Abstract
Study design:
Cross-sectional.
Objectives:
To compare differences in self-reported health status, participation and life satisfaction outcomes between adults with a spinal cord injury (SCI) sustained during paediatric (P) versus adulthood (A) years.
Setting:
Ontario, Canada.
Methods:
Secondary analysis of data from the Study of Health and Activity in People with SCI. Eighty-seven participants who sustained an SCI prior to age 19 (M±s.e.=25±1.5 years postinjury (YPI)) were matched for lesion level (C2–L5), severity (complete/incomplete), gender, age, education and ethnicity with 87 participants who sustained an SCI at ⩾age 19 years (MYPI=12.8±1.1).
Results:
Those with a paediatric SCI reported significantly less pain, fewer visits to the physician in the past year, greater functional independence, social participation, occupational participation and minutes per day of moderate-to-vigorous physical activity than those who sustained an SCI in adulthood. No significant differences were found for the measures of depression, perceived health status or life satisfaction (P>0.05). With the exception of moderate-to-vigorous physical activity and visits to the physician in the past year, between-group differences were independent of YPI.
Conclusions:
Regardless of time since injury, people who sustained a paediatric SCI reported better health and greater participation than those injured in adulthood. Nevertheless, both groups scored well below able-bodied normative values for all measures. The results highlight the importance of a comprehensive life-course approach to SCI rehabilitation, irrespective of age at the time of injury.
Similar content being viewed by others
Introduction
It is well documented that adults with spinal cord injury (SCI) have poorer health and psychological well-being and lower rates of participation than adults in the able-bodied population.1 However, there may be differences in outcomes for those who sustained a SCI during their childhood/youth versus adulthood. Identification of such differences is important for ensuring that any distinct needs of these two groups are met.
A small body of literature has attempted to compare aspects of health, psychosocial well-being and participation among adults who sustained an SCI during childhood/youth versus adulthood.2, 3, 4, 5, 6 Several of these studies have involved collecting data from participants who sustained an SCI during childhood/youth and comparing the results to previously published data collected from individuals who sustained an SCI during adulthood (for example, data obtained via the US SCI Model Systems (National Spinal Cord Injury Statistical Centre1)). For instance, in one study, 216 younger adults (mean age=29 years) who had sustained an SCI in childhood/youth completed a survey regarding medical complications experienced over the previous 3 years.7 Hwang et al.6 suggested that the prevalence rates of urinary tract infections, autonomic dysreflexia, pressure ulcers, bladder and bowel incontinence and urinary tract stones found in that sample were comparable to those observed in adult-sustained SCI samples.8, 9, 10, 11
In another study, 283 adults with paediatric-sustained SCI (mean age=34 years) were interviewed to assess employment outcomes over time.6 The authors discussed their findings relative to data collected through 18 SCI Model Systems.12 They concluded that the employment rates of their sample were similar to the rates reported in the model systems data for respondents with an associate’s or a bachelor’s degree but were much higher for those with a post-baccalaureate degree. The authors noted, however, that their sample was younger than the model systems cohort, and the age difference could have confounded their results. Indeed, an important limitation of studies that have used this approach for comparing data from adults with a paediatric- versus adulthood-sustained SCI is that the samples are not matched for key injury-related (for example, injury severity, time since injury) or demographic variables (for example, gender, ethnicity) that could be related to the outcomes of interest. Another limitation is that, although these studies have typically concluded that the two cohorts have similar outcomes, such conclusions have not been confirmed by statistical analyses.
A few studies have used statistical methods to compare outcomes among those with paediatric- versus adult-sustained SCI. These studies have produced mixed findings. For example, in a study conducted in the United States, people who sustained an SCI at age ⩽15 years had a 31% increase in their annual odds of mortality compared with those injured at age ⩾16 years.13 No risk factors or causes of mortality were measured that could explain these findings, but the authors proposed that complications associated with paediatric SCI could contribute to increased mortality. Notably, differences in mortality held after controlling for participants’ age, sex, race, injury severity and era of injury.
In contrast, a study of Finnish adults with SCI revealed that people who sustained an SCI at age <17 years reported significantly better perceived health and greater overall health-related quality of life than those injured in adulthood.14 On a set of single-item measures, the group with paediatric-sustained injuries also reported a higher level of employment, but no differences in functioning, social participation, pain, depression or distress compared with the group with a SCI sustained in adulthood. The analyses did not control for any between-group differences in injury-related or demographic characteristics. However, in a study conducted in the United Kingdom, a group of adults who sustained an SCI before the age of 16 years were matched for the injury level and time since injury (but not for demographics). No between-group differences emerged on a standardized measure of depressive symptoms.15
Despite the use of statistical methods, it is still difficult to draw conclusions from this set of studies. Not only are the findings inconsistent but also insufficient matching and controlling for confounds,14, 15 the use of single-item measures of complex constructs14 and the lack of data on specific aspects of health and well-being13 make it difficult to determine whether differences do exist between adults with paediatric- versus adult-sustained SCI. This is an important research question; such differences could have implications for rehabilitation and reintegration after injury and lead to the formulation of recommendations for policy reform to provide the best care for those with SCI.
The purpose of the present study was to statistically test for differences in health (physical and mental), participation and life satisfaction outcomes in samples of adults with a paediatric- versus an adult-sustained SCI. To address the limitations of previous research, both samples were drawn from the same cohort study and matched for injury-related and demographic variables. Well-validated, multi-item measures were used to assess the outcomes of interest. Although the limitations and ambiguities of the existing research made it difficult to formulate hypotheses, tentative predictions were made. Given the higher odds of mortality observed for those with a paediatric-sustained SCI,13 this group was expected to report poorer health-related outcomes than those who sustained an SCI in adulthood. However, given evidence of greater employment and health-related quality of life in samples with paediatric-sustained injuries,6, 14 this group was expected to report higher scores on measures of participation and life satisfaction than the group who had sustained an SCI during adulthood.
Methods
Participants
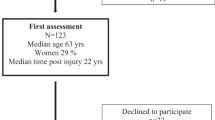
This study was a secondary analysis of data collected in the Study of Health and Activity in People with SCI (SHAPE-SCI). All applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research. Participants were recruited from four rehabilitation and research centres across Ontario, Canada. Study inclusion criteria were participants who incurred a traumatic SCI at least 12 months prior to study enrolment, used a mobility device outside of the home and were at least 18 years of age. The SHAPE-SCI data set included 87 participants who sustained an SCI prior to age 19 years. These individuals were matched (in order of priority) for lesion level, injury severity, gender, age, level of education and ethnicity with 87 SHAPE-SCI participants injured at age ⩾19 years. The strong negative correlation between years postinjury (YPI) and age rendered it impossible to match for both of these characteristics. A decision was made to match based on age (see Table 1) and to conduct analyses to determine whether YPI confounded the interpretation of any observed differences (refer to 'Data analyses' section).
Procedure
A full description of the SHAPE-SCI methods has been previously reported (Martin Ginis et al.16). To briefly summarise the protocol, 695 men and women with SCI were enrolled in an 18-month observational study. For this secondary analysis, only baseline data were analysed. Research Ethics Board approval was obtained by all four data collection sites, and all participants provided informed consent.
Measures
Health measures
Functional independence was assessed using the 13-item motor subscale of the Functional Independence Measure (FIM).17 Response options range from 1 to 7 where higher scores represent greater independence (1=complete dependence and 7=complete independence). FIM motor scores have shown adequate inter-rater reliability when comparing clinician scores to self-report scores in a sample of 40 men and women with chronic SCI (r=0.73).18 The FIM has been validated against the Walking Index for Spinal Cord Injury and the Berg Balance Scale in 141 people with SCI at acute care entry, 3, 6 and 12 months after injury, demonstrating strong correlations with these measures (r=0.73–0.77 and r=0.72–0.77, respectively).19
Pain and general health were measured with the Short Form (36) Health Survey (SF-36).20 A single question asked participants’ general perception of health and was rated on a 5-point scale (1=poor and 5=excellent). In addition, four health-related statements (for example, 'I seem to get sick a little easier than others' and 'I expect my health to get worse') were rated for how true or false the statements were on a 5-point Likert scale (1=definitely true and 5=definitely false). Bodily pain severity over the past 4 weeks was assessed on a 6-point scale (1=none and 6=very severe). The extent to which bodily pain had interfered with normal work was evaluated on a 5-point scale (1=not at all and 5=extremely). Analyses of inter-rater reliability have been conducted in 20 people with chronic SCI and shown adequate intraclass correlation coefficients (ICCs) of 0.4 and 0.7 for the health and pain subscales, respectively.21 Construct validity of the general health and pain subscores of the SF-36 were assessed comparing scores with the Behavioural Risk Factor Surveillance System subscales and have demonstrated moderate correlations of 0.4 and 0.5 in a sample of 183 US veterans with SCI.22
Physician visits were evaluated using a single item from the Health Care Utilisation Inventory.23 Participants were asked the number of times they had visited a physician in the past 6 months.23 This item has shown excellent test–retest reliability in a small sample of patients with chronic disease (r=0.76).23 Validity has not been reported for this measure.
Depressive symptoms were measured using the Patient Health Questionnaire (PHQ-9). Frequencies of 9 Diagnostic and Statistical Manual for Mental Disorders, Fourth Edition criteria items were assessed on a scale of 0–3 (0=not at all and 3=nearly every day).24 The PHQ-9 has been examined in 6000 clinical patients and demonstrated excellent test–retest reliability (r=0.84).24 Moderate correlations between total PHQ-9 scores and prevalence of Major Depressive Disorder have been shown in 727 US patients with SCI (r=0.5).25
Participation measures
Physical activity participation in leisure time physical activity was assessed using the Physical Activity Recall Assessment for People with Spinal Cord Injury (PARA-SCI).26 A comprehensive, telephone-based interview was conducted where participants were asked to recall the duration and intensity of all activities (including both activities of daily living and leisure time physical activity) performed in the morning, afternoon and evening over the past 3 days. Only moderate–vigorous intensity leisure time physical activity was used in this secondary analysis, as this is the intensity supported to improve fitness.27 When administered to 102 men and women with chronic SCI, the PARA-SCI demonstrated similar or superior test–retest reliability for moderate- and heavy-intensity physical activity (average ICC=0.75 and 0.79, respectively) in comparison with other known measures of physical activity (for example, Godin Leisure Time Physical Activity Recall, CARDIA Physical Activity Questionnaire).26 The PARA-SCI has also been shown to be the best estimate of physical activity energy expenditure in a small sample of people with SCI when compared with doubly labelled water (r2=0.62).28
Occupational and social participation activities were assessed using the Craig Handicap Assessment and Reporting Technique (CHART).29 As part of the CHART measure, the seven-item Occupation and the six-item Social Integration subscales were used for the present analysis. Each subscale has a maximum score of 100, indicating no disability.29 In a sample of 135 participants recruited from eight of the model SCI centres, high test–retest reliability (range=0.80–0.95) was demonstrated when administering the CHART at baseline and at 1 week follow-up.30 Discriminant validity was assessed in a sample of employed versus unemployed Japanese SCI patients showing significantly higher CHART occupation scores in those who declared an employed status.31 CHART Social Integration was very strongly correlated with the Community Integration Questionnaire-Social Integration scores in 28 participants with chronic SCI (r=0.77).32
Life satisfaction was measured using the Satisfaction with Life Scale (SWLS).33 Five questions related to life satisfaction set in the present, past and future were measured on a seven-point Likert scale (1= strongly disagree and 7=strongly agree). A review of the quality-of-life studies in people with SCI reported the SWLS 2-week test–retest reliability values to be low–moderate (ICC=0.39–0.65).34 In a sample of 225 people with recently acquired SCI, the SWLS demonstrated strong and significant correlations with both the Life Satisfaction Questionnaire and the Life Satisfaction measure (r=0.59–0.6).35
Normative values for the above measures in able-bodied populations from Canada are presented for comparison (Table 2). Normative data scores that were reported in a different format than what was previously published for the SHAPE-SCI data set were converted to match the same scales of the SHAPE-SCI data for comparison. As such, SF-36 pain scores were converted from percentage values to a score out of 11, and the general health scores were converted from percentages to a 5-point scale.
Data analyses
Demographic and injury-related data were summarised using descriptive statistics and compared between groups using a t-test and χ2 analyses. Paired-samples, two-tailed t-tests were conducted to test for between-group differences on each study measure.
As noted in the 'Participants' section, participants could not be matched for YPI. Furthermore, YPI could not be used as a covariate in an analysis of covariance to compare outcomes across groups, because this would violate the analysis of covariance assumption of independence of the independent/grouping variable and covariate.36 Nevertheless, we wanted to have confidence that any observed differences on the outcome measures reflected differences based on when participants were injured (that is, childhood/youth versus adulthood) rather than differences in YPI. Accordingly, two-tailed, Pearson product–moment correlations were computed to test the independence of YPI and each outcome measure. If an outcome measure was not significantly correlated with YPI (that is, P>0.05), then significant between-group differences on that measure could be attributed to differences in when the injury occurred rather than differences in YPI.
Results
Regarding the health-related measures, contrary to hypothesis, participants who sustained a paediatric SCI reported significantly greater functional independence, t(86)=2.3, P=0.03, less pain, t(86)=−2.5, P=0.02, and fewer visits to the doctor in the past year, t(86)=−2.1, P=0.04, than participants injured during adulthood. No significant differences were found for the measures of perceived health status or depressive symptoms (Ps>0.05).
With regard to participation, as hypothesised, study participants who sustained an SCI in their childhood/youth reported more minutes of moderate–vigorous leisure time physical activity, t(86)=1.9, P=0.05, and scored higher on measures of social participation, t(84)=2.1, P=0.04, and occupational participation, t(80)=2.2, P=0.03, than participants who sustained an SCI in adulthood.
Regarding life satisfaction, contrary to hypothesis, there were no significant between-group differences.
Correlational analyses revealed small, albeit significant, negative associations between YPI and visits to the doctor in the past year (r=−0.16, P=0.04) and between YPI and moderate–vigorous physical activity (r=−0.20, P=0.009). Thus, with greater YPI, there was a decrease in the number of doctor visits, as well as the number of minutes per day of physical activity. No other correlations were significant, indicating that all other differences between the two groups were statistically independent of YPI.
Discussion
The purpose of this study was to compare health, participation and life satisfaction outcomes between individuals with a paediatric- versus adult-sustained SCI. Contrary to hypothesis, individuals injured in their paediatric years reported better long-term health in terms of less pain, greater functional independence and fewer visits to a physician over the past year. Yet, as hypothesised, adults who sustained a paediatric SCI had higher scores on measures of social, occupational and physical activity participation.
Although a previous study reported greater odds of mortality for adults who sustained an SCI during their childhood/youth,13 we found that adults with a paediatric-sustained SCI reported more positive scores on measures of health outcomes than did those who sustained an SCI during adulthood. It is possible that our health-related outcome measures—pain, function, physician visits—did not capture factors that might be associated with increased risk for mortality. For instance, Shavelle et al.13 suggested that there may be metabolic effects or compromised organ development among people who sustain an SCI in childhood, which could increase risk of mortality. Further research is needed to address this issue and to determine whether people with paediatric- versus adult-sustained SCI differ on risk factors for metabolic syndrome, cardiovascular disease, diabetes and other conditions linked with mortality.
Nevertheless, our results suggest that, on some health-related dimensions, adults who sustained an SCI during their paediatric years fare better than those who were injured in adulthood. Those with youth-sustained SCI reported less pain and higher functional independence than the adult-sustained sample. One plausible explanation for these findings is that physical activity and fitness have been shown to be negatively correlated with pain37 and functional independence outcomes,38 and the cohort injured during childhood/youth was more physically active than that injured in adulthood. It should be noted, however, that the between-group differences in moderate–vigorous physical activity as well as physician visits were related to YPI and need to be interpreted with caution. Self-management of one’s health and health-related behaviours may improve with time and experience living with an SCI.
Consistent with previous literature,14 adults who sustained a paediatric SCI also scored higher on measures of participation. These results may reflect differences in the availability of support for reintegration for children/youth versus adults. For example, school-based accommodations are often legally mandated for students with SCI and other disabilities. In contrast, adults with SCI typically experience numerous barriers to returning to work, such as lack of transportation, need for on-the-job support, requirements for job accommodations,39 and negative stereotypes and misperceptions about hiring a person with a disability. Thus the reintegration of a person with SCI into community life may be more comprehensive when the point of re-entry is school rather than the workforce and could explain why those with paediatric-sustained SCI scored higher on measures of social and employment participation than those with an adult-sustained SCI. Strategies directed at policy, organisational and community levels to facilitate re-entry into the workforce could alleviate disparities in social and employment participation observed among those who have sustained an SCI in adulthood. For instance, a Dutch survey of 57 people with chronic SCI examined the process of reintegration into paid work following a traumatic SCI. Results supported such indicators as patient expectations to resume work, vocational retraining and job adaptation and modifications are associated with higher employment rates.40 They implicate that, in particular, the rehabilitation team can have an active role in forming a reintegration plan in conjunction with the patient and the employer.40
Interestingly, even though physical activity was negatively correlated with YPI, and those who were injured in childhood/youth had been injured for longer, this group still reported greater participation in physical activity than the group injured during adulthood. As with employment, there may be more support and opportunities in the school and community for children with disabilities to participate in physical activity than there are for adults with disabilities. For example, children with disabilities would have opportunities for adapted forms of physical education during the school day.41, 42
It should be noted, however, that, although those with paediatric-sustained injury reported higher health and participation outcomes than those with adult-sustained injury, compared with national normative data for the general population, both groups reported lower scores for all measures.1 Disparities in participation between able-bodied and people with SCI samples further highlight the need for more effective reintegration strategies.
With regard to depression, our findings were consistent with a previous study that found no differences in depressive symptomatology between adults who incurred an SCI in childhood versus adulthood and who were matched for injury time and severity.15 Overall, scores on the depression measure were relatively low in both the adult- and youth-sustained SCI samples. Nevertheless, these depressive symptom values are higher than those reported for the able-bodied normative values. Thus it remains that efforts should be devoted to improving the mental well-being of people with SCI.
Given the better health and participation outcomes reported by those who incurred a paediatric SCI, it is somewhat surprising that there were no between-group differences in perceived health status or life satisfaction. However, perceived health status and life satisfaction are relatively global measures of well-being.43 It is possible that, when formulating these global perceptions, respondents took into account other factors (for example, diagnoses of secondary health conditions, mobility, the ability to fulfil social roles) that are known to influence life satisfaction and other aspects of well-being in people with SCI43, 44 but were not measured in the present study. Further research is needed to determine whether there are differences in these factors as a function of paediatric- versus adult-sustained SCI.
Conclusion
Overall, this study has generated new knowledge regarding differences in health- and participation-related outcomes for those who sustained an SCI in childhood/youth versus adulthood. Moreover, the study methods addressed several limitations of previous work, and the results provide a basis for future investigations of differences between these two SCI sub-groups. A limitation to the study is that the sample was drawn from a single province in Canada. The results may not be generalisable to other provinces or countries where reintegration strategies differ for children and adults. In addition, because of the cross-sectional study design, it is not possible to determine what causes the observed differences or how they develop over time. Nevertheless, the finding of more positive scores on measures of health and participation outcomes in paediatric- than adult-sustained SCI samples suggest that these domains may be better supported for children/youth who sustain an SCI than for adults. However, the need for adult reintegration supports should not detract from the ongoing support needed for those with paediatric-sustained injury, whose outcomes are still well below values reported in the able-bodied population.
Data archiving
There were no data to deposit.
Change history
05 December 2016
This article has been corrected since Advance Online Publication and an erratum is also printed in this issue
References
National Spinal Cord Injury Statistical Centre. Spinal Cord Injury Model Systems 2013 Annual Report Complete Public Version. Birmingham, UK, 2013, 13–89.
January AM, Zebracki K, Chlan KM, Vogel LC . Understanding post-traumatic growth following pediatric-onset spinal cord injury: the critical role of coping strategies for facilitating positive psychological outcomes. Dev Med Child Neurol 2015; 57: 1143–1149.
Vogel LC, Hickey KJ, Klaas SJ, Anderson CJ . Unique issues in pediatric spinal cord injury. Orthop Nurs 2004; 23: 300–308.
Anderson CJ, Krajci KA, Vogel LC . Community integration among adults with spinal cord injuries sustained as children or adolescents. Dev Med Child Neurol Child Neurol 2003; 45: 129–134.
Kelly EH, Mulcahey MJ, Klaas SJ, Russell HF, Anderson CJ, Vogel LC . Psychosocial outcomes among youth with spinal cord injury and their primary caregivers. Top Spinal Cord Inj Rehabil 2012; 18: 67–72.
Hwang M, Zebracki K, Chlan KM, Vogel LC . Longitudinal employment outcomes in adults with pediatric-onset spinal cord injury. Spinal Cord 2014; 52: 477–482.
Vogel L, Krajci K, Anderson C . Adults with pediatric-onset spinal cord injury: part 1: prevalence of medical complications. J Spinal Cord Med 2002; 25: 106–116.
Levi R, Hultling C, Nash MS, Seiger A . The Stockholm spinal cord injury study: 1. Medical problems in a regional SCI population. Paraplegia 1995; 33: 308–315.
Walker DK, Wilber N, Meyers AR, Mitra M, Allen D . Predictors of secondary conditions in a sample of independently living adults with high-level spinal cord injury. Top Spinal Cord Inj Rehabil 2000; 6: 1–8.
Noreau L, Proulx P, Gagnon L, Drolet M, Laramee M-T . Secondary impairments after spinal cord injury. Am J Phys Med Rehabil 2000; 79: 526–535.
Hwang M, Zebracki K, Chlan KM, Vogel LC . Longitudinal changes in medical complications in adults with pediatric-onset spinal cord injury. J Spinal Cord Med 2014; 37: 171–178.
Krause JS, Kewman D, DeVivo MJ, Maynard F, Coker J, Roach MJ et al. Employment after spinal cord injury: an analysis of cases from the Model Spinal Cord Injury Systems. Arch Phys Med Rehabil 1999; 80: 1492–1500.
Shavelle RM, Devivo MJ, Paculdo DR, Vogel LC, Strauss DJ . Long-term survival after childhood spinal cord injury. J Spinal Cord Med 2007; 30 (Suppl 1): S48–S54.
Kannisto M, Merikanto J, Alaranta H, Hokkanen H, Sintonen H . Comparison of health-related quality of life in three subgroups of spinal cord injury patients. Spinal Cord 1998; 36: 193–199.
Kennedy P, Gorsuch N, Marsh N . Childhood onset of spinal cord injury: self-esteem and self-perception. Br J Clin Psychol 1995; 34: 581–588.
Martin Ginis KA, Latimer AE, Buchholz AC, Bray SR, Craven BC, Hayes KC et al. Establishing evidence-based physical activity guidelines: methods for the Study of Health and Activity in People with Spinal Cord Injury (SHAPE SCI). Spinal Cord 2008; 46: 216–221.
Dijkers MPJ, Yavuzer G . Short versions of the telephone motor functional independence measure for use with persons with spinal cord injury. Arch Phys Med Rehabil 1999; 80: 1477–1484.
Grey N, Kennedy P . The functional independence measure: a comparative study of clinician and self- ratings. Paraplegia 1993; 31: 457–461.
Ditunno JF, Barbeau H, Dobkin BH, Elashoff R, Harkema S, Marino RJ et al. Validity of the walking scale for spinal cord injury and other domains of function in a multicenter clinical trial. Neurorehabil Neural Repair 2007; 21: 539–550.
Ware JE, Sherbourne CD . The MOS 36-item short-form health survey (SF-36). Med Care 1992; 30: 473–483.
Lin M-R, Hwang H-F, Chen C-Y, Chiu W-T . Comparisons of the brief form of the World Health Organization Quality of Life and Short Form-36 for persons with spinal cord injuries. Am J Phys Med Rehabil 2007; 86: 104–113.
Andresen EM, Fouts BS, Romeis JC, Brownson CA . Performance of health-related quality-of-life instruments in a spinal cord injured population. Arch Phys Med Rehabil 1999; 80: 877–884.
Lorig K, Stewart A, Ritter P, Gonzalez V, Laurent D, Lynch J . Outcome Measures for Health Education and Other Health Care Interventions. Sage: Thousand Oaks, CA, USA. 1996.
Kroenke K, Spitzer RL, Williams JBM . The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 2001; 16: 606–613.
Kraus JS, Saunders LL, Reed KS, Coker J, Zhai Y, Johnson E . Comparison of the Patient Health Questionnaire and the Older Adult Health and Mood Questionnaire for self-reported depressive symptoms after spinal cord injury. Rehabil Psychol 2009; 54: 440–448.
Martin Ginis KA, Latimer AE, Hicks AL, Craven BC . Development and evaluation of an activity measure for people with spinal cord injury. Med Sci Sports Exerc 2005; 37: 1099–1111.
Martin Ginis KAM, Hicks AL, Latimer AE, Warburton DER, Bourne C, Ditor DS et al. The development of evidence-informed physical activity guidelines for adults with spinal cord injury. Spinal Cord 2011; 49: 1088–1096.
Tanhoffer RA, Tanhoffer AIP, Raymond J, Hills AP, Davis GM . Comparison of methods to assess energy expenditure and physical activity in people with spinal cord injury. J Spinal Cord Med 2012; 35: 35–45.
Hall KM, Brooks CA, Whiteneck G, Dijkers M, Krause JS . The Craig Handicap Assessment and Reporting Technique (CHART): metric properties and scoring. Top Spinal Cord Inj Rehabil 1998; 4: 16–30.
Dijkers M . Scoring CHART: survey and sensitivity analysis. J Am Paraplegia Soc 1991; 14: 85–86.
Tozato F, Tobimatsu Y, Wang C, Iwaya T, Kumamoto K, Ushiyama T . Reliability and validity of the Craig Handicap Assessment and Reporting Technique for Japanese individuals with spinal cord injury. Tohoku J Exp Med 2005; 205: 357–366.
Gontkovsky ST, Russum P, Stokic DS . Comparison of the CIQ and chart short form in assessing community integration in individuals with chronic spinal cord injury: a pilot study. NeuroRehabilitation 2009; 24: 185–192.
Diener E, Emmons R, Larsen J, Griffin S . The Satisfaction With Life Scale. J Pers Assess 1985; 5: 164–172.
Hill M, Noonan V, Sakakibara B, Miller W . Quality of life instruments and definitions in individuals with spinal cord injury : a systematic review. Spinal Cord 2010; 48: 438–450.
Post MWM, Van Leeuwen CM, Van Koppenhagen CF, De Groot S . Validity of the Life Satisfaction questions, the Life Satisfaction Questionnaire, and the Satisfaction With Life Scale in persons with spinal cord injury. Arch Phys Med Rehabil 2012; 93: 1832–1837.
Field A. Discovering Statistics Using SPSS. Sage Publications Ltd: London, UK, 2009, pp 395–421.
Tawashy AE, Eng JJ, Lin KH, Tang PF, Hung C . Physical activity is related to lower levels of pain, fatigue and depression in individuals with spinal-cord injury: a correlational study. Spinal Cord 2009; 47: 301–306.
Noreau L, Shephard RJ, Simard C, Pare G, Pomerleau P . Relationship of impairment and functional ability to habitual activity and fitness following spinal cord injury. Int J Rehabil Res 1993; 16: 265–275.
Targett P, Wehman P, Young C . Return to work for persons with spinal cord injury: designing work supports. NeuroRehabilitation 2004; 19: 131–139.
Schönherr MC, Groothoff JW, Mulder GA, Schoppen T, Eisma WH . Vocational reintegration following spinal cord injury: expectations, participation and interventions. Spinal Cord 2004; 42: 177–184.
Block ME, Obrusnikova I . Inclusion in physical education: a review of the literature from 1995-2005. Adapt Phys Activ Q 2007; 24: 103–124.
Murphy NA, Carbone PS . Promoting the participation of children with disabilities in sports, recreation and physical activities. Pediatrics 2008; 121: 1057–1061.
Dijkers MPJM . Quality of life of individuals with spinal cord injury: a review of conceptualization, measurement and research findings. J Rehabil Res Dev 2005; 42: 87–110.
Post MWM . Definitions of quality of life : what has happened and how to move on. Top Spinal Cord Inj Rehabil 2014; 20: 187–199.
Hopman WM, Towheed T, Anastassiades T, Tenenhouse A, Poliquin S, Berger C et al. Canadian normative data for the SF-36 health survey. Can Med Assoc J 2000; 163: 265–271.
Leavens A, Patten SB, Hudson M, Baron M, Thombs BD . Influence of somatic symptoms on patient health questionnaire-9 depression scores among patients with systemic sclerosis compared to a healthy general population sample. Arthritis Care Res 2012; 64: 1195–1201.
Colley RC, Garriguet D, Janssen I, Craig CL, Clarke J, Tremblay MS . Physical activity of Canadian children and youth : accelerometer results from 2007-2009 Canadian Health Measures Survey. Stat Canada Cat. no. 82-003-XPE. Health Rep 2011; 22: 15–24.
Martin Ginis KA, Hicks AL, Latimer AE, Warburton DER, Bourne C, Ditor DS et al. The development of evidence-informed physical activity guidelines for adults with spinal cord injury. Spinal Cord 2011; 49: 1088–1096.
Blais MR, Vallerand RJ, Pelletier LG, Brière NM . L'échelle de satisfaction de vie: validation Canadienne-Française du ‘Satisfaction With Life Scale’. Can J Behav Sci 1989; 21: 210–223.
Acknowledgements
SHAPE-SCI was funded by an Operating Grant from the Canadian Institutes of Health Research (CIHR). Dr Gorter holds the Scotiabank Chair for Child Health Research (2012–2014).
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Ma, J., Post, M., Gorter, J. et al. Differences in health, participation and life satisfaction outcomes in adults following paediatric- versus adult-sustained spinal cord injury. Spinal Cord 54, 1197–1202 (2016). https://doi.org/10.1038/sc.2016.45
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2016.45