–3422.
Wydenkeller S, Maurizio S, Dietz V, Halder P . Neuropathic pain in spinal cord injury: significance of clinical and electrophysiological measures. Eur J Neurosci 2009; 30: 91–99.
Kumru H, Soler D, Vidal J, Tormos JM, Pascual-Leone A, Valls-Sole J . Evoked potentials and quantitative thermal testing in spinal cord injury patients with chronic neuropathic pain. Clin Neurophysiol 2012; 123: 598–604.
Ulrich A, Haefeli J, Blum J, Min K, Curt A . Improved diagnosis of spinal cord disorders with contact heat evoked potentials. Neurology 2013; 80: 1393–1399.
Parizel PM, van der Zijden T, Gaudino S, Spaepen M, Voormolen MH, Venstermans C et al. Trauma of the spine and spinal cord: imaging strategies. Eur Spine J 2010; 19 (Suppl 1):S8–17.
Grant RA, Quon JL, Abbed KM . Management of acute traumatic spinal cord injury. Curr Treat Options Neurol 2015; 17: 334.
Gold M . Magnetic resonance imaging of spinal emergencies. Top Magn Reson Imag 2015; 24: 325–330.
Yoon EJ, Kim YK, Shin HI, Lee Y, Kim SE . Cortical and white matter alterations in patients with neuropathic pain after spinal cord injury. Brain Res 2013; 1540: 64–73.
Jutzeler CR, Huber E, Callaghan MF, Luechinger R, Curt A, Kramer JL et al. Association of pain and CNS structural changes after spinal cord injury. Sci Rep 2016; 6: 18534.
Landmann G, Lustenberger C, Schleinzer W, Schmelz M, Stockinger L, Rukwied R . Short lasting transient effects of a capsaicin 8% patch on nociceptor activation in humans. Eur J Pain 2016; 20: 1443–1453.
Rage M, Van Acker N, Facer P, Shenoy R, Knaapen MW, Timmers M et al. The time course of CO2 laser-evoked responses and of skin nerve fibre markers after topical capsaicin in human volunteers. Clin Neurophysiol 2010; 121: 1256–1266.
Beydoun A, Dyke DB, Morrow TJ, Casey KL . Topical capsaicin selectively attenuates heat pain and A delta fiber-mediated laser-evoked potentials. Pain 1996; 65: 189–196.
Truini A, Panuccio G, Galeotti F, Maluccio MR, Sartucci F, Avoli M et al. Laser-evoked potentials as a tool for assessing the efficacy of antinociceptive drugs. Eur J Pain 2010; 14: 222–225.
Malver LP, Brokjaer A, Staahl C, Graversen C, Andresen T, Drewes AM . Electroencephalography and analgesics. Br J Clin Pharmacol 2014; 77: 72–95.
Lorenz J, Beck H, Bromm B . Differential changes of laser evoked potentials, late auditory evoked potentials and P300 under morphine in chronic pain patients. Electroencephalogr Clin Neurophysiol 1997; 104: 514–521.
Lorenz J, Beck H, Bromm B . Cognitive performance, mood and experimental pain before and during morphine-induced analgesia in patients with chronic non-malignant pain. Pain 1997; 73: 369–375.
Simpson DM, Schifitto G, Clifford DB, Murphy TK, Durso-De Cruz E, Glue P et al. Pregabalin for painful HIV neuropathy: a randomized, double-blind, placebo-controlled trial. Neurology 2010; 74: 413–420.
Mainka T, Malewicz NM, Baron R, Enax-Krumova EK, Treede RD, Maier C . Presence of hyperalgesia predicts analgesic efficacy of topically applied capsaicin 8% in patients with peripheral neuropathic pain. Eur J Pain 2016; 20: 116–129.
Zhang Y, Ahmed S, Vo T St, Hilaire K, Houghton M, Cohen AS et al. Increased pain sensitivity in chronic pain subjects on opioid therapy: a cross-sectional study using quantitative sensory testing. Pain Med 2015; 16: 911–922.
Vollert J, Kramer M, Barroso A, Freynhagen R, Haanpaa M, Hansson P et al. Symptom profiles in the painDETECT Questionnaire in patients with peripheral neuropathic pain stratified according to sensory loss in quantitative sensory testing. Pain 2016; 157: 1810–1818.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Landmann, G., Berger, M., Stockinger, L. et al. Usefulness of laser-evoked potentials and quantitative sensory testing in the diagnosis of neuropathic spinal cord injury pain: a multiple case study. Spinal Cord 55, 575–582 (2017). https://doi.org/10.1038/sc.2016.191
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2016.191
This article is cited by
-
Variability in clinical and neurophysiological evaluation of pain development following acute spinal cord injury: a case report
Spinal Cord Series and Cases (2021)
-
Multimodal sensory evaluation of neuropathic spinal cord injury pain: an experimental study
Spinal Cord (2021)
-
Motor imagery for pain and motor function after spinal cord injury: a systematic review
Spinal Cord (2020)
-
Regional Hyperexcitability and Chronic Neuropathic Pain Following Spinal Cord Injury
Cellular and Molecular Neurobiology (2020)