Abstract
Study design:
Prospective open cohort case series.
Objectives:
To identify opportunities for improvement by recording duration of key processes from acute hospital admission until spinal rehabilitation unit (SRU) admission.
Setting:
SRU, Victoria, Australia.
Methods:
Consecutive referrals of patients with recent spinal cord damage had prospective documentation of the key clinical and demographic characteristics and duration (days) of the following sequential discrete processes: acute hospital admission until referral to SRU, referral until SRU assessment, SRU assessment until ready for transfer to SRU and ready for transfer until SRU admission.
Results:
A total of 347 patients were referred with median age (interquartile range (IQR)) of 65 (52–76) years. Most patients were male (n=203, 58.5%), had paraplegia (n=267, 77%) and an aetiology due to spinal cord myelopathy (n=280, 80.7%). There was a median of 12 days (IQR 6–20) from acute hospital admission until referral, a median of 1 day (IQR 0–2) from referral till assessment, a median of 0 (IQR 0–3.5) days from assessment till deemed ready and a median of 7 (IQR 2–20) days from deemed ready until transfer to SRU. Overall, patients spent 34.2% (4951/14 478 days) of their acute hospital length of stay waiting for a SRU bed.
Conclusions:
There are opportunities to improve the efficiency of the acute hospital journey for patients referred to a SRU. The biggest opportunities exist for reducing the time from acute hospital admission till referral to SRU and the time from deemed ready for transfer to SRU till admission.
Similar content being viewed by others
Introduction
Problems with patient flow have been well described in emergency departments1 and acute care hospitals2, 3 in many countries. It is likely that this challenge will intensify with population ageing4 and the anticipated increase in chronic disease and disability. There has been relatively little attention given to barriers for acute hospital patients waiting for inpatient rehabilitation,5, 6, 7, 8, 9 or the occurrence and causes of discharge barriers for rehabilitation patients remaining in hospital after they are deemed to no longer require inpatient rehabilitation for management of the activity limitations resulting from their impairment.8, 10 The occurrence of these barriers has an adverse impact ‘upstream’—with flow-on affects reducing acute hospital bed availability and increasing the risk of adverse outcomes for patients, such as iatrogenic11 or impairment-related complications.5, 12
Spinal cord damage (SCD), either traumatic spinal cord injury (SCI) or non-traumatic spinal cord myelopathy (SCM) require optimal care from the onset in order to prevent secondary complications that can have a detrimental influence on long-term outcomes. A review of the evidence regarding setting of care for patients with SCD has highlighted that patients have improved outcomes with a specialized and systematic approach to their care, in comparison with less specialized and less coordinated models of care.12 The benefits of a specialised and integrated system of care include reduced complications, length of stay (LOS) in hospital, costs and improved efficiency of rehabilitation in reducing disability.12, 13 There has been very little formal study of the process barriers for patients with SCD needing admission to a spinal rehabilitation unit (SRU), although a number of studies have highlighted this as a problem area5, 6, 14, 15 and this has recently been highlighted as an international problem.16
The primary objective of this study was to measure the time taken for the key processes in the patient journey for patients with SCD from acute hospital admission through to inpatient SRU admission in order to identify opportunities for improvement. In addition, as an exploratory analysis, secondary objectives were to test hypotheses regarding whether clinical or demographic factors contributed to three key outcomes: (1) the delay from acute hospital admission until referral to SRU, (2) the delay between being deemed ready for transfer to SRU and subsequent admission SRU and (3) to determine whether the time waiting for a SRU bed after being deemed ready for transfer was associated with either an increased LOS in SRU, pelvic pressure ulcer or an increased dependency at discharge from rehabilitation.
Materials and methods
Setting
The SRU at the Caulfield Hospital, Victoria, Australia is a 12-bed adult inpatient unit. It is located in a public hospital and funded by the State. Patients with SCD are referred from both private and public hospitals from greater metropolitan Melbourne and elsewhere in the State. Many patients are admitted from the acute care tertiary hospital in the inner-south of metropolitan Melbourne that is part of the same Network as the SRU. As the other major SRU in Melbourne does not routinely admit patients with SCM, the SRU at Caulfield hospital admits mainly these patients; however, it has no specific aetiology bias in its’ admission criteria.
The typical hospital journey for patients involves them being referred by the treating acute hospital unit to the SRU via a central access unit at Caulfield Hospital. The patient would then be assessed by either an advanced trainee in rehabilitation medicine or the unit head (the author—a physician in rehabilitation medicine who specialises in SCD). Patients referred from hospitals in other health networks were typically assessed by the rehabilitation assessment service based at that hospital and subsequently by the advanced trainee in rehabilitation medicine in the SRU, who would confer with the unit head. If the patient was deemed by the SRU to be appropriate and ready for admission, they would be put on a waiting list for admission with the central access unit, which coordinated the timing of admission as beds became available.
Study design
This was a prospective open cohort case series of consecutive referrals of patients with SCD to the SRU between 1 September 2006 and 31 July 2013.
Participants
All patients with a recent onset of SCD who were referred and accepted for admission into the SRU were included in the study. Patients with a chronic SCD readmitted to hospital for management of late-onset complications after a previous rehabilitation admission were excluded.
Outcome measures
Relevant dates were collected to calculate the duration (in days) of the sequential discrete processes that patients passed through from acute hospital admission until transfer into the SRU. If the onset of SCD occurred after the acute hospital admission—for example, in cases of SCM due to spinal cord infarction from aortic aneurysm surgery—then the date of onset of SCD was used instead of the date of acute hospital admission. The key processes recorded were as follows: acute hospital admission (or onset if after) until referral to SRU, referral until assessment by the SRU, assessment by SRU until deemed ready for transfer to rehabilitation and ready for transfer until SRU admission. These processes are based on previous research in this area.17, 18 If a patient was deemed ready for transfer to the SRU and became unwell—for example, due to medical complications—then the ‘not ready’ duration was excluded from calculating the duration waiting for transfer. Patients referred and accepted for admission into the SRU, but not subsequently admitted, had the date they were removed from the waiting list and the reason for this recorded.
In addition to the duration of the above processes, the following information was also recorded: referral source (same health network or another network); age on admission to acute hospital (years); gender; level of SCD (tetraplegia or paraplegia); and aetiology of SCD (traumatic SCI or non-traumatic SCM).
On admission to the SRU, the presence of any pelvic region pressure ulcers was noted. This complication was selected because wounds in this region have the greatest negative impact, compared with other locations, on participation in rehabilitation by limiting sitting in a wheelchair and bed-based tasks. At SRU admission and discharge, the American Spinal Injury Association Impairment Scale (AIS) grade of injury19 and the Functional Independence Measure (FIM) were recorded.20
Data collection and storage
The data were recorded in a password-protected database prospectively by the advanced trainee in rehabilitation medicine or the unit head and were reviewed by the unit head weekly to confirm their accuracy.
Statistical analysis
Continuous variables were described using the median and interquartile range (IQR). Comparisons were made using the Kruskal–Wallis rank test. Although multiple analyses were planned, as this was a hypothesis generating study no correction was made for these. Analysis was performed to test for the influence of clinical (AIS grade and level), demographic (gender or age) and referral source on the key process in the patient journey from acute hospital to SRU.
On the basis of previous research9, 17 it was decided to use the time waiting for a SRU bed after being deemed ready for transfer from acute hospital and the time from acute hospital admission until referral to the SRU as dependent variables for regression analysis. Stepwise multiple linear regression (backwards inclusion) was used to determine factors associated with the following four dependent variables: (1) the log-transformed time between acute hospital admission and referral to the SRU, (2) the log-transformed time between deemed ready for transfer to the SRU and admission, (3) the log-transformed rehabilitation LOS and (4) physical disability at discharge from SRU measured using the motor subscale of the FIM. Log-transformation was used to facilitate parametric analysis. As some of the wait periods in acute hospital were zero days, when the log-transformation was made for all of these one was added to the raw score to avoid a result of infinity. Patients’ age, gender, level, aetiology (SCI or SCM) and AIS on admission (dichotomised to AIS A, B or C versus D) were considered as covariates for all models. The FIM motor subscale on admission to SRU (as an indicator of disability and burden of care at transfer from acute hospital), the presence of a pelvic region pressure ulcer on SRU admission and the acute network where the patient was treated (same health network or another network) were additionally included as covariates in the second model. The log-transformed time between deemed ready for SRU and subsequent admission was included as a covariate in the third and fourth models. Admission FIM motor subscale was also included as a covariate in the fourth model.
All applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research. The project was approved by the Alfred Health Human Research Ethics Committee. P-values of <0.05 were deemed statistically significant. Stata version 12 (StataCorp, College Station, TX, USA) was used for statistical analysis.
Results
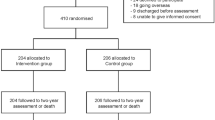
There were 378 patients referred to the SRU during the study period; however, 31 were excluded because they had a prior SCD, leaving 347 patients ranging in age from 17 to 93 years included in the analysis. We analysed the age of patients on admission, duration of the four key processes from acute hospital admission until transfer into SRU and the total acute hospital LOS by the following: aetiology of SCD, level of SCD, AIS on admission, gender and the acute hospital Network before rehabilitation admission Table 1.
The proportion of patients achieving the key processes within specified time frames is shown in Table 2. Half the patients spent 28.6% of their acute hospital admission waiting for a rehabilitation bed and a quarter of patients spent 54.1% of their acute admission waiting for a SRU bed. Overall, SCD patients spent 34.2% (4951/14 478 days; IQR 8.3–51.4%) of their acute hospital LOS waiting for a SRU bed to become available.
Of the 347 patients referred and accepted for admission into the SRU, most (n=283, 81.6%) were subsequently admitted. However, 31 patients (8.9%) were admitted to a non-specialist rehabilitation unit because of the long delay waiting for a bed into the SRU, 10 patients (2.9%) changed their mind after being accepted and decided that they did not want to come to the SRU, 6 patients were transferred to palliative care, 6 patients (1.7%) died and 11 (3.2%) were removed from the waiting list for other reasons.
The results of the multiple linear regressions to determine the influence of variables on (1) the delay between acute hospital admission and referral to the SRU, (2) delay between deemed ready for rehabilitation and transfer into the SRU, (3) LOS in the SRU and (4) motor subscale of the FIM at discharge from SRU are shown in Table 3.
Patients with a more complete grade of injury tended to have a longer duration between acute hospital admission and referral to SRU. A longer delay from when deemed ready for transfer to SRU and subsequent admission into SRU was found for patients who were more physically disabled (lower motor FIM), had a pelvic region pressure ulcer on admission to the SRU, were female or were referred from another network to the SRU. The LOS in the SRU tended to be longer for patients who were more disabled on admission and was not influenced by the duration of the wait from being deemed ready for SRU until transfer. Patients who were less disabled at discharge from SRU tended to be less disabled on admission, have a longer LOS in rehabilitation, wait shorter from being deemed ready for transfer to SRU after being deemed ready, have a traumatic SCI and were younger.
Discussion
There was typically a short delay between referral and assessment by the SRU, and most SCD patients were ready for transfer to rehabilitation on the day of assessment. The longest delays were for the period between the acute hospital admission/onset of SCD and the referral for assessment by the SRU and the wait for transfer to SRU after being deemed ready for admission.
These findings highlight the important opportunities for improving the acute hospital processes for patients with SCD in our region. There is a need to educate acute hospital staff about the importance of commencing the discharge-planning process for patients with SCD much sooner. Earlier referral to a SRU has the potential to reduce unnecessary time in acute hospital and prevent complications related to SCD. No explanation is available as to why the patients with complete SCD would tend to wait longer for referral, and it is important to note that this covariate only explained a small amount of the variance in the regression analysis.
A major effort is needed to reduce the unnecessary time that patients with SCD spend in acute hospital waiting for a bed in a SRU, particularly for patients from other health networks to the one associated with the SRU. This would also probably help to reduce the not insignificant proportion of patients accepted to the SRU but subsequently admitted to non-specialist general rehabilitation units because of the long delay they spent waiting for a SRU bed. Patients in our study who waited longer for a SRU bed after being deemed ready tended to have a lower motor FIM score on admission, be more likely to have a pressure ulcer and were female. No explanation is available as to why female patients waited longer for admission into the SRU. It is not possible to determine whether the increased pressure ulcers and disability in patients who waited longer for a SRU bed was a result of the delay or the cause. Patients experiencing a longer delay for a SRU bed tended to have greater disability at rehabilitation discharge, after adjusting for the disability on admission. The LOS in SRU was prolonged for patients who were more disabled on admission and those who waited longer for a SRU bed after being deemed ready for transfer, possibly because of greater deconditioning or increased complications, again emphasising the importance of developing strategies to reduce this wait.
A study of general rehabilitation patients admitted into two units in a different health network in Melbourne recently reported that the proportion of acute hospital LOS spent waiting for a rehabilitation bed was 12%.9 The waiting time for the key processes for the SCD patients in this study was much longer compared with the general rehabilitation patients, especially for the delay between acute hospital admission and referral and being deemed ready for rehabilitation and transfer.
There are a number of studies in the literature that are relevant for comparison with our findings. There are a few reports in the literature of delays for patients with SCD accessing SRU. Different authors use different cutoffs in duration for defining delays in processes, whereas in the present study the durations are reported as medians, IQR and proportion of patients achieving process within certain time frames. In one study from the United Kingdom over a 5-year period, the average time from traumatic SCI to referral was 5.5 days and from referral to admission was 10.7 days.6 As was found here, others have also reported an association between the delay in admission to SRU and the occurrence of pressure ulcers,14 increased LOS in SRU6, 14, 21 and greater disability at discharge from SRU.15, 21
A strength of this study is that it uses validated measures of the key processes in the acute hospital to SRU journey to identify opportunities for improvement.9, 17 Although others have highlighted the delays that patients with SCD can face in accessing SRU,5, 6, 14, 15, 16 none have reported the duration of each sequential process.
The results of this study cannot be generalised to other SRUs because of the variability in systems and organisation of care for patients with SCD.22 It is important to emphasise, however, that unless processes are measured, they cannot be improved, and that there appears to be support internationally among those working in SRUs to record these processes for benchmarking and quality improvement processes.16
Limitations of this study include that data were only collected from one SRU and there is inevitably referral bias associated with any centre. Our SRU has a bias towards patients with SCM. It was not possible to explore the reasons for delay in admission to SRU or referral.
In conclusion, the implications of this study are that future study of process barriers for admission into SRUs should include the reasons for delay and involve a number of different sites. Health-care managers and clinicians should allocate resources to process improvement projects that optimise the acute hospital LOS for patients with SCD in order to reduce complications, preventable disability and improve the efficiency of the hospital system by facilitating earlier referral and transfer to specialised SRU.
Data Archiving
There were no data to deposit.
References
Eitel DR, Rudkin SE, Malvehy MA, Killeen JP, Pines JM . Improving service quality by understanding emergency department flow: a White Paper and Position Statement prepared for the American Academy of Emergency Medicine. J Emerg Med 2010; 38: 70–79.
Weaver FM, Guihan M, Hynes DM, Byck G, Conrad KJ, Demakis JG . Prevalence of subacute patients in acute care: results of a study of VA hospitals. J Med Syst 1998; 22: 161–172.
Flintoft VF, Williams Jl, Williams RC, Basinski AS, Blackstien-Hirsch P, Naylor CD . The need for acute, subacute and nonacute care at 105 general hospital sites in Ontario. Joint Policy and Planning Committee Non-Acute Hospitalization Project Working Group. CMAJ 1998; 158: 1289–1296.
United Nations. Report of the Second World Assembly on Ageing;, 8–12 April 2002; Madrid, Spain. United Nations: New York, NY, USA.
Pagliacci MC, Celani MG, Spizzichino L, Zampolini M, Aito S, Citterio A et al. Spinal cord lesion management in Italy: a 2-year survey. Spinal Cord 2003; 41: 620–628.
Amin A, Bernard J, Najarajah R, Davies N, Gow F, Tucker S . Spinal injuries admitted to a specialist centre over a 5-year period: a study to evaluate delayed admission. Spinal Cord 2005; 43: 434–437.
Bradley LJ, Kirker SG, Corteen E, Seeley HM, Pickard JD, Hutchinson PJ . Inappropriate acute neurosurgical bed occupancy and short falls in rehabilitation: implications for the National Service Framework. Br J Neurosurg 2006; 20: 36–39.
New PW, Cameron PA, Olver JH, Stoelwinder JU . Key stakeholders’ perception of barriers to admission and discharge from inpatient subacute care in Australia. Med J Aust 2011; 195: 538–541.
New PW, Andrianopoulos N, Cameron PA, Olver JH, Stoelwinder JU . Reducing the length of stay for acute hospital patients needing admission into inpatient rehabilitation: a multicentre study of process barriers. Intern Med J 2013; 43: 1005–1011.
New PW, Jolley DJ, Cameron PA, Olver JH, Stoelwinder JU . A prospective multicentre study of barriers to discharge from inpatient rehabilitation. Med J Aust 2013; 198: 104–108.
Andrews LB, Stocking C, Krizek L, Gottlieb L, Krizek C, Vargish T et al. An alternative strategy for studying adverse events in medical care. Lancet 1997; 349: 309–313.
Wolfe DL, Hsieh JTC, Curt A, Teasell RW, the SCIRE Research Team. Neurological and functional outcomes spinal cord injury. Top Spinal Cord Inj Rehabil 2007; 13: 11–31.
New PW, Simmonds F, Stevermuer T . Comparison of patients managed in specialised spinal rehabilitation units with those managed in non-specialised rehabilitation units. Spinal Cord 2011; 49: 909–916.
Aung TS, El Masry WS . Audit of a British centre for spinal injury. Spinal Cord 1997; 35: 147–150.
Scivoletto G, Morganti B, Molinari M . Early versus delayed inpatient spinal cord injury rehabilitation: an Italian study. Arch Phys Med Rehabil 2005; 86: 512–516.
New PW, Scivoletto G, Smith É, Townson A, Gupta A, Reeves RK et al. International survey of perceived barriers to admission and discharge from spinal cord injury rehabilitation units. Spinal Cord 2013; 51: 893–897.
New PW, Cameron PA, Olver JH, Stoelwinder JU . Defining barriers to discharge from inpatient rehabilitation, classifying their causes, and proposed performance indicators for rehabilitation patient flow. Arch Phys Med Rehabil 2013; 94: 201–208.
Poulos CJ, Eagar K, Poulos RG . Managing the interface between acute care and rehabilitation—can utilisation review assist? Aust Health Rev 2007; 31 (suppl 1): S129–S140.
Marino RJ, Barros T, Biering-Sørensen F, Burns SP, Donovan WH, Graves DE et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Med 2003; 26 (Suppl 1): S50–S56.
Guide for the Uniform Data Set for Medical Rehabilitation (including the FIM instrument), version 5.1. State University of New York at Buffalo: Buffalo, NY, USA, 1997.
Sumida M, Fujimoto M, Tokuhiro A, Tominaga T, Magara A, Uchida R . Early rehabilitation effects for traumatic spinal cord injury. Arch Phys Med Rehabil 2001; 82: 391–395.
New PW, Townson A, Scivoletto G, Post MWM, Eriks-Hoogland I, Gupta A et al. International comparison of the organisation of rehabilitation services and systems of care for patients with spinal cord injury. Spinal Cord 2013; 51: 33–39.
Acknowledgements
I thank Drs Irina Astrakhantseva, Puey Ling Chia, Seema Chopra, Harry Eeman, Kapil Gupta, Cristina Manu, Caroline McFarlane, Olivia Ong, Parinaz Sharifi, James Ting and especially Richard Bignell for their assistance with data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The author declares no conflict of interest.
Additional information
An interim analysis of the data used in this manuscript was presented at the combined 50th International Spinal Cord Society and American Spinal Injury Association annual scientific meeting, 3-8th June 2011, Washington DC, USA.
Rights and permissions
About this article
Cite this article
New, P. Reducing process barriers in acute hospital for spinal cord damage patients needing spinal rehabilitation unit admission. Spinal Cord 52, 472–476 (2014). https://doi.org/10.1038/sc.2014.59
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2014.59