Abstract
Study design:
Self-reported survey.
Objective:
Our purpose was to identify the predictors of pain medication misuse (PMM) among participants with spinal cord injury (SCI).
Setting:
A medical university in the southeastern United States.
Methods:
A total of 919 adults with impairment from traumatic SCI of at least 1-year duration, who reported at least one painful condition and were taking prescription medication to treat pain, were included in this study. PMM was measured by the Pain Medication Questionnaire (PMQ).
Results:
The average PMQ score was 19.7, with 25.8% of participants scoring at or above the cutoff of 25, which is indicative of PMM. A three-stage logistic regression analysis was conducted by sequentially adding three sets of predictors to the equation: (1) demographic and injury characteristics; (2) pain characteristics and (3) frequency of pain medication use. Age and education level were protective of PMM, whereas pain intensity, pain interference and pain medication use were risk factors. Number of painful days was not significant in the final model.
Conclusion:
PMM must be of concern after SCI, given its high prevalence among those with at least one painful condition and its relationship with pain indicators.
Similar content being viewed by others
Introduction
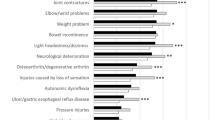
Traumatic spinal cord injury (SCI) is associated with high incidence of secondary health conditions, including pain. The prevalence rates of pain in SCI are difficult to estimate, with reports of severe pain ranging widely from 18 to 63%.1, 2 Pain severity among those with SCI is higher than established norms in the general population.3 Experiencing pain is associated with lower self-rated global health, community reintegration and quality of life, as well as poorer mental health and quality of sleep.4, 5, 6, 7
Pain medication misuse (PMM) is an important issue to consider, given the high levels of pain intensity, significant effects of pain outcomes on the quality of life, and the increasing incidence of poisoning deaths related to unintentional pain medication overdose in the general population in the USA.8 Prevalence estimates and individual characteristics associated with PMM and abuse have been examined in noncancer chronic pain samples; however, research is lacking in the SCI population. Findings from a large, non-SCI sample have suggested that age is inversely related to the risk of PMM, and the diagnosis of two or more mental health disorders or a substance abuse diagnosis was found to increase the risk of misuse.9 Similar findings have been reported in studies examining predictors of opioid medication misuse in patients with chronic pain.10 Being white, male, smoking cigarettes, reporting greater pain-related limitations and reporting greater subjective pain intensity ratings have been associated with higher risk for PMM.11, 12
We were able to identify only one study examining prescription medication misuse in individuals with SCI. This study, published in 1992, used only 96 participants and focused more broadly on a variety of psychotropic medications. Results indicated that, of the 43% reporting recent prescription medication use, 24% reported misuse characterized by using more than the prescribed dose or using without a prescription. Significant differences in depressive symptoms or acceptance of disability were not found between individuals who used prescription medications as prescribed and those who misused.13
Purpose
Our purpose was to identify: (a) the prevalence of PMM and (b) the relationship of PMM with pain indicators among participants with SCI who have at least one painful condition. A multistage, logistic modeling approach was used to identify the predictors of PMM as related to demographic and injury characteristics, pain characteristics and frequency of pain medication use.
Materials and methods
Participants
Institutional Review Board approval was obtained before study initiation. We also obtained a certificate of confidentiality that protects identifiable research information from forced disclosure in any civil, criminal, administrative, legislative or other proceeding, whether at the federal, state or local level. Participants were identified from records of a large specialty hospital in the southeastern United States. All participants (1) were adults, (2) were a minimum of 1 year after traumatic SCI and (3) had some residual impairment. There were 3154 potential participants in the preliminary pool, including 575 confirmed deceased cases. Of the remaining 2558, usable materials were returned by 1689 (66%). There were 400 nonrespondents, and 469 were lost to follow-up (either their materials were returned undeliverable, or we could not confirm their address by phone). The adjusted response rate among those who were successfully contacted was 81%.
Additional eligibility criteria required were added to eliminate those who either did not report at least one painful condition or used at least some prescription medication for pain. A total of 1023 participants met these selection criteria, 919 of whom completed all items of the pain medication questionnaire (PMQ)14 and were retained for analyses (Figure 1).
Procedures
Before sending actual materials, preliminary cover letters were sent to potential participants to describe the study and alert them that materials would be forthcoming in 4–6 weeks. Up to three mailings and a follow-up phone call were used to encourage participation. Participants received $50 remuneration.
Measures
Prescription pain medication use was measured by asking participants the frequency with which they used prescribed pain medications in the past 12 months with the following response options: (a) never, (b) sometimes, (c) weekly or (d) daily.15, 16, 17
Pain experience within the past 30 days was assessed using the following self-report item, taken from the Behavioral Risk Factor Surveillance System questionnaire: ‘During the past 30 days, about how many days did pain make it hard for you to do your usual activities, such as self-care, work, or recreation?’18 Self-report items from the Brief Pain Inventory were used to assess pain intensity and interference of pain on functioning.19 Average pain intensity was measured by asking participants to describe the pain they experienced on average by rating their pain from 0 to 10, with 0 being ‘no pain’ and 10 being ‘pain as bad as you can imagine’. The second Brief Pain Inventory item, the extent of interference of pain on mood and functional activity, asked participants to rate their pain interference on a scale from 0 to 10, with 0 being ‘does not interfere’ and 10 being ‘completely interferes,’ with the following activities in the past week: (a) general activity, (b) mood, (c) walking ability, (d) normal work, (e) relation with others, (f) sleep and (g) enjoyment of life. The average pain interference score was calculated for individuals who answered over half of the items.20
PMM was measured using the PMQ.14 The PMQ consists of 26 self-report items arranged in a 5-point Likert format intended to assess the risk for PMM in individuals with a variety of pain syndromes. Items that are examples of PMM include the following: ‘At times, I need to take pain medication more often than it is prescribed in order to relieve my pain’ and ‘I get pain medication from more than one doctor in order to have enough medication for my pain’. Response options indicate the degree of agreement to or behavioral conformity to each item and are scored from 0–4. Possible total scores range from 0–104, with a higher overall score indicating greater risk of PMM. A cutoff score of 25 or greater has been proposed as reflecting medication use behaviors predictive of problematic use and has been used to differentiate between low-scoring and high-scoring individuals.21 Preliminary analysis of the reliability of the PMQ has shown moderate but acceptable reliability coefficients, and, based on construct and concurrent validity correlations, higher PMQ scores were associated with history of substance abuse, higher levels of psychosocial distress and poorer functioning.14, 22
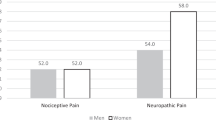
Demographic variables included sex (male, female), race/ethnicity (white, non-Hispanic; black, non-Hispanic; other), age and years since injury. Injury severity was categorized as follows: C1–C4, nonambulatory; C5–C8, nonambulatory; noncervical, nonambulatory; and ambulatory (regardless of level). Ambulatory status is used as a self-report proxy measure for the ASIA (American Spinal Injury Association) Impairment Scale D, and classification of injury severity using a combination of injury level and ambulatory status/ASIA Impairment Scale D has been widely reported in the literature.23, 24 Cause of injury was dichotomized as violent and nonviolent. Education was categorized as less than high school, high school diploma or some college education, 4-year college degree or higher. Annual household income was measured and grouped as <$25 000, $25 000–74 999 and $75 000+.
Data analysis
SPSS 21 (IBM Corp., Armonk, NY, USA) was used for all data analyses. Descriptive statistics were calculated for participant demographic information, injury characteristics, medication use and pain experiences.
To evaluate selective attrition, we compared respondents and those who did not respond (deceased, lost or refusal) on biographic and injury characteristics using the chi-square statistic for categorical variables (sex, race/ethnicity, education, income, cause of injury and injury severity) and the independent sample t-test for metric variables (age at injury, years post injury and chronological age). Data on demographic and injury characteristics were available only on a subsample of those who did not respond.
Bivariate analyses used t-tests and the chi-square statistic to identify the association of demographic, injury, pain variables and frequency of pain medication use as a function of PMM based on a cutoff score of 25 or greater. Pearson's correlation coefficients were used to examine relationships between PMQ score, pain indicators and frequency of pain medication use.
Logistic regression was used to identify predictors of PMM. A three-stage analysis using the enter method and simple coding to compare categorical variables was used. Demographic and injury characteristics were entered in the first stage as statistical controls, followed by three pain-related conditions including the following: (a) pain experience in the past 30 days; (b) average pain intensity and (c) pain interference. Frequency of pain medication use was entered in the final stage and thus the association of this variable with the risk of PMM could be assessed after consideration of all other factors. The three-stage procedure, therefore, allowed us to identify the importance of each set of factors, with the introduction of additional predictors.
Statement of ethics
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
Selective attrition
There were no differences between respondents and nonrespondents with respect to chronological age, sex, race-ethnicity, age at injury or cause of injury (Table 1). Respondents had more education, higher income, a greater number of years post injury and less severe injuries (that is, more likely to be ambulatory).
Descriptive
The majority of the sample used pain medication daily (63.1%), followed by sometimes (28.4%) and weekly (8.5%) (Table 2). Just fewer than 26% of the participants had PMQ scores indicative of PMM. The reliability of the PMQ scale was acceptable (r=0.74).
Bivariate comparisons
Bivariate comparisons indicated several variables significantly related to PMM (Table 2). Participants meeting cutoff criteria for PMM reported a greater number of days experiencing pain in the past 30 days (t911=–7.93; P⩽0.001), higher average pain intensity (t907=−9.87; P⩽0.001) and more interference from pain (t906=−11.71; P⩽0.001). Of participants reporting scores above the cutoff for PMM, 79.3% used pain medication daily compared with 57.5% of those below the cutoff for medication misuse (χ22= 46.07; P⩽0.001).
Significant bivariate correlations were found between PMQ total score and pain in the past 30 days (+0.33), average pain intensity (+0.37) and pain interference on daily activities (+0.45) (Table 3).
Logistic regression
Odds ratios (OR) and confidence intervals (CIs) for the three-stage analysis are presented in Table 4. In stage 1, PMM was associated with current age, education and income. Those who were younger were more likely to report PMM. Individuals with less education and less annual income were more likely to report PMM. Compared with those with a 4-year college degree, individuals with <12 years of education had 3.43 greater odds (95% CI=1.90–6.21) and those with 12–15 years of education had 2.17 greater odds of reporting PMM (95% CI=1.37–3.42). Compared with those whose annual income was >$75 000, individuals with an annual income <$25 000 had 1.67 greater odds of reporting PMM.
After the addition of the pain indicators, age and education were still significantly associated with PMM. Income was no longer significant. Two pain indicators were significantly related to PMM: average pain intensity and pain interference on daily activities. Those reporting a higher average pain intensity and greater pain interference were more likely to report PMM. For every point increase in average pain intensity, there was a 16% (OR=1.16; 95% CI=1.05–1.29) increase in the odds of PMM. Similarly, for every point increase in pain interference, there was a 26% (OR=1.26; 95% CI=1.15–1.37) increase in the odds of PMM.
In the final stage, frequency of pain medication use was significantly predictive of PMM. Age, education, average pain intensity and pain interference remained significant in the final stage. However, the odds for education decreased substantially to 2.13 (95% CI=1.12–4.06) for those with less than a high school degree and 1.80 (95% CI=1.10–2.95) for those with a high school degree or some college education.
Discussion
The findings suggest the prevalence of PMM is strongly indicated in SCI participants, as nearly 26% of those who reported a minimum of one painful condition met the cut-off for PMM. Adjusting for those who did not have painful conditions and did not take prescription medication for pain would reduce the prevalence to 16% for the full cohort. Given the increasing frequency of deaths due to poisoning within the general population in the USA,8 largely owing to overuse of pain medications, the consequences of pain medication abuse are potentially catastrophic.
The prevalence of PMM within our sample is within the range presented in the noncancer, chronic pain patients and consistent with the prevalence presented within a SCI sample.9, 13, 25, 26 In non-SCI samples, age has been found to be inversely related to and predictive of PMM, which is consistent with the findings presented in the current study.9, 10 Education was found to be a significant predictor, with individuals without a high school diploma and those with a high school diploma or some college education being more likely to meet PMM criteria than those with a 4-year college degree or higher, respectively. This finding is inconsistent with the literature on non-SCI samples that have not supported education as a significant predictor of PMM.25
Our findings also indicate a greater risk for PMM with increased average pain intensity and greater reported limitations in daily activities owing to pain. These findings are consistent with the literature on non-SCI, chronic pain patients.11, 12
Similar to findings in the general population,9 our results indicated that more frequent use of pain medication was associated with greater risk of misuse. Specifically, individuals taking pain medication weekly and daily were 2.5 and 3 times more likely than those who infrequently use pain medication to report PMM, respectively.
Study limitations
All data were self-reported and subject to reporting bias. Because the information requested is sensitive (that is, medication abuse), there is the possibility of underreporting. We attempted to limit response bias by using standardized and validated measures. Furthermore, within the consent procedure, all participants were notified that the study was covered by an NIH certificate of confidentiality, and thus participant responses cannot be disclosed in civil or criminal litigation.
Second, although the response rates were relatively high (66% of all those potentially alive and 81% of those who could be definitively contacted), there is always a concern of selective attrition. However, our comparisons of respondents and nonrespondents indicated limited selective attrition related to education, income, injury severity and time since injury. The first three of these characteristics have consistently been associated with mortality rates, and a substantial number of individuals were deceased (n=575).27
Third, we do not have data on the specific types of pain medications used and potentially misused. Also, other factors, such as a history of substance abuse and mental health factors would likely relate to pain medication misuse but were not a focus of this study. Nevertheless, the strength of the relationship between pain medication use and PMM is of clear clinical significance.
Last, the participant cohort was identified from a clinical setting and therefore, like the vast majority of SCI research (including that coming from the SCI Model Systems within the USA), is not population-based. Those who do not receive primary rehabilitative services after their injuries may potentially be at greater risk for poor outcomes, including PMM.
Clinical implications
It is important that physicians and other healthcare professionals carefully assess PMM, given the high rates of pain medications combined with the high prevalence rates for pain after SCI. A guiding principle is to be conservative when making pain medication prescriptions owing to the high prevalence of PMM after SCI and the elevated risk of mortality. On the other hand, failure to accurately assess and treat pain may inadvertently result in increased PMM as individuals seek alternatives to reduce consequences of pain. These alternatives may be illicit drugs that are not professionally managed or that may have other even more dangerous issues related to purity and dosage. Alternative therapies should be considered, and pain management strategies need to be implemented. It is also important to perform assessments of PMM whenever possible and involve psychologists within the assessment process.
Future research
Additional research should investigate specific types of pain medications in relation to PMM and pain outcomes among those with SCI. Determining the psychological factors related to pain medication use, including substance abuse and mental health, is also of great importance, and thus we can understand the risk profiles of those most likely to abuse pain medications and implement appropriate preventative and clinical strategies. It will be important to identify whether specific medications are more highly related to PMM, and which medications. Last, as always, research is needed on the effectiveness of interventions to either prevent or treat PMM.
Conclusion
PMM occurs in more than one in four persons with SCI who have at least one painful condition and take prescription medications to treat pain. PMM is highest among those of younger ages, those with less education, elevated pain parameters and with higher use of pain medications.
Data archiving
There were no data to deposit.
References
Ehde DM, Jensen MP, Engel JM, Turner JA, Hoffman AJ, Cardenas DD . Chronic pain secondary to disability: a review. Clin J Pain 2003; 19: 3–17.
Rintala DH, Hart KA, Priebe MM . Predicting consistency of pain over a 10-year period in persons with spinal cord injury. J Rehabil Res Dev 2004; 41: 75–88.
Jensen MP, Hoffman AJ, Cardenas DD . Chronic pain in individuals with spinal cord injury: a survey and longitudinal study. Spinal Cord 2005; 43: 704–712.
Siddall PJ, McClelland JM, Rutkowski SB, Cousins MJ . A longitudinal study of the prevalence and characteristics of pain in the first 5 years following spinal cord injury. Pain 2003; 103: 249–257.
Donnelly C, Eng JJ . Pain following spinal cord injury: the impact on community reintergration. Spinal Cord 2005; 43: 278–282.
Putzke JD, Richards JS, Dowler RN . The impact of pain in spinal cord injury: a case–control study. Rehabil Psychol 2000; 45: 386–401.
Norrbrink Budh C, Hultling C, Lundeberg T . Quality of sleep in individuals with spinal cord injury: a comparison between patients with and without pain. Spinal Cord 2005; 43: 85–95.
Paulozzi LJ, Jones CM, Mack KA, Rudd RA . Vital signs: overdoses of prescription opioid pain relievers — United States, 1999–2008. MMWR Morb Mortal Wkly Rep 2011; 60: 1477–1509.
Sullivan MD, Edlund MJ, Fan MY, Devries A, Brennan Braden J, Martin BC . Risks for possible and probable opioid misuse among recipients of chronic opioid therapy in commercial and medicaid insurance plans: The TROUP Study. Pain 2010; 150: 332–339.
Ives TJ, Chelminski PR, Hammett-Stabler CA, Malone RM, Perhac JS, Potisek NM et al. Predictors of opioid misuse in patients with chronic pain: a prospective cohort study. BMC Health Serv Res 2006; 6: 46.
Liebschutz JM, Saitz R, Weiss RD, Averbuch T, Schwartz S, Meltzer EC et al. Clinical factors associated with prescription drug use disorder in urban primary care patients with chronic pain. J Pain 2010; 11: 1047–1055.
Jamison RN, Link CL, Marceau LD . Do pain patients at high risk for substance misuse experience more pain? A longitudinal outcomes study. Pain Med 2009; 10: 1084–1094.
Heinemann AW, McGraw TE, Brandt MJ, Roth E, Dell'Oliver C . Prescription medication misuse among persons with spinal cord injuries. Int J Addict 1992; 27: 301–316.
Adams LL, Gatchel RJ, Robinson RC, Polatin P, Gajraj N, Deschner M et al. Development of a self-report screening instrument for assessing potential opioid medication misuse in chronic pain patients. J Pain Symptom Manage 2004; 27: 440–459.
Krause JS, Carter RE, Pickelsimer E . Behavioral risk factors of mortality after spinal cord injury. Arch Phys Med Rehabil 2009; 90: 95–101.
Krause JS, Zhai Y, Saunders LL, Carter RE . Risk of mortality after spinal cord injury: an 8-year prospective study. Arch Phys Med Rehabil 2009; 90: 1708–1715.
Kohout RK, Saunders LL, Krause JS . The relationship between prescription medication use and ability to ambulate distances after spinal cord injury. Arch Phys Med Rehabil 2011; 92: 1246–1249.
CDC. Behavioral Risk Factor Surveillance System 2010 [cited 2012 August 22]. Available from http://www.cdc.gov/brfss/questionnaires/pdf-ques/2010brfss.pdf.
Cleeland CS, Ryan KM . Pain assessment: global use of the brief pain inVentory. Ann Acad Med Singapore 1994; 23: 129–138.
Cleeland CS The Brief Pain Inventory: User Guide 2009. Available from http://www.mdanderson.org/education-and-research/departments-programs-and-labs/departments-and-divisions/symptom-research/symptom-assessment-tools/BPI_UserGuide.pdf.
Dowling LS, Gatchel RJ, Adams LL, Stowell AW, Bernstein D . An evaluation of the predictive validity of the Pain Medication Questionnaire with a heterogeneous group of patients with chronic pain. J Opioid Manag 2007; 3: 257–266.
Holmes CP, Gatchel RJ, Adams LL, Stowell AW, Hatten A, Noe C et al. An opioid screening instrument: long-term evaluation of the utility of the Pain Medication Questionnaire. Pain Pract 2006; 6: 74–88.
Saunders LL, Krause JS, Acuna J . Association of race, socioeconomic status, and health care access with pressure ulcers after spinal cord injury. Arch Phys Med Rehabil 2012; 93: 972–977.
Saunders LL, Krause JS, Selassie AW . Association of health services with secondary conditions: use of a population-based cohort of persons with SCI in South Carolina. Top Spinal Cord Inj Rehabil 2010; 16: 30–39.
Morasco BJ, Dobscha SK . Prescription medication misuse and substance use disorder in VA primary care patients with chronic pain. Gen Hosp Psychiatry 2008; 30: 93–99.
Edlund MJ, Martin BC, Fan MY, Devries A, Braden JB, Sullivan MD . Risks for opioid abuse and dependence among recipients of chronic opioid therapy: results from the TROUP study. Drug Alcohol Depend 2010; 112: 90–98.
Krause JS, Saunders LL, Acuna J . Gainful employment and risk of mortality after spinal cord injury: effects beyond that of demographic, injury and socioeconomic factors. Spinal Cord 2012; 50: 784–788.
Acknowledgements
The contents of this publication are developed under a grant from the Department of Education, NIDRR grant numbers H133B090005 and H133G090059. However, those contents do not necessarily represent the policy of the Department of Education, and endorsement by the Federal Government should not be assumed. We thank the following individuals who contributed to the work reported in the manuscript: Richard Aust, Josh Acuna, Dr. Yue Cao, Jennifer Coker, Alex Jackson, Melinda Jarnecke, Kristian Manley, Karla Reed and D’Andra Roper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Krause, J., Clark, J. & Saunders, L. Pain medication misuse among participants with spinal cord injury. Spinal Cord 53, 630–635 (2015). https://doi.org/10.1038/sc.2015.42
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2015.42
This article is cited by
-
Employment status, hours working, and gainful earnings after spinal cord injury: relationship with pain, prescription medications for pain, and nonprescription opioid use
Spinal Cord (2020)
-
Cross-cultural adaptation of the Pain Medication Questionnaire for use in Brazil
BMC Medical Research Methodology (2019)
-
Rasch measurement properties of the Pain Medication Questionnaire in persons with spinal cord injury
Spinal Cord (2017)