Abstract
Study design:
Prospective study.
Objective:
To determine the integrity of the hypothalamic-pituitary-testicular axis in healthy men with spinal cord injury (SCI).
Methods:
Thirty healthy men with chronic SCI (37±10 years) and thirty-eight able-bodied (AB) controls (36±10 years) participated. Gonadotropin-releasing hormone (GnRH; 100 μg IV) was administered to determine gonadotropin release, and human chorionic gonadotropin (hCG; 4000 IU IM) was administered to determine testosterone (T) secretion. Responses to stimulation were categorized as ‘responder’ or ‘non-responder’ by clinical criteria. Single factor ANOVA with repeated measures was performed to identify group differences.
Results:
The proportion of responders to pituitary GnRH stimulation was similar in the SCI group (22 subjects (73%) for the follicular-stimulating hormone (FSH) and 23 subjects (76%) for the luteinizing hormone (LH) to that of the AB group. The SCI-responder group had an increased FSH response after stimulation compared with the AB-responder group (P<0.05). The SCI-responder group had a greater LH area under the curve to GnRH stimulation than the AB-responder group (P=0.06). The peak FSH response was at 60 min and the peak LH response at 30 min, regardless of group designation. All groups had similar increases in serum T concentration to hCG stimulation.
Conclusions:
The pituitary response to stimulation in healthy men with SCI revealed an augmented FSH response; LH response only trended higher. The testicular response to provocative stimulation was similar in hypogonadal and eugondal subjects and in GnRH responders and non-responders. These findings suggest a lack of hypothalamic drive of pituitary gonadotropin release in healthy people with chronic SCI.
Similar content being viewed by others
Introduction
Because of the general awareness of fertility problems and low testosterone levels in subgroups of adult men with chronic spinal cord injury (SCI), the question of disordered regulation of the hypothalamic-pituitary-testicular axis has been considered as one possible contributing etiology for these findings. Early reports were inconclusive with regard to testicular function in men with SCI.1, 2 The apparent question of whether a testicular or a central defect is present in those with SCI could, in part, be attributed to varying factors in the selection of the population studied, the influence of health and nutrition parameters, medication effects, level and duration of SCI and/or to differences in methodology. Recently, however, a study performed in a larger population of men with SCI demonstrated that a sizeable proportion of this group was testosterone (T) deficient, with the prevalence of deficiency increasing with advancing age.3 Circulating levels of T have a substantial influence on soft tissue body composition,4, 5 physical performance,6 energy expenditure,7 carbohydrate and lipid metabolism,8 risk of cardiovascular disease9, 10 and quality of life.11, 12 Another consideration is fertility after SCI, with an abnormality of the hypothalamic-pituitary-testicular axis having the potential to contribute to abnormalities in spermatogenesis and increased male infertility.13, 14
The studies to date that have addressed the integrity of the hypothalamic-pituitary-testicular axis in people with SCI have generally been performed in relatively small sample sizes.15, 16, 17 Provocative testing of the pituitary with the gonadotropin-releasing hormone (GnRH) has been reported only once in the same cohort with concomitant stimulation of the testes with human chorionic gonadotropin (hCG).16 In prior studies, basal levels of T and the gonadotropins were normal, low or elevated; in subsets of subjects, the pituitary follicular stimulation hormone (FSH) response to provocative stimulation was often exaggerated, and the luteinizing hormone (LH) response was frequently increased. Even in people with SCI who had normal serum levels of gonadotropins, T and estradiol, and in whom testicular responses to hCG were normal, abnormalities were observed to be present in spermatogenesis.2 To further assess the integrity of the hypothalamic-pituitary-testicular axis in a healthy cohort of adult men with SCI, standard clinical provocative testing of the testes and the pituitary was performed.
Materials and methods
Study cohort
Subjects were recruited from the James J Peters VA Medical Center (JJP VAMC), Bronx, NY and the Kessler Institute of Rehabilitation (KIR), West Orange, NJ. Healthy men between the ages of 18 and 65 with chronic SCI (duration of injury >1 year) or healthy men who were neurologically intact (able-bodied (AB)) were considered to be eligible for the study recruitment. The group with SCI was recruited from a convenience sample and found to have approximately half of the SCI participants with serum T concentrations below the normal range (14 hypogonadal) without an apparent etiology for this condition, with the remainder having values in the normal range (16 eugonadal); an effort was made to recruit a similar distribution in the AB group, which was successfully achieved by randomly screening a convenience sample of AB individuals for serum T concentration to permit identification of a sufficient number of AB subjects with low values for enrollment (AB: 18 eugonadal; 20 hypogonadal). Exclusion criteria consisted of the following conditions: acute illness; active thyroid disease; medications for depression, mood changes or any nervous system condition; centrally acting high blood pressure medications (that is, guanethidine, reserpine, methyldopa, β-adrenergic blockers and clonidine); medications for gastrointestinal disorders; medication for heart disease; medications for seizures (that is, dilantin or barbiturates); epilepsy; congestive heart failure; anti-cancer medications; antibiotics; pain medications; hormones (other than replacement doses); history of pituitary or testicular surgery; and/or less than 18 or older than 65 years of age. Abstinence from alcohol-containing beverages was required for 48 h before study procedures. The research study was approved by the Institutional Review Boards of the JJP VAMC and the KIR. Written informed consent was obtained from each subject before study participation.
To assist with characterizing responses to the respective stimulation tests, individual subject responses were categorized as ‘responder’ or ‘non-responder’ to GnRH for LH or FSH. The criteria to be considered as a gonadotropin responder was to attain a greater than two-fold increase in the plasma LH level and a greater than 50% increase in the plasma FSH level from the baseline concentration after GnRH administration,18 with any participant not achieving these threshold levels of gonadotropin release then categorized as a non-responder. Because there were no statistical differences observed for pituitary or testicular responses to provocative testing based on gonadal status (for example, eugonadal or hypogonadal) between SCI or AB groups, subsequent analyses were performed on combined groups. The SCI and control group non-responders were combined into a single group to facilitate statistical analyses. Thus, there were three groups for the LH and FSH responses to provocative stimulation: AB-responder, SCI-responder and non-responder groups. The group designation as ‘responder’ or ‘non-responder’ to GnRH response also was used to categorize participants who underwent hCG stimulation.
Procedures
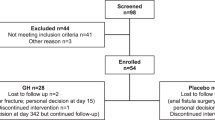
This was a prospective, open-label, randomized and parallel group investigation to differentiate between normal and abnormal pituitary and/or testicular function in people with SCI. Two stimulation tests were performed: one to test pituitary function to the administration of intravenous GnRH (100 μg) to assess the release of gonadotropins (LH, FSH) and the other to test the testicular responsiveness to the administration of intramuscular hCG (4000 IU) to determine the secretion of T. For each stimulation test, serial blood draws permitted a dose–response curve to be obtained. For the hCG (Novarel, Ferring Pharmaceuticals, Parsippany, NJ, USA) stimulation test, each subject completed 3 consecutive days of testing during a 1-week period; hCG was administered intramuscularly on 2 consecutive days, with blood collected for serum T between 0800 and 0900 h before injection, and subjects returned on day 3 when a blood sample was collected (Figure 1a). For the GnRH (Clinafla, Bachem, Bubendorf, Switzerland) stimulation test, an intravenous line was placed in an antecubital vein for serial blood draws in heparinized tubes at time 0, 15, 30 and 60 min following provocative stimulation (Figure 1b). Blood samples were centrifuged; plasma was separated for the determination of plasma LH and FSH using commercial kit assay, and serum was separated for the determination of T using a commercial kit assay. Plasma/serum samples were frozen at −70 °C until batch processing at the completion of all testing.
Schematic representation of each provocative hormone stimulation test and blood draw timeline. hCG was administered on successive visits after a blood sample was obtained on days 1 and 2; a blood sample was performed on day 3 (a). A single administration of GnRH occurred after a baseline blood sample was obtained; successive blood draws were performed in a time-indicated manner (b).
Laboratory analysis
Plasma FSH and LH levels were determined in duplicate by immunoradiometric assay (Siemens Medical Solutions Diagnostics, Los Angeles, CA, USA). The sensitivity for the FSH assay was 0.06 mIU ml−1; the intra-assay coefficients of variation (CV) were 3.8, 2.4 and 3.8% for FSH concentrations of 1.6, 10 and 73 mIU ml−1, respectively; the inter-assay CV were 5.7, 4.0 and 5.0% for FSH concentrations of 4.6, 11 and 38 mIU ml−1, respectively; the 95% range for adult males is 1.1–13.5 mIU ml−1. The sensitivity of the LH assay was 0.15 mIU ml−1; the inter-assay CV were 1.6, 1.2 and 1.0% for LH concentrations of 9, 16 and 22 mIU ml−1, respectively; the inter-assay CV were 7.1, 2.6 and 3.4% for LH concentrations of 2, 9 and 24 mIU ml−1, respectively; the 95% range for adult males is 0.4–5.7 mIU ml−1. The serum levels of T were determined in duplicate by radioimmunoassay, in accordance with the manufacturer’s guidelines (ICN Biomedicals, Inc., Costa Mesa, CA, USA). The sensitivity for T assay was 0.08 ng ml−1; the intra-assay CV were 9.6, 8.1 and 7.8% for T concentrations of 0.9, 7.0 and 20 ng ml−1, respectively; the inter-assay CV were 8.6, 9.1 and 8.4% for T concentrations of 0.7, 6.0 and 16 ng ml−1, respectively; the 2 standard deviation normal range for adult males is 2.8–8.8 ng ml−1.
Statistical analyses
Values are expressed as group mean±s.d. (95% confidence interval, CI). Separate factorial analysis of variance (ANOVA) was performed to identify group differences (SCI compared with control) for demographic (age, height, weight, body mass index and duration of injury) and baseline laboratory values (T, LH and FSH).
To determine whether differences were present in the stimulation test (GnRH: 100 μg; hCG: 4000 IU) and end point (FSH, LH and T) responses between eugonadal and hypogonadal participants, separate two-factor (group: AB, SCI; and gonadal status: hypogonadal, eugonadal) ANOVA tests with repeated measures on time (0, 15, 30 and 60 min) were performed to identify group differences (these data are not shown). Because there were no group differences in the provocative responses between gonadal status groups, our grouping designation was based on the presence or absence of a response to the respective stimulation tests and their end points in AB or SCI participants. Thus, separate single-factor (response group: AB-Responder, SCI-Responder and Non-Responder) mixed model ANOVA with repeated measures on time (0, 15, 30 and 60 min) was performed to identify group differences for the respective stimulation tests (GnRH: 100 μg; hCG: 4000 IU) and end points (FSH, LH and T). To further identify and describe significant main effects in the response to stimulation tests, Bonferroni post hoc tests were applied to the respective time points. For each stimulation test and laboratory outcome, the area under the curve (AUC) was calculated using Graphpad software (Prism 5.0, La Jolla, CA, USA), as the sum of the rise above the baseline value for each time point. Factorial ANOVA was performed to identify the presence of any group differences for AUC in the FSH, LH and T responses to stimulation. An a priori level of significance was set at P⩽0.05. Statistical analyses were completed using IBM SPSS Statistics 21 (IBM, Armonk, NY, USA).
Results
Demographic information and baseline blood values
Demographic data for subjects in the AB and SCI groups are provided (Table 1). The groups were well matched for demographic characteristics. Baseline laboratory values for the group are provided (Table 2). The mean plasma FSH level in the SCI group was higher (P<0.05) than that of the AB group, although the mean values were within normal range for both groups. No other significant differences were observed between the groups for serum LH or T values at baseline.
GnRH provocative stimulation
Provocative testing with GnRH was performed (Figure 1). Significant group (P<0.05), time (P<0.0001) and interaction (P<0.0001) effects were observed for plasma FSH response, indicating that the SCI-responder group had an augmented FSH response compared with the other groups. Bonferroni post hoc tests revealed that the SCI-responder group had a markedly elevated FSH concentration at 15, 30 and 60 min after stimulation compared with the other groups (Figure 2, top panel). The peak FSH response to GnRH was at 60 min in both the SCI- and AB-responder groups. The augmented FSH response to stimulation in the SCI-responder group was confirmed by the AUC (Table 3). Being eugonadal or hypogonadal did not predict those who were responders or non-responders to GnRH stimulation for FSH.
Response of plasma gonadotropin concentration to stimulation by GnRH 100 μg. Data are presented as group mean with standard error bars redacted for enhanced visualization of group responses of the FSH (top panel) and LH (bottom panel) concentrations to provocative stimulation. Significant interaction effects were present for FSH (P<0.0001) and LH (P<0.01). Standard errors of the mean are provided by time (i.e., 0, 15, 30 and 60 min) for each group for plasma FSH concentrations (AB-Responders: 0.26, 0.47, 0.60, 0.55 mIU ml−1; SCI-Responders: 0.76, 1.42, 1.49, 1.83 mIU ml−1; Non-Responders: 0.70, 0.93, 0.95, 0.79 mIU ml−1) and for plasma LH concentrations (AB-Responders: 0.46, 2.32, 2.88, 2.44 mIU ml−1; SCI-Responders: 0.36, 4.23, 3.91, 3.33 mIU ml−1; Non-Responders: 2.51, 3.58, 4.47, 5.04 mIU ml−1). Significant Bonferroni post hoc test comparisons for individual time points: 1AB-Responders vs SCI-Responders P<0.05; 2SCI-Responders vs Non-Responders P<0.05.
Significant time (P<0.0001) and interaction (P<0.01) effects were observed for plasma LH response (Figure 1, bottom panel); group main effects trended toward a significant difference (P=0.09); by definition, both the SCI- and AB-responder groups had an elevated response compared with the non-responder group. At 15 and 30 min after stimulation, the SCI-responder group had significantly elevated LH responses (P<0.05) compared with the non-responder group, but the response was only trending toward a difference compared with the AB-responder group at these time points (Figure 2, bottom panel). The highest concentration after stimulation of LH was observed at 30 min, regardless of group designation. An augmented AUC response of LH to GnRH stimulation approached significance (P=0.06) in the SCI-responder group compared with the AB-responder group (Table 3). Gonadal status did not predict those who were responders or non-responders to GnRH stimulation for LH.
hCG provocative stimulation
Provocative testing with hCG was performed (Figure 3). There was no group or interaction effects to hCG stimulation. Time main effects were observed (P<0.0001) for each group, indicating release of T upon stimulation. In all groups, serum T concentration approximately doubled after stimulation by day 3. All groups had similar increases in serum T concentration to provocative stimulation, and the AUC was not significantly different among the groups (Table 3).
Responses of serum testosterone concentration to stimulation by hCG 4000 IU. Data are presented as group mean with standard error bars redacted for enhanced visualization of group responses for serum testosterone concentrations to provocative stimulation. Standard errors of the mean are provided by time (i.e., days 1, 2 and 3) in each group for serum testosterone concentrations (AB-Responders: 10.4, 17.2, 19.9 nmol l−1; SCI-Responders: 13.4, 20.1, 26.1 nmol l−1; Non-Responders: 12.7, 18.2, 22.9 nmol l−1). Time main effects were present for day of visit, but groups were not statistically different.
Discussion
Primary testicular failure is associated with depressed serum T levels and elevated plasma LH levels. In our study at baseline, mean gonadotropin and testosterone levels were within the normal range, but the mean value for plasma FSH was significantly higher in the SCI group than that in the AB group, albeit the mean FSH value for each group was within the normal range. In the group with SCI, about three-quarters of subjects had a gonadotropin response to pituitary stimulation that was within the normal range, which represents a similar proportion to that observed for the AB group. However, the SCI-responder group had significantly heightened response of FSH at several time points after provocative stimulation compared with that of the AB-responder group. The mean serum plasma LH response in the SCI-responder group and the AUC was higher and approached significance compared with that of the AB-responder group. Thus, conventional clinical interpretation of the heightened central responses to provocative stimulation in subjects with SCI would suggest a mild androgen deficiency state. However, arguing against this conclusion, the gonadotropin responder and non-responder groups with SCI had similar and appropriate increases from baseline values for serum T concentration, which supports normal Leydig cell function. Furthermore, whether a subject with SCI was hypogonadal or eugonadal did not predict as to whether the individual would be a responder or non-responder to pituitary stimulation of gonadotropins. Thus, these findings, taken together, would suggest a central problem related to insufficient hypothalamic drive to pituitary gonadotropin release.
Although basal levels of circulating gonadotropins and T are quite helpful in evaluating static function of the pituitary and testis, provocative stimulation of the hypothalamic-pituitary-gonadal axis has the potential to provide further insight into the integrity of the system. To date, there has been only a single study that has tested both the pituitary and testicular responses to provocative stimulation and that report was quite limited in the number of subjects studied; 18 subjects received gonadotropin-stimulating factor and, of these, only 8 subjects received hCG.16 Almost all other stimulation studies of either the pituitary or the testes were relatively small in sample size and had not attempted to control for possible extraneous factors such as medication or other potentially confounding factors. As such, the work presented herein represents the most rigorously controlled study to date with regard to limiting confounding variables in addressing the effects of chronic SCI per se on the hypothalamic-pituitary-testicular axis in those with normal or reduced serum T concentrations.
Pituitary release of LH regulates steroidogenesis of the Leydig cells of the testis, and FSH simulates the Sertoli cells and gametogenesis. Pituitary release of gonadotropins is under the control of GnRH from the hypothalamus and other factors that may modulate the frequency and/or amplitude of response. Non-aromatized androgens reduce the frequency of LH release, and estrogenic compounds reduce both the frequency and amplitude of release. Opiate administration decreases the frequency and amplitude of LH release, whereas opiate antagonists would have a contrary action. Provocative stimulation by the single intravenous administration of GnRH results in the release of stored gonadotropins from the pituitary gland. The gonadotropin response in normal men generally, but not always, is a several-fold increase in the release of LH above the baseline level that peaks approximately 30 min after intravenous administration of GnRH; and, FSH release is characterized by a more blunted response that peaks somewhat later, at about 45–60 min after provocation. The peak values for FSH and LH observed in our subjects with SCI were appropriate when compared with observations in the general literature.
Whether testosterone deficiency in men with SCI is, in part, central or peripheral in etiology has been a topic of controversy. Studies to date have generally been limited.15 Hayes et al. studied basal and stimulated serum gonadotropin levels in 15 men with SCI; the basal levels of gonadotropins were elevated in about half the subjects, and almost all had elevated FSH and about half had elevated LH responses to provocative stimulation. Morley et al.16 found about one-third of 18 men with SCI to have elevated or abnormal gonadotropin responses despite similar serum T levels to a control group; in a subset of 8 men with SCI, the testicular response to hCG stimulation was adequate. In 30 men with SCI, 8 of whom had an unexplained elevation in serum T levels, Huang et al.17 reported elevated gonadotropin responses to GnRH; approximately half of the SCI subjects had an elevated LH, and 20% had an elevated FSH response to provocative stimulation; of note, all subjects had normal baseline serum LH levels, and one subject had an elevated serum FSH level. Whether the elevated LH response to GnRH testing was a consequence of unresponsiveness of the end organ to pituitary stimulation was not addressed in this report, but a significant correlation was found between total sperm count and serum LH concentration. Provocative stimulation of the testis was found to be normal in five subjects who had normal levels of serum LH, FSH, T and estradiol; testicular biopsies were performed in only two subjects, one of whom had spermatogenic arrest and both had immunological abnormalities of either the seminiferous tubule or the spermatogonia.2
Abnormal function of the pituitary-gonadal axis often has consequences on sexual function, although there is no shortage of other reasons for poor semen quality in people with chronic SCI, including local hyperthermia, medications and infection of the genitourinary tract, among other etiologies.19 Spermatogenesis was reported to be abnormal in about half of the testicular biopsies obtained in men with SCI, and men with normal spermatogenesis had a higher T-to-LH ratio, with no other factors being predictive of histopathology of the testis.20 Naderi et al. studied 55 men with SCI for endocrine profiles, stimulation tests of the pituitary-testicular axis and semen quality.21 Sperm motility and percent normal sperm morphology were lower in those with SCI than in healthy AB controls; basal levels of gonadotropins, LH, FSH, or both, were depressed in 28 subjects, of whom 9 had low levels of serum T; the exaggerated responses of gonadotropins to GnRH were only significant in those subjects with SCI who had basal levels of gonadotropins below the normal range when compared with normal controls.21 Fujisawa et al.22 investigated the GnRH response to 52 men with SCI who had idiopathic oligozoospermia and normal basal levels of serum gonadotropins and T; of note, subjects who had lower sperm concentrations (<10 × 106 per ml) had significantly increased peak levels of gonadotropins than those with high sperm concentrations.
People with SCI have been considered a model of accelerated aging. The associated morbidities in those with SCI include reduced lean tissue mass occurring earlier in life,23, 24 carbohydrate and lipid disorders,25, 26 severe osteoporosis 27 and increased cardiovascular disease.28, 29 Although many of these conditions may be predominantly the result of immobilization, it is conceivable that a reduction in serum T concentration may worsen these clinical end points.
The work presented in this report has limitations. The men studied are representative of a relatively healthy group of individuals with chronic SCI, and therefore do not address central or gonadal function in men with SCI who may have a variety of chronic morbid conditions. Our sample size was not large enough to determine the effect of duration, level or completeness of injury on provoked outcomes; the severity of neurological impairment may be speculated to have an influence on either pituitary responsiveness or testicular health. The nutritional status, alcohol consumption and/or surreptitious drug abuse were not assessed, any one of which may have contributed to the presence of the central dysregulation of hypothalamic–pituitary function. The likelihood for clinically significant malnutrition was low, but excessive alcohol consumption or opioids may have had a role in subsets of our cohort, although the prevalence of alcoholism in veterans with SCI has been reported to be lower than that reported for the general population.30 However, the prevalence of pain is fairly high in the SCI population,31, 32 which may lead to either the prescription or the occult use of narcotics.33, 34, 35 It should be appreciated that every effort was made to exclude individuals with known medical conditions that could have confounded interpretation of the data.
Conclusion
In a healthy cohort of men with chronic SCI, pituitary response to provocative stimulation revealed an augmented FSH response and an LH response that trended higher than the respective AB group. The heightened central response to provocative stimulation in healthy people with chronic SCI would suggest a mild androgen deficiency state. However, the testicular response to provocative stimulation was similar in both responders and non-responders with SCI, and the increase in serum testosterone concentration was of normal magnitude, regardless of group designation; thus, testicular function appears to be without deficit. As such, the likelihood of a reduction in hypothalamic drive to the pituitary gonadotropins should be considered. The possibility exists that a more graded provocative stimulation of the pituitary or the testes may have greater sensitivity to reveal a deficit in the function of one or both of these glands
DATA ARCHIVING
There were no data to deposit.
References
Ver Voort SM . Infertility in spinal-cord injured male. Urology 1987; 29: 157–165.
Kikuchi TA, Skowsky WR, El-Toraei I, Swerdloff R . The pituitary-gonadal axis in spinal cord injury. Fertil Steril 1976; 27: 1142–1145.
Bauman WA, La Fountaine MF, Spungen AM . Age-related prevalence of low testosterone in men with spinal cord injury. J Spinal Cord Med 2014; 37: 32–39.
Kelly DM, Jones TH . Testosterone: a metabolic hormone in health and disease. J Endocrinol 2013; 217: R25–R45.
De Maddalena C, Vodo S, Petroni A, Aloisi AM . Impact of testosterone on body fat composition. J Cell Physiol 2012; 227: 3744–3748.
Zitzmann M . Effects of testosterone replacement and its pharmacogenetics on physical performance and metabolism. Asian J Androl 2008; 10: 364–372.
Bauman WA, Cirnigliaro CM, La Fountaine MF, Jensen AM, Wecht JM, Kirshblum SC et al. A small-scale clinical trial to determine the safety and efficacy of testosterone replacement therapy in hypogonadal men with spinal cord injury. Horm Metab Res 2011; 43: 574–579.
Cattabiani C, Basaria S, Ceda GP, Luci M, Vignali A, Lauretani F et al. Relationship between testosterone deficiency and cardiovascular risk and mortality in adult men. J Endocrinol Invest 2012; 35: 104–120.
Hyde Z, Norman PE, Flicker L, Hankey GJ, Almeida OP, McCaul KA et al. Low free testosterone predicts mortality from cardiovascular disease but not other causes: the Health in Men Study. J Clin Endocrinol Metab 2012; 97: 179–189.
Makinen J, Jarvisalo MJ, Pollanen P, Perheentupa A, Irjala K, Koskenvuo M et al. Increased carotid atherosclerosis in andropausal middle-aged men. J Am Coll Cardiol 2005; 45: 1603–1608.
Yassin DJ, Doros G, Hammerer PG, Yassin AA . Long-term testosterone treatment in elderly men with hypogonadism and erectile dysfunction reduces obesity parameters and improves metabolic syndrome and health-related quality of life. J Sex Med 2014; 11: 1567–1576.
Aydogan U, Aydogdu A, Akbulut H, Sonmez A, Yuksel S, Basaran Y et al. Increased frequency of anxiety, depression, quality of life and sexual life in young hypogonadotropic hypogonadal males and impacts of testosterone replacement therapy on these conditions. Endocr J 2012; 59: 1099–1105.
Talebi AR, Khalili MA, Vahidi S, Ghasemzadeh J, Tabibnejad N . Sperm chromatin condensation, DNA integrity, and apoptosis in men with spinal cord injury. J Spinal Cord Med 2013; 36: 140–146.
Qiu Y, Wang LG, Zhang LH, Zhang AD, Wang ZY . Quality of sperm obtained by penile vibratory stimulation and percutaneous vasal sperm aspiration in men with spinal cord injury. J Androl 2012; 33: 1036–1046.
Hayes PJ, Krishnan KR, Diver MJ, Hipkin LJ, Davis JC . Testicular endocrine function in paraplegic men. Clin Endocrinol (Oxf) 1979; 11: 549–552.
Morley JE, Distiller LA, Lissoos I, Lipschitz R, Kay G, Searle DL et al. Testicular function in patients with spinal cord damage. Horm Metab Res 1979; 11: 679–682.
Huang TS, Wang YH, Chiang HS, Lien YN . Pituitary-testicular and pituitary-thyroid axes in spinal cord-injured males. Metabolism 1993; 42: 516–521.
Bhasin S, Jameson JL Disorders of the testes and male reproductive system. In: Braunwald E, Anthony SF, Stephen LH, Kasper DL, Jameson JL, Longo DL (eds). Harrison's Principles of Internal Medicine: New York. 2005, p 2188.
Linsenmeyer TA . Male infertility following spinal cord injury. J Am Paraplegia Soc 1991; 14: 116–121.
Elliott SP, Orejuela F, Hirsch IH, Lipshultz LI, Lamb DJ, Kim ED . Testis biopsy findings in the spinal cord injured patient. J Urol 2000; 163: 792–795.
Naderi AR, Safarinejad MR . Endocrine profiles and semen quality in spinal cord injured men. Clin Endocrinol (Oxf) 2003; 58: 177–184.
Fujisawa M, Kanzaki M, Hayashi A, Tanaka H, Okada H, Arakawa S et al. Alteration of the hypothalamus-pituitary-testis axis in oligozoospermic men with normal gonadotropin levels. Int J Urol 1995; 2: 273–276.
Spungen AM, Adkins RH, Stewart CA, Wang J, Pierson RN Jr, Waters RL et al. Factors influencing body composition in persons with spinal cord injury: a cross-sectional study. J Appl Physiol 2003; 95: 2398–2407.
Spungen AM, Wang J, Pierson RN Jr, Bauman WA . Soft tissue body composition differences in monozygotic twins discordant for spinal cord injury. J Appl Physiol 2000; 88: 1310–1315.
Bauman WA, Adkins RH, Spungen AM, Kemp BJ, Waters RL . The effect of residual neurological deficit on serum lipoproteins in individuals with chronic spinal cord injury. Spinal Cord 1998; 36: 13–17.
Bauman WA, Spungen AM . Body composition in aging: adverse changes in able-bodied persons and in those with spinal cord injury. Top Spinal Cord Inj Rehabil 2001; 6: 22–36.
Bauman WA, Cardozo CP . Osteoporosis in individuals with spinal cord injury. PMR 2015; 7: 188–201.
Wahman K, Nash MS, Lewis JE, Seiger A, Levi R . Increased cardiovascular disease risk in Swedish persons with paraplegia: The Stockholm spinal cord injury study. J Rehabil Med 2010; 42: 489–492.
Cragg JJ, Noonan VK, Dvorak M, Krassioukov A, Mancini GB, Borisoff JF . Spinal cord injury and type 2 diabetes: Results from a population health survey. Neurology 2013; 81: 1864–1868.
Kirubakaran VR, Kumar VN, Powell BJ, Tyler AJ, Armatas PJ . Survey of alcohol and drug misuse in spinal cord injured veterans. J Stud Alcohol 1986; 47: 223–227.
Dijkers M, Bryce T, Zanca J . Prevalence of chronic pain after traumatic spinal cord injury: a systematic review. J Rehabil Res Dev 2009; 46: 13–29.
van Gorp S, Kessels AG, Joosten EA, van Kleef M, Patijn J . Pain prevalence and its determinants after spinal cord injury: a systematic review. Eur J Pain 2015; 19: 5–14.
Norrbrink C, Lundeberg T . Tramadol in neuropathic pain after spinal cord injury: a randomized, double-blind, placebo-controlled trial. Clin J Pain 2009; 25: 177–184.
Attal N, Guirimand F, Brasseur L, Gaude V, Chauvin M, Bouhassira D . Effects of IV morphine in central pain: a randomized placebo-controlled study. Neurology 2002; 58: 554–563.
Heinemann AW, Doll MD, Armstrong KJ, Schnoll S, Yarkony GM . Substance use and receipt of treatment by persons with long-term spinal cord injuries. Arch Phys Med Rehabil 1991; 72: 482–487.
Acknowledgements
We thank the James J Peters VA Medical Center, Bronx, NY, the Department of Veterans Affairs Rehabilitation Research and Development Service and the Kessler Institute for Rehabilitation, West Orange, NJ, for their support. This work was funded by the Veteran Affairs Rehabilitation Research and Development National Center of Excellence for the Medical Consequences of Spinal Cord Injury (#B2648-C, #B4162-C and #B9212-C).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Bauman, W., La Fountaine, M., Cirnigliaro, C. et al. Provocative stimulation of the hypothalamic–pituitary–testicular axis in men with spinal cord injury. Spinal Cord 54, 961–966 (2016). https://doi.org/10.1038/sc.2016.50
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2016.50
This article is cited by
-
Can the positive association of osteocalcin with testosterone be unmasked when the preeminent hypothalamic–pituitary regulation of testosterone production is impaired? The model of spinal cord injury
Journal of Endocrinological Investigation (2019)
-
Administration of increasing doses of gonadotropin-releasing hormone in men with spinal cord injury to investigate dysfunction of the hypothalamic–pituitary–gonadal axis
Spinal Cord (2018)
-
Testicular responses to hCG stimulation at varying doses in men with spinal cord injury
Spinal Cord (2017)
-
Musculoskeletal Health in the Context of Spinal Cord Injury
Current Osteoporosis Reports (2017)