Abstract
Study design:
Prospective parallel waitlist randomised controlled trial.
Objectives:
Evaluate the feasibility and effectiveness of an Internet-based psychological intervention treating comorbid mood disorder in adults with spinal cord injury (SCI). Improved mood and satisfaction with life were primary outcomes.
Setting:
Victoria, Australia.
Intervention:
Electronic Personal Administration of Cognitive Therapy (ePACT).
Measures:
Depression, Anxiety and Stress Scale–Short Form (DASS21), Personal Well-being Index, Helplessness subscale of the Spinal Cord Lesion Emotional Well-being Scale v1 Australia, at each time point.
Participant qualifying criteria:
Adults (18–70 years), chronic SCI, attend SCI review clinic at Austin or Caulfield Hospital and score above normative threshold of the Depression, Anxiety and Stress Scale–Short Form (DASS21).
Methods:
Forty-eight participants completed Time 2 post intervention (n=23) or time equivalent for waitlist control group (n=25) telephone interviews. The measures were repeated a third time (Time 3) for a small subgroup (n=12) at 6 months post intervention within the study implementation time frame.
Results:
Univariate within group analyses revealed significant improvement in mood in the intervention group at Time 2: (lower depression (effect size (ES)=0.4), anxiety (ES=0.4) and stress (ES=0.3)) and higher satisfaction with life (ES=0.2). Waitlist control group improved in depression only (ES=0.3) by Time 2. Multilevel variance components analyses, although not as positive, were still encouraging. Improvement in mood symptoms was maintained in the small group reinterviewed at Time 3.
Conclusion:
Although Internet-based interventions for mental health issues in SCI not a solution for all, our results indicate that they are a potentially valuable addition to the currently available options.
Similar content being viewed by others
Introduction
Individuals with chronic spinal cord injury (SCI) of any cause, both traumatic and non-traumatic, are highly vulnerable to mental health problems, particularly depression, anxiety and stress, which can further compromise their quality of life and adversely affect their relationships and community participation.1, 2, 3, 4 Unfortunately, poor uptake of mental health services among those with chronic SCI is well documented.1, 3 Social withdrawal consequent to mental health problems is likely exacerbated by limited services and finances, mobility and travel challenges and demands of daily living, making it difficult to easily attend specialist health providers for help with these difficulties.5
The availability of novel forms of treatment and mental health promotion that are accessible, acceptable and sympathetic to the special needs of people with SCI is needed.5, 6 There is growing evidence for the efficacy of Internet-based interventions targeting depression and/or anxiety in the general population with early meta-analyses showing good potential,7, 8, 9 particularly with therapist support.9
In response to the perceived need for alternative methods of delivering mental health support and interventions, an Electronic Personal Administration of Cognitive Therapy (ePACT) programme was recently developed and successfully trialled on three adults with chronic SCI, confirming the acceptability and potential of the therapy.10
The aim of this project was to conduct a randomised control trial (RCT) of ePACT for people with SCI and comorbid mood disturbance to evaluate the feasibility of this mode of therapy and effectiveness on a larger group of individuals.
Materials and methods
Design, setting and participants
The inclusion criteria for participants in this study were adults aged between 18 and 70 years, with a chronic SCI (⩾ 6 months post injury of any cause (traumatic and non-traumatic SCI), living in the community and scored above the normative threshold of the screening tool, the Depression, Anxiety and Stress Scale–Short Form (DASS21), which is described below. Participants comprised a subgroup of a large sample, the recruitment of which is described more fully in a report on screening for mental health issues in people with chronic SCI.11 In summary, participants were sourced from the two dedicated SCI rehabilitation units in Victoria, the Caulfield Hospital (part of Alfred Health) and the Austin Hospital (part of Austin Health), over a 15-month period in 2012–2013. Any screened adult with SCI who scored above the DASS21 normative threshold and so deemed would benefit from psychological support could choose from a range of options that included, in part, referral to their general practitioner, referral to a psychologist, linking with disability support services or trying the Internet-based programme ePACT.
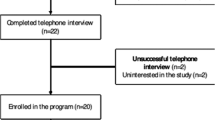
The design of the study was a prospective parallel waitlist RCT. Improved mood and satisfaction with life were the primary outcomes. Computerised random ordering was achieved through http://www.random.org. The study began with 1:1 random allocation in blocks of 10 by Migliorini. However, as the study progressed there emerged a systematic pattern to those who dropped out of the study—each had been allocated to the Intervention group, none allocated to the Waitlist control group. To achieve a more balanced final sample, ~9 months or 60% into the recruitment period, the randomisation methodology was adapted to be weighted in favour of the intervention group 3:2 in blocks of 10. Allocation was concealed from participants until the time 1 interview was completed. The interviewer (Migliorini) extracted the next allocation from the random-allocation list at the end of the time 1 interview. See Figure 1 for details.
Intervention: ePACT
ePACT is a 10-module skills and psycho-educational programme that is largely based on cognitive behaviour therapy principles but with the addition of a positive psychology (session 8) and mindfulness meditation aspects (session 9), as follows.
-
Introduction and welcome
-
Session 1: Starting out
-
Session 2: Altered thinking
-
Session 3: Changing unhelpful behaviour
-
Session 4: Practical problem solving
-
Session 5: Building resiliency/feeling physical
-
Session 6: Scheduling pleasant events
-
Session 7: Setting goals
-
Session 8: Positive events/building resiliency
-
Session 9: Relaxation
It can be used as a self-help programme on its own; however, it is recommended to also have clinician support by phone and/or email. Individuals undertake (roughly) one module per week and complete between module activities. Each module includes links to further information that the reader can follow. Although modules were sequentially numbered, there was no obligation to follow the sequence. Some modules can be completed in as little as 10 min, whereas others could take up to 1 h. The homework tasks required some effort to be made on most if not every day between modules.10
Outcome measures
All measures were taken at enrolment into the RCT pre-randomisation, at 10–12 weeks post intervention (or time equivalent for waitlist control participants), and for a small subset at 6 months post intervention within the study implementation time frame. All measures have previously demonstrated good reliability and validity.
The Depression, Anxiety and Stress Scale short version (DASS21)12 is a reliable, valid, self-report measure of depression, anxiety and stress previously used with general population groups, clinical population groups and population groups with physical disabilities. Respondents are asked how much each of the 21-items had applied to them over the previous week. The rating scale comprise the following: 0=did not apply to me at all; 1=applied to me to some degree or some of the time; 2=applied to me to a considerable degree or a good part of the time; 3=applied to me very much or most of the time. Scores of the subscales are summed and then doubled to convert to equivalent full 42-item DASS scores for severity categorisation. Severity ratings comprise normal, mild, moderate, severe and extremely severe. At Time 1 screening/enrolment, the Cronbach alpha coefficient for the overall DASS21 scale was α=0.95; alpha coefficients for the subscale domain depression were α=0.93, for anxiety were α=0.81 and for stress were α=0.90. The terms depression, anxiety and stress will be used to indicate that the individuals with SCI have a score on the relevant scale that was above the published clinical cutoff. These terms are not synonymous with a clinical diagnosis but do indicate a high probability of such a diagnosis.
The Personal Well-being Index–Adult13 is a self-report questionnaire measuring satisfaction across eight quality of life domains: standard of living, health, achieving in life, relationships, safety, community connectedness, future security and spirituality/religion. A 0–10 rating scale is used where 0 represents completely dissatisfied, 10 represents completely satisfied and 5 is neutral. Overall satisfaction with life is the mean average of the eight domains. At Time 1 enrolment, the Cronbach alpha coefficient for the overall Personal Well-being Index scale was α=0.85.
The Spinal Cord Lesion Emotional Well-being Questionnaire version 1 Australia (SCL EWL v1 Australia)14 is a 12-item self-report measure that assesses individuals with SCI their current well-being across the three domains of helplessness, intrusion and personal growth. This study focused on helplessness only as it was the only independent variable to correlate to both positive and negative outcomes previously.14 The domain helplessness reflects perplexity, lack of control and loss of self-esteem. Respondents select from 1=strongly disagree, 2=disagree, 3=agree or 4=strongly agree. The score for the domain is the overall mean of the items within the domain and can range from one to four. Higher scores represent higher affirmation of the domain. At Time 1 enrolment, the Cronbach alpha coefficient for the subscale domain helplessness was α=0.78.
Power analysis
Currently available cross-sectional data indicate sizeable differences in mean depression, anxiety and stress scores between those identified as having emotional disorder and those not so identified. These give an order-of-magnitude indication of ‘best possible’ results. The present study design with treated and control groups of size 50 per group has power above 0.9 to detect modest proportions of the ‘best possible’ improvements, for example, change of 4 of a possible 14 DASS depression score points or 3 of a possible 8 DASS anxiety points.
Analyses
Initial descriptive analyses were performed. Comparative analyses (t-tests and chi-square) were conducted to test for potential differences between individuals who dropped out and those who remained in the study and between the Intervention and Waitlist Control groups at Time 1. Paired-samples t-tests were conducted to examine the differences between Time 1 and Time 2 for the Intervention group and the same for the Waitlist Control group. Effect size using Eta squared (η2) was calculated and interpreted according to the Cohen’s guidelines,15 whereby 0.01 is considered as a mall effect size, 0.06 is considered a moderate effect size and 0.14 is considered as a large effect size.
The overall study design is a longitudinal study with individuals divided into two groups that create a natural nesting model. Multilevel models, otherwise known as hierarchical linear models, nested models or random-coefficient models, are a particularly appropriate multivariate way of analysing longitudinal within-person data that adjusts for both within and between-subject variances.16, 17
For the multilevel analyses, marital status was dichotomised into the independent variable relationship with 0=single, widowed, divorced or separated and 1= married, defacto or partner relationship. All participants who were randomly allocated to a group and had a complete data set at Time 1 were included in the multivariate analyses, therefore conforming to the principle of intention to treat.
IBM SPSS v21 and STATA v10 were used for the analyses. P-values less than.05 were deemed statistically significant.
All applicable institutional and governmental regulations concerning the ethical use of human subjects were followed during the course of this research. Monash University Human Ethics Committee, Austin Health Human Ethics Committee and Alfred Health Human Ethics Committee approved the research project. The RCT was registered at A&NZ Clinical Trial Registry (ACTRN 12612000587808).
Results
Screening
Details of the screening process and screening results have been recently published and are described more fully elsewhere.11 In total, 573 adults with chronic SCI aged 70 years or less were screened. Just over half of those screened scored within the DASS21 normative range; however, 263 individuals (46%) reported symptoms that indicated the likely presence of some level of mood disturbance, hence fulfilling the programme participation criteria. Just over half who did meet the criteria were willing to receive psychological support (n=135, 51.3%) including 25% of this subgroup of individuals who were already seeing a mental health professional. See Figure 1 for details.
Time 1: Enrolment in intervention programme
In total, 71 individuals (27% of those who reported clinically significant symptomology) accepted the option of trying the ePACT programme. These individuals did not differ from those who declined in anxiety (P=0.42) or stress (P=0.76); however, they tended to be more depressed (opted for ePACT M (s.d.)=20.0 (10.7), declined ePACT M (s.d.)=16.9 (9.9), t=2.2 (df, 261) P=0.03). Twelve individuals failed to complete the intake process. Several explanations were given including computer breakdown, medical emergency, requiring admission to hospital and complicated family life. Those who failed to complete the intake process did not differ in depression (P=0.32) or anxiety (P=0.29) scores. The difference in scores for stress bordered on significance with those not completing the intake interview tending to be more stressed (completed intake M (s.d.)=17.1 (9.2) and not completed intake M (s.d.)=22.8 (8.7), t=−2.0 (df, 69), P=0.05).
The remaining 59 adults who met the criteria and completed the intake process were randomly allocated into either the intervention group or the waitlist control group. There were no significant differences between groups in depression (P=0.85), anxiety (P=0.11), stress (P=0.10), helplessness (P=0.57) or overall satisfaction with Life (P=0.19). There were no significant differences between groups according to gender (P=0.86) or age (P=0.12); however, there were significant differences according to time since injury (TSI; P=0.02) and the level of injury distribution. See Table 1 for details.
Progress through the Intervention programme
During the progress of the study, 11 individuals (19%) discontinued their participation in the study; all had been allocated to the Intervention group. Several explanations were given including overestimating their computer skills, could not cope with the time required because of substantial medical commitments, had old hardware that broke down and no funds for repairs, were living in chaos (including domestic violence) and some thought the programme was not for them after all. Intervention group participants who dropped out of the programme did not differ significantly from those who stayed in the programme according to depression (P=0.35), anxiety (P=0.81), stress (P=0.95), satisfaction with life (P=0.58), helplessness (P=0.77) age (P=0.91), TSI (P=0.17) or gender (P=0.63).
Time 2: Post-intervention or time equivalence preliminary analyses
Paired-samples t-tests were conducted to examine the impact of the intervention for Group A intervention participants and the equivalent in time to Group B waitlist control participants. Depression only improved with the passage of time for Group B waitlist control group (depression η2=0.25). In contrast, depression, anxiety and stress reduced significantly, and satisfaction with life improved concurrently in Group A intervention group with a large effect size to each (depression η2=0.37; anxiety η2=0.43; stress η2=0.28; satisfaction η2=0.24). See Table 2 for details.
Random effects (multilevel-variance components models)
All participants were randomly allocated to a group, except three people who had missing values in either age or being in a relationship status variables.
Outcome satisfaction with life
Overall satisfaction with life improved by 1.0 point more in the intervention group, which was a statistically significant improvement (P=0.01). In contrast, satisfaction with life dropped 0.4 points over time in the waitlist control group, albeit by a statistically nonsignificant amount (P=0.09). In the model, satisfaction with life was not associated with age, gender, TSI or being in a relationship. See Table 3 for details.
Outcome depression
By Time 2, depression reduced significantly for everyone: in the waitlist control group by 4.0 points and in the intervention group by 6.7 points. By Time 2, depression reduced on average 2.7 points more in the intervention group; however, the size of the reduction in the intervention group compared with the waitlist control group was nonsignificant at the 5% level. In the model, depression was not associated with age, gender or TSI. See Table 3 for details.
Outcome anxiety
Symptoms of anxiety reduced by 3.3 points more in the intervention group and approached statistical significance with the probability sitting at the 6% level. In the model, anxiety was not associated with age, TSI or whether in a relationship or simply the passage of time. See Table 3 for details.
Outcome stress
Although there tended to be a small reduction in stress over time, no independent variable was associated with stress in the model. See Table 3 for details.
Outcome helplessness
TSI was significantly associated with helplessness. Helplessness was lower in those injured earlier, reducing by 0.01 points per year. In the model, helplessness was not associated with age, gender, being in a relationship, the intervention or simply the passage of time. See Table 3 for details.
Time 3: 6 Months post intervention
The third interview of 6 months post intervention was conducted with 12 participants. Because of this small sample size and the non-normal distribution of scores (particularly common in social sciences), nonparametric Friedman tests were conducted.
Investigation of the small subgroup of Group A intervention participants who were eligible for the Time 3 (6 months post intervention) interview found that, on the whole, depression, anxiety and stress decreased substantially by the Time 2 post-intervention time point. This not only was maintained for 6 months but there was also a further, albeit small decrease. This was not found in the satisfaction with life scores. See Table 4 for details.
Discussion
Mental health and quality of life improvements were deemed evidence of programme effectiveness. According to these standards, ePACT was relatively successful. Analyses suggest that Individuals who progressed through the programme experienced significantly reduced mood disturbance and improved satisfaction with life. Moreover, the reduction in mood disturbance was maintained for 6 months post intervention, albeit in the limited number of participants who were reviewed at that third time point.
More sophisticated analyses, although not as positive, were still encouraging. On average, depression reduced with the passage of time for everyone. In contrast, overall satisfaction with life concurrently improved in the intervention group only. The significance of the interaction term in the satisfaction with life outcome multilevel analysis suggests that this can be directly attributable to the intervention itself rather than simply the passage of time. Similarly, anxiety reduced for the intervention group only with the interaction term bordering on significance.
ePACT is a programme that is based on sound mental health principles. It is largely based on cognitive behaviour therapy principles that are supplemented with some positive psychology and mindfulness meditation components. Cognitive therapy was first developed by Beck in the early 1960s and has since been adapted to treat a wide range of disorders and problems to good effect.18 Indeed, Beck reports that ‘more than 500 outcome studies have demonstrated the efficacy of cognitive behaviour therapy for a wide range of psychiatric disorders, psychological problems and medical problems with psychological components (p4).18 A recent meta-analysis examining the efficacy of cognitive behaviour therapy for the management of psychological outcomes following SCI confirmed that cognitive behaviour therapy is a valuable therapy option for individuals with SCI and comorbid mood disorders.19 To our knowledge, the impact of purposefully used positive psychology exercises and mindfulness meditation on individuals with SCI and comorbid mood disorder has not been reported previously; however, both activities have been shown to enhance well-being and effectively treat moderate depression in general population groups, as well as populations with various medical disorders.20, 21, 22, 23 For these reasons, the intervention itself is not likely to be the reason for the lack of significance found in the multivariate results.
Adherence and dropping-out are related problems of most treatments whether online or face-to-face. These issues, as they relate to online education and treatment for various health conditions including mental health, have already been the subject of several meta-analyses and reviews. For example, see Christensen et al.,24 Andrews et al.25 and Donkin et al.26 They report that adherence is often reported as high but could be as low as 48%; clinician contact/support is beneficial, and open-access web pages tend to have lower adherence. Interestingly, being in a relationship was statistically significant in the multivariate models where depression and helplessness were the dependent variables (DVs) (not reported), whereas they were not statistically significant when the models included those who dropped out as per the Intention-to-Treat Analyses reported in Table 3. One hypothesis is the several of those who dropped out had partners or families who were unhelpful, hence counterbalancing the constructive effect of being in a relationship in the alternate statistical models that were not reported. Lending weight to this hypothesis was that living unhelpful families was one of the difficulties that kept cropping up during the course of the study (discussed further below). Having said that the inconsistency could simply reflect the small sample size. Future studies with larger sample sizes could shed light on this conundrum.
Only a few of the participants reported completing all the ePACT modules, with most indicating that they had completed only half. It is not known which or how many of the modules are necessary for a therapeutic effect. For example, the developers of MoodGYM, a similar interactive depression treatment web programme developed in Australia, found a minimum of two modules necessary for significant mood improvement that lasted more than 12 months.27, 28 The implication is that a shortened version of ePACT may be as beneficial; however, it is unknown whether it was the same modules that were helpful to everyone or different modules that were helpful to different people. Clinician support was optional in ePACT and not everyone took up this option. However, in those who did, it can be anecdotally reported that different modules appealed to different people and the extra support was viewed as helpful, thus raising further research questions.
There was a systematic difference between the groups that relates to TSI and the level of SCI, which may have affected the result. It is possible that depression reduced in the waitlist control group as well as the intervention group because the knowledge that they would still be offered the intervention gave them hope of a more positive future. Further, the waitlist control participants tended to have been living with their injury over a longer period of time and therefore may have developed a capacity for patience. The passage of time might also have been helpful to everyone. However, the small number of intervention group participants who were assessed 6-month post-intervention were able to remain relatively free of symptoms of depression.
Another important consideration is the potential bias that self-selection may have had on the results. Screened participants presenting with mood disorder were offered a range of appropriate options, one of which was taking part in the ePACT trial. The pathways of the individuals who were screened included 19% who felt that they did not have a problem, and 13% were already seeing a health professional (psychologist or GP with whom they had a strong relationship) and 11% who accepted a referral for face-to-face support (further detail reported elsewhere).11 However, 27% did agree to the online intervention. Although this was the most common option taken, clearly it did not represent the majority. Those who agreed tended to be more depressed. The opportunity to examine systematic differences between those who opted for ePACT and those who did not was not possible in this study, aside from screening scores. However, this consideration has been considered by Donkin et al.29 who, when investigating sampling bias in a large Internet treatment trial, found few factors such as self-selection to be of concern. In addition, although those who agreed to take part in the study were significantly more depressed that those who did not in a statistical sense, it is less clear whether there was a clinically meaningful difference, as the median average of both groups fell within the moderate range.
The difficulties experienced in this project were frequent and repetitive and affected recruitment, adherence and dropouts. The recurrent obstacles were skills, technology and finances, schedules and chaotic circumstances. Lack of computer skills restricted entry for some people and was a noticeable reason for accepting referrals for face-to-face support. Furthermore, several individuals overestimated their computer skills and required extra support. Many individuals had limited finances, which meant that they had older technology that broke down and no funds for repairs within the study time frame. Many individuals were required to attend multiple appointments and/or take multiple tests, causing busy schedules, increased fatigue and little time for themselves. Finally, there were some individuals who lived among chaos including domestic violence and unhelpful family systems. Many of these difficulties would also impede the receipt from receiving face-to-face support. In reality, they are important matters that must be taken into consideration when developing interventions for this population.
There were several limitations to the study. One was the less than optimal sample size that resulted from the implementation of the programme being fixed to a funding time frame. Ideally, the sample size should be governed by the number of observations required to identify reliable change in outcomes while limiting type I and II errors as suggested by the power analysis, rather than being governed by funding and consequent restriction in implementation time. Claims that underpowered treatment studies might hinder the receipt of established efficacious treatment and/or potentially create more harm have been used to support the contention that it is unethical to conduct an underpowered study of medical interventions.30, 31 However, we would counter that the intervention was based on well-researched cognitive behaviour therapy principles rather than a novel or an experimental intervention, and we were providing education and evidence-based therapy to individuals who would not have received treatment at all. Untreated mood disorder is connected with increased medical costs (for health services as well as for individuals), unnecessary and/or prolonged distress and the possibility of increased risk of suicidality, especially in those with pre-morbid vulnerabilities.32 In addition, the lower-than-desired sample size may have resulted in an underestimation of the effectiveness of ePACT: repeating the study with a larger sample is recommended.
A further limitation was that the participants were self-selected. Only participants who had adequate English language skills, a computer, computer skills and Internet access participated; there were individuals who would have liked to take part but did not have the necessary skills and/or hardware. In addition, only participants who expressed interested in trying the programme took part rather than anyone who would potentially benefit from support. There was a lack of blinding in the study: allocation of group was achieved by the interviewer selecting the next allocation from the randomly ordered list, and every participant was aware of their allocation after completing their Time 1 interview. Nevertheless, this was a pragmatic study of individuals who lived in the community; the study could never replicate laboratory conditions. Finally, only two clinicians provided the clinical support (Migliorini and Sinclair): both have considerable experience in working with this particular population.
Clearly, online interventions will not become the default solution. Nevertheless, there are several further reasons why reliance on typical face-to-face psychological treatment may not be a practical option for many in this cohort. Mobility issues include wheelchairs and other gait aids, architectural inaccessibility, and transport restrictions complicating access. Gender is another reason. Males are overrepresented in SCI populations, and, in general, males are notoriously reluctant to seek help with emotional difficulties. Finally, the overarching goal of rehabilitation is to increase the independence of patients. This attitude tends to underpin many activities post rehabilitation as well. Yet, to seek help is to acknowledge vulnerability and work against the understandable need to be independent.
In summary, it is clear that online psychological treatment will not be a panacea for mental health problems in those with a SCI. This study, however, provides some empirical evidence that it is a potentially valuable and accessible addition to available mental health interventions. Additional clinician support probably facilitates better outcomes, which is in keeping with previous research.
Data archiving
There were no data to deposit.
References
Migliorini C, Tonge B, Taleporos G . Spinal cord injury and mental health. Aust N Z J Psychiatry 2008; 42: 309–314.
Williams R, Murray A . Prevalence of depression following spinal cord injury: a meta-analysis. Arch Phys Med Rehabil 2014; 96: 133–140.
Fann JR, Bombardier CH, Richards JS, Tate DG, Wilson CS, Temkin N et al. Depression After Spinal Cord Injury: Comorbidities, Mental Health Service Use, and Adequacy of Treatment. Arch Phys Med Rehabil 2011; 92: 352–360.
Migliorini C, New PW, Tonge B . Comparison of depression, anxiety and stress in persons with traumatic and non-traumatic spinal cord injury. Spinal Cord 2009; 47: 783–788.
DeJong G, Hoffman J, Meade M, Bonbardier C, Deutsch A, Nemunaitis G et al. Postrehabilitative Health Care for Individuals with SCI: Extending Health Care into the Community. Topics Spinal Cord Injury Rehabil 2011; 17: 46–58.
Liss HJ, Glueckauf RL, Ecklund-Johnson EP . Research on telehealth and chronic medical conditions: Critical review, key issues, and future directions. Rehabil Psychol 2002; 47: 8.
Andersson G, Cuijpers P . Internet-based and other computerized psychological treatments for adult depression: a meta-analysis. Cogn Behav Ther 2009; 38: 196–205.
Kaltenthaler E, Brazier J, De Nigris E, Tumur I, Ferriter M, Beverley C et al. Computerized cognitive behavior therapy for depression and anxiety update: A systematic review and economic evaluation. Health Technol Assess 2006; 10: 1–70.
Spek V, Cuijpers P, Nyklícek I, Riper H, Keyzer J, Pop V et al. Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: A meta-analysis. Psychol Med 2007; 37: 319–328.
Migliorini C, Tonge B, Sinclair A . Developing and piloting ePACT: a flexible psychological treatment for depression in people living with chronic spinal cord injury. Behav Change 2011; 28: 45–54.
Migliorini C, Sinclair A, Brown D, Tonge B, New P . Prevalence of mood disturbance in Australian adults with chronic spinal cord injury. Intern Med J 2015; 45: 1014–1019.
Lovibond SH, Lovibond PF. Manual for the Depression Anxiety Stress Scales 2 edn. Psychology Foundation of Australia Inc: Sydney, Australia. 1995.
International Wellbeing Group Personal Wellbeing Index. Deakin University, Australian Centre on Quality of Life: Melbourne, VIC, Australia. 2006.
Migliorini C, Elfström ML, Tonge B . Translation and Australian validation of the spinal cord lesion-related coping strategies and emotional wellbeing questionnaires. Spinal Cord 2008; 46: 690–695.
Cohen J . Statistical Power Analysis for the Behavioral Sciences 2 edn. Lawrence Erlbaum Associates: HIllsdale, New Jersey. 1988.
Kwok O-M, Underhill AT, Berry JW, Luo W, Elliott TR, Yoon M et al. Analyzing longitudinal data with multilevel models: an example with individuals living with lower extremity intra-articular fractures. Rehabil Psychol 2008; 53: 370–386.
Kreft I, de Leeuw J . Introducing Multilevel Modeling. Sage Publications: London. 1999.
Beck JS . Cognitive Behavior Therapy: Basics and Beyond. The Guildord Press: New York, New York. 2011.
Dorstyn D, Mathias J, Denson L . Efficacy of cognitive behavior therapy for the management of psychological outcomes following spinal cord injury: A meta-analysis. J Health Psychol 2010; 16: 374–391.
Seligman M, Steen T, Park N, Peterson C . Positive psychology progress: empirical validation of interventions. Am Psychol 2005; 60: 410–421.
Sin NL, Lyubomirsky S . Enhancing well-being and alleviating depressive symptoms with positive psychology interventions: a practice-friendly meta-analysis. J Clin Psychol 2009; 65: 467–487.
Hofmann S, Sawyer A, Witt A, Oh D . The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. J Consult Clin Psychol 2010; 78: 169–183.
Layous K, Chancellor J, Lyubomirsky S, Wang L, Doraiswamy P . Delivering happiness: translating positive psychology intervention research for treating major and minor depressive disorders. J Altern Complement Med 2011; 17: 675–683.
Christensen H, Griffiths KM, Farrer L . Adherence in internet interventions for anxiety and depression: systematic review. J Med Internet Res 2009; 11: e13.
Andrews G, Cuijpers P, Craske M, McEvoy P, Titov N . Computer therapy for the anxiety and depressive disorders is effective, acceptable and practical health care: A meta-analysis. PLoS ONE 2010; 5: e13196.
Donkin L, Christensen H, Naismith SL, Neal B, Hickie IB, Glozier N et al. A systematic review of the impact of adherence on the effectiveness of e-Therapies. J Med Internet Res 2011; 13: e52.
National Institute for Mental Health Research. MoodGYM: frequently asked questions. n.d. Available from: https://moodgym.anu.edu.au/welcome/faq (11 December 2014).
Griffiths KM, Christensen H . Internet-based mental health programs: A powerful tool in the rural medical kit. Aust Jf Rural Health 2007; 15: 81–87.
Donkin L, Hickie IB, Christensen H, Naismith SL, Neal B, Cockayne NL et al. Sampling bias in an internet treatment trial for depression. Transl Psychiatry 2012; 2: e174.
Janosky JE . The ethics of underpowered clinical trials. JAMA 2002; 288: 2118–2119.
Rosoff PM . Can Underpowered Clinical Trials Be Justified? IRB 2004; 26: 16–19.
Craig A, Tran Y, Middleton J . Psychological morbidity and spinal cord injury: a systematic review. Spinal Cord 2008; 47: 108–114.
Acknowledgements
We thank Dr John Taffe, biostatistician, Centre for Developmental Psychiatry and Psychology, for his technical assistance. We also thank Drs Brian Anthonisz, Cristina Manu, Parinaz Sharifi and especially Ms Marie Mallawarachchy for their assistance in the screening of patients at the Caulfield Hospital. This work was supported by beyondblue: Victorian Centre of Excellence 2011 Research Grant Round: Randomised control trial of ePaCT: a flexible treatment for depression and anxiety in adults living with chronic spinal cord injury. This work was supported by beyondblue: Victorian Centre of Excellence 2011 Research Grant. The RCT was registered at A&NZ Clinical Trial Registry (ACTRN 12612000587808).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Migliorini, C., Sinclair, A., Brown, D. et al. A randomised control trial of an Internet-based cognitive behaviour treatment for mood disorder in adults with chronic spinal cord injury. Spinal Cord 54, 695–701 (2016). https://doi.org/10.1038/sc.2015.221
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2015.221
This article is cited by
-
The impact of technology systems and level of support in digital mental health interventions: a secondary meta-analysis
Systematic Reviews (2023)
-
Internet-based and mobile-based cognitive behavioral therapy for chronic diseases: a systematic review and meta-analysis
npj Digital Medicine (2023)
-
Current Approaches in Telehealth and Telerehabilitation for Spinal Cord Injury (TeleSCI)
Current Physical Medicine and Rehabilitation Reports (2022)
-
Guided internet-delivered cognitive-behaviour therapy for persons with spinal cord injury: a feasibility trial
Spinal Cord (2020)
-
Work and SCI: a pilot randomized controlled study of an online resource for job-seekers with spinal cord dysfunction
Spinal Cord (2019)