Abstract
Study design:
Cross-sectional study.
Objectives:
To describe participation in activities and explore the relationship with secondary complications among persons aging with a traumatic spinal cord injury (SCI).
Setting:
A regional SCI outpatient center in Sweden.
Methods:
Data were collected through a phone survey, which included 10 activities from the instrument PARTS/M-v3 (PARTicipation Survey/Mobility version-3) together with data from the participants’ medical records. Cross-tabulation and χ2 were used for data analysis.
Results:
In this study, 121 persons matched the inclusion criteria and the final study sample comprised 73 participants (60% response rate): 55 men and 18 women. Mean age was 63.7±9.4 years, and mean time since injury was 36.3±9.2 years. Regardless of duration of SCI, all 73 participated in dressing, bathing and leisure activities. Women reported better health than men. Particularly for those who lived 36–55 years after injury; increasing pain, fatigue, spasticity and decreased muscle strength were negatively affecting participation in activities, especially exercise and active recreation. Additionally, a need to save strength/energy was also a reason for not participating in the activities. Perceived future support and concerns in relation to personal assistance, assistive devices and rehabilitation was also reported.
Conclusion:
Increasing secondary health complications and a need to save strength/energy influenced participation in activities. Laws and/or governmental policies regarding personal assistance and assistive devices did not always support participation in activities. Interventions should aim to create a balance among activities in everyday life.
Similar content being viewed by others
Introduction
A traumatic spinal cord injury (SCI) caused by, for example, a road accident or fall will change the prerequisites for participation in activities of everyday life. Participation is a multifaceted concept and can be described in different ways. Within the International Classification of Functioning, Disability and Health, participation stands for the opportunity to be involved in everyday life.1 Whereas Hammel et al.2 emphasized the need to focus on the experiences of participation, such as, for example, meaning and satisfaction. Earlier research has to a great extent focused on how participation in activities changes right after a SCI, the initial rehabilitation and the importance of re-integration in the community.3, 4, 5
As people are aging with an SCI, a wide range of secondary health complications (SHC) have been noted, for instance: fatigue and osteoporosis,6, 7 pain, and increasing muscle weakness in, for example, upper extremities.8, 9 Also, an increased risk of repeated pressure sores,10 together with additional bladder and bowel regulation problems,11, 12 cardiovascular diseases13, 14 carbohydrate intolerance, diabetes mellitus, obesity15, 16, 17 and also obstructive sleep apnea and sleep-disordered breathing.18 The majority of these SHC occur with higher frequency among those with longer SCI duration.19, 20, 21 How will these SHC effect participation among persons aging with a traumatic SCI? Rimmer et al.22 indicated that participation in activities of everyday life will decrease as a result to SHC but without giving any further explanations. Krause and colleagues have described the natural courses of SCI over a 35-year interval, showing, for example, a decreased satisfaction concerning health, social life and sex life.23, 24, 25, 26, 27, 28 Additionally, in a qualitative study of ours, we found that aging with a traumatic SCI can be seen as a complex daily struggle in order to know how to act and continue to participate in activities owing to, for example, SHC.29
To our awareness, and also recognized by Groah et al.,30, 31 a gap of knowledge remains: which activities are most exposed to changes regarding participation, and which SHC will affect participation in activities the most—knowledge that can be important for professionals within rehabilitation in order to recognize changes in participation as a result of SHC at an early stage and to be able to plan for interventions and thereby prevent additional complications. Therefore, the objective for this study was to describe participation in activities and explore the relationship with SHC among persons aging with a traumatic SCI.
Materials and methods
This cross-sectional study was conducted at Rehab Station Stockholm/Spinalis, a regional SCI outpatient center in Sweden. This center offers an individualized rehabilitation with multidisciplinary teams, both for the initial rehabilitation and the consequently follow-up visits. Primarily, it is financed by agreements/contracts with county councils, municipalities and the National Social Security Office. In addition, persons themselves can apply for rehabilitation at the outpatient center.
In Sweden, laws on a national level regulates the right for persons with a disability and thus individuals with SCI, to receive sickness compensation when not being able to work full time, assistive devices and personal assistance.
Participants
Inclusion criteria for this study were: (i) men and women with a traumatic SCI, (ii) aged ⩾50 years, (iii) neurological level C5–L2, (iv) American Spinal Injury Association (ASIA) Impairment Scale (AIS) A, B, C and D according to the AIS32 and (v) at least 20 years postinjury. A total of 121 community-dwelling persons were matching these inclusion criteria among those registered at the regional SCI outpatient center.
A letter containing information about the study and the survey were posted to 10 persons at a time. A week after the letters was posted, the first author contacted them on the phone to answer any questions and conduct the survey with those interested to participate. The procedure was repeated until all 121 persons had been contacted by letter; 18 persons declined participation in the survey, 10 could not be reached owing to, for example, inadequate contact information, 20 (13 men and 7 women) reported poor state of health as a reason to not participate in the study. In total, 73 persons completed the phone survey and thus constitute the final study sample. No compensation was offered to the participants.
Data collection
Data collection was performed between June and September 2014 and the following methods were used.
Data from medical records
Demographic information (gender and year of birth) and injury-related information (level of injury, neurological severity according to AIS and year of injury) for the 121 persons was derived from the medical records at the regional SCI outpatient center.
Survey
The survey was based on PARTS/M-v3 (PARTicipation Survey/Mobility version-3), which is a self-assessment instrument divided into two sections. The first one measures, for example, the experience of general health, the prevalence of SHC and the use of assistive devices. The second one measures participation for persons with mobility impairments in 24 activities. For each activity, four components of participation (temporal, evaluative, health-related and supportive) are measured. Temporal questions focus on frequency of, and time spent participating in, each activity. Evaluative questions focus on choice, control, satisfaction and importance of participating in a particular activity. Health-related questions focus if an activity is limited by pain and/or fatigue. Supportive questions focus on personal and/or assistive devices is needed to participate. The original version has been tested as a reliable measure with good internal consistency and stability.33
For this study, 10 activities (Table 1) were selected from PARTS/M-v3 to the survey, a decision based on the findings in an earlier study of ours.29
PARTS/M-v3 was translated to Swedish and a few modifications of the original version were carried out in order to answer the objective. One question was added in relation to the temporal questions for each activity in order to find out the underlying cause if not participating in the activity. The question about prevalence of SHC (spasticity, respiratory diseases, cardiovascular diseases, urinary tract infection, bladder and/or bowel incontinence, pressure sore and/or depression) from the first section was condensed and added to each activity in relation to the health-related questions. For the activity ‘Leave home’, a question was added to the supportive questions regarding commonly used transport means. At the end of the survey, the participants were asked an open-ended question about their perceived support in order to continue to participate in the activities. The translation and modifications were all carried out by the first author (UL) in cooperation with the fourth author (DG), one of the developers of the instrument. Continuous discussions were held in the research group before a final version of the survey was completed.
The first author administered the survey by phone and entered the responses of the participants directly in an electronic spreadsheet. The average for the phone survey with each participant was 40 min.
Field notes
Comments and/or clarifying information from the participants were documented in relation to each question.
Data analysis and statistics
To answer the objective for study, the research group decided to analyze two of the temporal questions (if participating and if not, the reason why), the supportive and the health-related questions.
Data from medical records and survey
Data analyses were conducted using the IBM Statistical Package for Social Sciences (SPSS, IBM Corp, Armonk, NY, USA) statistics, version 22.0. Descriptive statistical analyses, for example, mean, s.d. and frequencies, were performed to explore the study population and the data. Cross-tabulation and X2 were used to examine the relationships between demographic variables, level of injury, neurological severity according to AIS and time since injury and the selected questions in relation to the 10 activities used in the survey. A P-value of<0.05 was required for statistical significance.34
Owing to the limited data set, the grouping proposed by DeVivo et al.35 was not possible to use. Instead the following groupings were made for the data analysis. Age was dichotomized based on the retirement age in Sweden: age group 1 included persons aged between 50 and 65 years, and age group 2 included those aged between 66 and 87 years. Time since injury was dichotomized to retain two comparable groups regarding size: 20–35 and 36–55 years. Level and severity of injury was divided into four groups to retain comparable groups regarding size: group 1, included C5–C8; group 2, Th1–Th6; group 3, Th7–Th12; and group 4, L1–L2, including AIS A, B, C and D within each group.
Data from the open-ended question and field notes
Answers from the closing open-ended question in the survey together with any comments from the participants were identified and compiled in relation to each question and used to expand the understanding of the data in the results.
Statement of ethics
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research. The study was approved by the Human Ethics committee in Stockholm, Sweden (no.: 2014/214-31/3).
Results
Participation and drop out analysis
Descriptive characteristics of the total (n=121) and study population (n=73) together with the nonparticipants (n=48) can be seen in Table 2, showing that demographics, injury level and severity in the study population are representative for the total population. Education level and marital status is presented for the study population. There were no significant differences between the participants and the nonparticipants.
In Table 3, data on the level and severity of injury among the 73 participants in the study are presented.
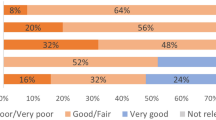
General health in the study population
The participants (n=73) rated their general health on a scale from 1 to 5, with higher scores indicating better health (a question in PARTS/M-v3). Overall, women reported better health than men. Among the 34 participants who scored their health as poor or fair, 32 were men (P=0.05).
The use of assistive devices and transport means
The use of assistive devices indoors and outdoors in relation to time since injury can be seen in Figure 1.
The use of assistive devices indoors and outdoors. *Other—indoor refer to walking without assistive device but with support from, for example, furniture. Other—outdoor refer to, for example, support from a person or adaptive hand bikes, which can be installed to manual wheelchairs. ‡Time since injury: TSI 1=20–35 years; TSI 2=36–55 years. Percentage of what assistive devices participants most frequently use when moving indoors and outdoors in relation to time since injury. A full color version of this figure is available at the Spinal Cord journal online.
No statistically significant relations were found between the use of assistive devices and age or time since injury. However, worth mentioning is that the participants in the group 36–55 years after injury were always using assistive devices for mobility. In addition, they used powered wheelchairs to a greater extent compared with the participants in the group 20–35 years after injury. Not surprisingly, statistically significant relations were found between assistive devices and severity of injury, AIS grade A–C were related to the use of manual wheelchairs indoors (P=0.001) and AIS A and B for using manual wheelchair outdoors (P=0.001). When participating in activities out in the community, the participants used their assistive devices in combination with the following transport means: 45 adapted car/van, 15 mobility service, and 9 public transportation.
Participation in activities
As shown in Figure 2, all the 73 participated in dressing, bathing and leisure activities. Approximately 70% were participating in dressing and bathing independently, and they were evenly distributed between the group 20–35 and 36–55 years after injury. Among the remaining 30% who participated in these activities with the help from personal assistants, approximately two-thirds were in the group 36–55 years after injury. When it comes to leisure activities, 94% of the participants were independent. Likewise, 91% were participating in social activities independently. Participation in exercise and active recreation was lower in both groups and especially in the group 36–55 years after injury. In addition, there were just a few who participated in exercise (n=6) and active recreation (n=2) with personal assistance. Among the 25 having an employment, no one had personal assistance at their work. There were no statistically significant relations between participation in activities and age or time since injury.
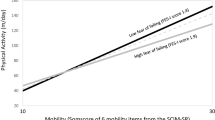
Participation and SHC
Participants reported if pain, fatigue and other SHC influenced their participation for each activity, and the results are shown in Figure 3. Participants in the group 36–55 years after injury reported how especially fatigue and other SHC (for example, decreasing muscle strength, increasing spasticity, pressure sore and prolonged time for bowel care) negatively influenced their participation in activities (P=0.03). Sixty-eight percent of the participants in the group 20–35 years after injury reported pain when participating in active recreation (P=0.02) in comparison with participants in the group 36–55 years after injury.
Overall, 42.2% of the participants specified SHC such as pain, fatigue, spasticity and decreased muscle strength primarily as reasons for no longer participating in active recreation while 31.1% reported that they needed their strength/energy for other activities. In addition, 67.7% reported that the same SHC as above was the reason for no longer exercising and 22.6% reported that they needed their strength/energy for other activities.
Perceived future support to continue participation in activities
Data from the open-ended question and field notes showed that within a period of 5 years, approximately 50% of all the participants expected an increased need for help to participate in activities, such as bathing, dressing and working inside their homes. The majority of them expressed their concerns about what would happen if these needs appeared after they turned 65 years, since then laws and/or governmental policies makes it impossible to expand personal assistance in Sweden. A number of participants had their applications for personal assistance rejected even though they were aged <65 years and they questioned what the future would be like when their needs for help further increased. The participants also expected a need to change or start to use new assistive devices in relation to indoor and outdoor mobility. In addition, they were frustrated about the bureaucracy they experienced regarding getting a prescribed assistive device.
Participants expressed the need for regular follow-ups together with a multi-professional rehabilitation team and not just a physician together with a nurse. They thought that these appointments could be improved in several ways to prepare them for changes in relation to SHC and, in turn, prevent difficulties to participate in activities. Many of the participants in the group 36–55 years after injury also experienced an increased need for non-routine visits to physicians. They had already experienced a poor knowledge about SCI among health-care professionals in general and the combination of aging with a SCI made it even more complicated. This experience made them wish for better education in the area among health-care professionals in general.
Discussion
The results in this study describe participation in activities and how pain, fatigue and other SHC negatively influenced participation in activities among persons aging with a traumatic SCI. Further, our findings describe the participants’ perceived support in order to continue to participate in activities. These findings should be viewed in relation to that, for example, age and time since injury of our study population is similar to the ones in other studies.27, 36 Still it is important to remember that, even though individuals now are successfully surviving to their 70s and 80s, life expectancy is directly related to severity and completeness of the injury.30, 31 No ventilator-dependent individuals participated in this study owing to the inclusion criteria, and around 20 among those matching the inclusion criteria denied participation because of a poor state of health. Thus there is a chance that those who participated in the study had more favorable characteristics and were better adapted to longer survival.
All the participants were participating in leisure activities and the majority were also socializing, activities that earlier has been described as important among persons with SCI.37, 38 Krause and Bozard27 identified in their 35-year longitudinal study that social participation decreased over time, which is in contrast to our findings that showed no relations between socializing and time since injury. However, this comparison should be considered in relation to the different study designs that were used.
Earlier research has identified that independence in activities of daily living such as dressing and bathing declines with every decade after injury.12, 39 This is in line with our findings as the participants in the group 36–55 years after injury needed more help with dressing and bathing than the group with participants 20–35 years after injury.
Our results show that the participants who lived with an SCI for 36–55 years did not participate in exercise and active recreation as their physical functions are decreasing. Interestingly, participating in these activities independently appear to be important as our findings indicate that the participants rather choose to resign from participating in these activities than accepting help. The SHC (for example, pain, fatigue, spasticity and decreased muscle strength), which the participants reported as reasons for not participating in exercise and active recreation, have been described in earlier research.19, 20, 40 Earlier findings by Rimmer et al.22 suggest that exercise can prevent or reduce, for example, shoulder pain, whereas others have described how physical activity improves health and well-being41, 42 and can prevent SHC-like cardiovascular diseases43 among persons with SCI. On the other hand, our results also show that the increasing needs to save strength/energy to prioritize participation in other activities was a common reason for not participating in exercise and active recreation.
Knowing the benefits of physical activity in relation to our findings, how can we promote persons aging with an SCI to continue to exercise and participate in active recreation? We suggest the following implications for rehabilitation: the need for screening their everyday life in order to be able to create/re-establish a balance among their activities. This emphasizes the importance of these persons to have regular meetings with multi-professional teams, something that also is in line with recent research from Molton et al.44 In addition, we suggest that all the team members should have a proactive approach in their work and also educate persons to be attentive to changes of participation in activities at an early stage.
Remarkably, even if SHC negatively influenced participation in activities especially among those who lived with the SCI between 36 and 55 years, the majority of the participants still rated their general health as good. The fact that women reported better general health than men is worth mentioning since a greater proportion of women in the general population rate their health less positive.45, 46 In comparison to the SCI population, where no significant differences in general health between genders were found.47
The participants’ concerns about getting personal assistance approved or increased owing to laws and/or governmental policies, together with the bureaucracy regarding assistive devices, is in line with earlier research29, 48 and can create an injustice.49 This means that persons aging with an SCI are not given the same rights to participate in activities based on their own terms and desires.
The findings from this study should be interpreted based on the following methodological considerations. Using a phone survey proved to be effective in gathering data, all surveys were completed and the participants gave detailed answers. As a basis for our survey, 10 activities from PARTS/M-v3 were used and thus cover the majority of the activities suggested by International Spinal Cord Society50 in their data set for activity and participation.51 One advantage with PARTS/M-v3 is the multidimensional picture that it gives of participation. However, this study also has its limitations; owing to the cross-sectional design and the limited data set, it is not possible to explain if the observed differences is caused by, for example, duration of injury, severity of SCI and/or current chronological age. In addition, another effect of the limited data set can be the difficulty in establishing significant relations between variables. Therefore, generalization of our findings may be limited. At the same time, the present study is exploratory in nature, and our findings can serve as a base for designing further research.
To conclude, the present study show how pain, fatigue and other SHC were negatively influencing participation in activities. Women reported better health than men. Additionally, persons who lived with their SCI between 35 and 55 years were more likely to not participate in exercise and active recreation owing to decreased physical function and increased need for strength/energy for other activities. The participants described perceived future support and also frustration/concerns regarding, for example, personal assistance, assistive devices and rehabilitation.
For the future, it would be of interest to re-evaluating a purposeful sampled group from the sample in this study, every 5 years, using a time-sequential design52 by adding a longitudinal component to cross-sectional studies and also comparing our findings with data collected with PARTS/M-v3 internationally. Further research in this area is needed to describe what kind of support persons aging with an SCI needs to continue participation in activities, such as exercise and active recreation.
Data archiving
There were no data to deposit.
References
World Health Organization [WHO] Toward a Common Language for Functioning, Disability and Health: ICF, the International Classification of Functioning, Disability and Health. World Health Organization: Geneva, Switzerland. 2002.
Hammel J, Magasi S, Heinemann A, Whiteneck G, Bogner J, Rodriguez E . What does participation mean? An insider perspective from people with disabilities. Disabil Rehabil 2008; 30: 1445–1460.
Schönherr M, Groothoff J, Mulder G, Eisma W . Participation and satisfaction after spinal cord injury: results of a vocational and leisure outcome study. Spinal Cord 2004; 43: 241–248.
Angel S, Kirkevold M, Pedersen BD . Getting on with life following a spinal cord injury: regaining meaning through six phases. Int J Qual Stud Health Well-being 2009; 4: 39–50.
Whiteneck G, Gassaway J, Dijkers M, Backus D, Charlifue S, Chen D et al. Inpatient treatment time across disciplines in spinal cord injury rehabilitation. J Spinal Cord Med 2011; 34: 133–148.
Cook KF, Molton IR, Jensen MP . Fatigue and aging with a disability. Arch Phys Med Rehabil 2011; 92: 1126–1133.
Garland DE, Adkins RH, Rah A, Stewart CA . Bone loss with aging and the impact of SCI. Top Spinal Cord Inj Rehabil 2001; 6: 47–60.
Brose SW, Boninger ML, Fullerton B, McCann T, Collinger JL, Impink DB et al. Shoulder ultrasound abnormalities, physical examination findings, and pain in manual wheelchair users with spinal cord injury. Arch Phys Med Rehabil 2008; 89: 2086–2093.
Waters RL, Sie IH . Upper extremity changes with SCI contrasted to common aging in the musculoskeletal system. Top Spinal Cord Inj Rehabil 2001; 6: 61–68.
Hitzig SL, Tonack M, Campbell KA, McGillivray CF, Boschen KA, Richards K et al. Secondary health complications in an aging Canadian spinal cord injury sample. Am J Phys Med Rehabil 2008; 87: 545–555.
Faaborg PM, Christensen P, Finnerup N, Laurberg S, Krogh K . The pattern of colorectal dysfunction changes with time since spinal cord injury. Spinal Cord 2008; 46: 234–238.
Liem N, McColl M, King W, Smith K . Aging with a spinal cord injury: factors associated with the need for more help with activities of daily living. Arch Phys Med Rehabil 2004; 85: 1567–1577.
Myers J, Lee M, Kiratli J . Cardiovascular disease in spinal cord injury: an overview of prevalence, risk, evaluation, and management. Am J Phys Med Rehabil 2007; 86: 142–152.
Wahman K, Nash MS, Lewis JE, Seiger Å, Levi R . Increased cardiovascular disease risk in Swedish persons with paraplegia: the Stockholm Spinal Cord Injury Study. J Rehabil Med 2010; 42: 489–492.
Bauman W, Spungen A . Carbohydrate and lipid metabolism in chronic spinal cord injury. J Spinal Cord Med 2001; 24: 266–277.
Lavela SL, Weaver FM, Goldstein B, Chen K, Miskevics C, Rajan S et al. Diabetes mellitus in individuals with spinal cord injury or disorder. J Spinal Cord Med 2006; 29: 387–395.
Rajan S, McNeely MJ, Hammond M, Goldstein B, Weaver F . Association between obesity and diabetes mellitus in veterans with spinal cord injuries and disorders. Am J Phys Med Rehabil 2010; 89: 353–361.
Biering-Sørensen F, Jennum P, Laub M . Sleep disordered breathing following spinal cord injury. Respir Physiol Neurobiol 2009; 169: 165–170.
Capoor J, Stein AB . Aging with spinal cord injury. Phys Med Rehabil Clin N Am 2005; 16: 129–161.
Jensen M, Truitt A, Schomer K, Yorkston K, Baylor C, Molton I . Frequency and age effects of secondary health conditions in individuals with spinal cord injury: a scoping review. Spinal Cord 2013; 51: 882–892.
Savic G, Charlifue S, Glass C, Soni BM, Gerhart KA, Ali Jamous M . British ageing with SCI study: changes in physical and psychosocial outcomes over time. Top Spinal Cord Inj Rehabil 2010; 15: 41–53.
Rimmer JH, Chen MD, Hsieh K . A conceptual model for identifying, preventing, and managing secondary conditions in people with disabilities. Phys Ther 2011; 91: 1728–1739.
Krause J, Broderick L . A 25-year longitudinal study of the natural course of aging after spinal cord injury. Spinal Cord 2005; 43: 349–356.
Krause J, Coker J . Aging after spinal cord injury: a 30-year longitudinal study. J Spinal Cord Med 2006; 29: 371–376.
Crewe N, Krause J . An eleven-year follow-up of adjustment to spinal cord injury. Rehabil Psychol 1990; 35: 205–210.
Krause JS . Longitudinal changes in adjustment after spinal cord injury: a 15-year study. Arch Phys Med Rehabil 1990; 73: 564–568.
Krause J, Bozard J . Natural course of life changes after spinal cord injury: a 35-year longitudinal study. Spinal Cord 2012; 50: 227–231.
Krause JS . Changes in adjustment after spinal cord injury: a 20-year longitudinal study. Rehabil Psychol 1998; 43: 41–45.
Lundström U, Lilja M, Gray DB, Isaksson G . Experiences of participation in everyday occupations among persons aging with a tetraplegia. Disabil Rehabil 2015; 37: 951–957.
Groah SL, Charlifue S, Tate D, Jensen MP, Molton IR, Forchheimer M et al. Spinal cord injury and aging: challenges and recommendations for future research. Am J Phys Med Rehabil 2012; 91: 80–93.
Groah S, Kehn M . The state of aging and public health for people with spinal cord injury: lost in transition? Top Spinal Cord Inj Rehabil 2010; 15: 1–10.
Kirshblum SC, Burns SP, Biering-Sorensen F, Donovan W, Graves DE, Jha A et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med 2011; 34: 535–546.
Gray DB, Hollingsworth HH, Stark SL, Morgan KA . Participation survey/mobility: psychometric properties of a measure of participation for people with mobility impairments and limitations. Arch Phys Med Rehabil 2006; 87: 189–197.
Dawson B, Trapp RG . Basic & Clinical Biostatistics, 4th edn, Lange Medical Books/McGraw-Hill: New York, USA. 2004.
DeVivo M, Biering-Sørensen F, New P, Chen Y . Standardization of data analysis and reporting of results from the international spinal cord injury core data set. Spinal Cord 2011; 49: 596–599.
Jörgensen S, Iwarsson S, Norin L, Lexell J . The Swedish Aging With Spinal Cord Injury Study (SASCIS): methodology and initial results. PM R 2016; 8: 667–677.
Lundström U, Lilja M, Petersson I, Lexell J, Isaksson G . Leisure repertoire among persons with a spinal cord injury: Interests, performance, and well-being. J Spinal Cord Med 2013; 37: 186–192.
Carpenter C, Forwell SJ, Jongbloed LE, Backman CL . Community participation after spinal cord injury. Arch Phys Med Rehabil 2007; 88: 427–433.
Charlifue SW, Weitzenkamp DA, Whiteneck GG . Longitudinal outcomes in spinal cord injury: aging, secondary conditions, and well-being. Arch Phys Med Rehabil 1999; 80: 1429–1434.
Thompson L . Functional changes in persons aging with spinal cord injury. Assist Technol 1999; 11: 123–129.
Ginis KM, Jetha A, Mack D, Hetz S . Physical activity and subjective well-being among people with spinal cord injury: a meta-analysis. Spinal Cord 2010; 48: 65–72.
Hicks A, Ginis KM, Pelletier C, Ditor D, Foulon B, Wolfe D . The effects of exercise training on physical capacity, strength, body composition and functional performance among adults with spinal cord injury: a systematic review. Spinal Cord 2011; 49: 1103–1127.
Buchholz AC, Martin Ginis KA, Bray SR, Craven CB, Hicks AL, Hayes KC et al. Greater daily leisure time physical activity is associated with lower chronic disease risk in adults with spinal cord injury. Appl Physiol Nutr Metab 2009; 34: 640–647.
Molton IR, Terrill AL, Smith AE, Yorkston KM, Alschelur KN, Ehde DM et al. Modeling secondary health conditions in adults aging with physical disability. J Aging Health 2014; 26: 335–359.
Moore E, Rosenberg M, Fitzgibbon S . Activity limitation and chronic conditions in Canada's elderly, 1986 2011. Disabil Rehabil 1999; 21: 196–210.
Statistics Sweden [SCB]. Living conditions surveys (ULF/SILC). General health, year 2012-2013. http://www.scb.se/sv_/Hitta-statistik/Statistik-efter-amne/Levnadsforhallanden/Levnadsforhallanden/Undersokningarna-av-levnadsforhallanden-ULFSILC/#c_li_354235 Updated 2015. Accessed 31 August 2015.
McColl M, Charlifue S, Glass C, Lawson N, Savic G . Aging, gender, and spinal cord injury. Arch Phys Med Rehabil 2004; 85: 363–367.
Whiteneck G, Meade MA, Dijkers M, Tate DG, Bushnik T, Forchheimer MB . Environmental factors and their role in participation and life satisfaction after spinal cord injury. Arch Phys Med Rehabil 2004; 85: 1793–1803.
Whiteford G In: Christiansen C, Townsend E (eds). An Introduction to Occupation: The Art and Science of Living, 2nd edn, Prentice Hall: Upple Saddle River, NJ, USA. 2010, pp 303–328.
International Spinal Cord Society. International SCI activity and particpation data set http://www.iscos.org.uk/international-sci-activity-and-participation-data-sets. Updated 2015. Accessed 31 January 2015.
Biering-Sørensen F, Charlifue S, DeVivo M, Noonan V, Post M, Stripling T et al. International spinal cord injury data sets. Spinal Cord 2006; 44: 530–534.
Adkins RH . Research issues in aging studies associated with SCI. Top Spinal Cord Inj Rehabil 2001; 6: 128–135.
Acknowledgements
We thank the participants who answered the survey in this study and for the assistance with practical tasks from the staff at the regional SCI outpatient center.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Lundström, U., Wahman, K., Seiger, Å. et al. Participation in activities and secondary health complications among persons aging with traumatic spinal cord injury. Spinal Cord 55, 367–372 (2017). https://doi.org/10.1038/sc.2016.153
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2016.153
This article is cited by
-
Experienced sitting-related problems and association with personal, lesion and wheelchair characteristics in persons with long-standing paraplegia and tetraplegia
Spinal Cord (2019)
-
Participation restriction and assistance needs in people with spinal cord injuries of more than 40 year duration
Spinal Cord Series and Cases (2018)
-
Neuropathic pain and spasticity: intricate consequences of spinal cord injury
Spinal Cord (2017)