Abstract
Study design:
Cross-sectional study.
Objectives:
The present study aims to analyze and correlate the interlimb reflexes (ILRs), through a standard methodology, in tetraplegic and healthy subjects. The study of the connectivity between the injured spinal cord and the ILR transmission empowers new rehabilitation pathways for tetraplegic patients.
Setting:
University Hospital—UNICAMP, Campinas, Brazil.
Methods:
A total of 15 chronic tetraplegic patients and 10 healthy subjects were analyzed with the same methodology. Two tests were performed: (i) In test 1, the stimulus was applied to the right-arm radial nerve and the electromyography (EMG) signal collected in contralateral left tibial muscle. (ii) In test 2, the stimulus was applied to the left-leg fibular nerve and EMG collected in contralateral limb biceps, exploring the opposite direction of the pathway. In both tests, the subjects were stimulated with intensities from 5 to 30 mA (5 mA step) and 40 × 500 μs current modulated pulses. Reflexes were detected from the averaging of the 40 EMG sweeps.
Results:
Each group was analyzed with regard to the reflexes’ incidence, amplitude and latency. ILRs were found with similar prominence in both groups. A correlation between the ILR amplitude and the subject injury level was verified. Significant differences were found in the correlation of ILR latency with stimulation charge between healthy and tetraplegic subjects.
Conclusion:
The ILR transmission parameters of healthy and tetraplegic subjects were studied. The results obtained strongly suggest a different ILR transmission between healthy and tetraplegic subjects, reinforcing the hypothesis of nerve regeneration after injury.
Similar content being viewed by others
Introduction
Neuroplasticity is the central nervous system’s ability to adapt when exposed to changes. It presents itself in varied situations, from memory processes to recovery from injuries.1,2 Dynamic changes associated with recovery may be observed in a diversity of complementary diagnostic tests. Imaging studies, such as computerized tomography and nuclear magnetic resonance imaging, do not correlate directly to the clinical status of subjects and provide less functional information regarding the, sometimes subtle, recovery of the patients. On the other hand, studies with electromyography (EMG), evoked potentials and interlimb reflexes (ILR) are better suited to assess the physiology of specific neural pathway.3
Studies on ILR have gained importance over the past years. ILR pathway represents an interconnection between upper and lower limbs. Thus, stimulus applied on cutaneous nerves of the upper limb can evoke motor response on contralateral lower limb, and vice versa. Although there are still few studies on the matter, some authors have found ILR in healthy subjects and correlated it with bipedal gait and spatial orientation.4, 5, 6, 7 Other studies claim that the ILRs found in spinal cord injury (SCI) patients are due exclusively to cellular modifications on the injury level and a new proprio-spinal pathway,8,9 which may suggest a regeneration process. Recent studies have identified the existence, but have not yet established objective measures of the ILRs.
In the present study, two groups of SCI patients and one healthy control group are analyzed for a better understanding of ILR, in an attempt to establish objective parameters for future use in the evaluation of inter- and intrasubject clinical evolution. Objective analysis of the proprio-spinal pathway responsible for the ILR may present the possibility of interlimb recovery therapy, in which stimulation of lower limbs could help improve upper limbs functionality and vice versa, leading to new therapeutic options for SCI patients. In tetraplegic patients, increased functionality of upper limbs has a fundamental role in a better quality of life, increasing also the subject’s independence regarding routine activities and self-esteem.
Materials and methods
Subjects
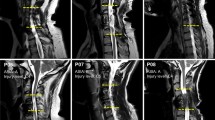
In this study a total of 25 subjects were analyzed and divided into three groups. Group 1 was composed of six male tetraplegic patients with sensory level10 between C1 and C4 (Asia Impairment Scale (AIS)-A10 n=5, AIS-B n=1), with a mean (s.d.) age at lesion of 25.16 (4.16) years, ranging from 20 to 31 years, and chronic traumatic lesion for a mean age of 12.00 (4.29) years, ranging from 7 to 17 years. Group 2 was composed of nine male tetraplegic patients with a sensory level between C5 and C8 (AIS-A n=7, AIS-B n=1 and AIS-C n=1), with a mean age at lesion of 26.44 (6.07) years, ranging from 19 to 34 years, and chronic traumatic lesion for a mean of 10.55 (2.92) years, ranging from 6 to 14 years. Finally, a control group was composed of 10 healthy subjects (8 males and 2 females), with a mean age of 22.00 (1.58) years, ranging from 22 to 26 years, without clinical history on neurologic disorders. The exclusion criterion for groups 1 and 2 was a time since traumatic injury <1.5 years, for properly central nervous system (CNS) adaptation.2 For the control group, the exclusion criterion was the existence of a previous diagnosis of neurological or degenerative disease. All experiments were approved by the Research Ethics Committee of the University Hospital of State University of Campinas.
Procedure
To explore both directions of the interlimb contralateral pathway, two tests were performed:
-
In test 1, the stimulus was applied at the radial nerve of the right arm surface and the EMG signal collected on the contralateral left leg anterior tibial muscle surface.
-
In test 2, the stimulus was applied at the fibular nerve surface on the left leg fibula head and EMG signal was collected on the surface of contralateral limb biceps brachii, exploring the opposite direction of the pathway.
In both the tests, the subjects were relaxed and seated while they were stimulated with intensities from 5 to 30 mA (5 mA step), with 40 sweeps of 500 μs current modulated single pulses, for each current increment. To properly cancel noise and mechanical artifacts, the pulses were randomly distributed into frequencies from 1.8 to 2.2 Hz. The entire procedure was repeated three times per patient, each repetition using a different single-pulse stimulation waveform,11 called mode. A standard square wave was applied in mode 1, a triangular wave in mode 2 and a quadratic wave in mode 3. In all three modes, monophasic single pulses were used with the same intensities and the same duration (500 μs). The current charge difference from each waveform was taken into account in the data analysis. The stimulation charge was computed accordingly to the stimulation intensity and waveform, with the following formula:

where I represents the current intensity, and t1 to t2 is the stimulus time, which in this case is a constant (500 μs).
The application of this neuromodulation methodology enables the exploration of new descriptive parameters for the evaluation of the interlimb propriospinal pathway.
EMG signal was acquired with a 2000 Hz sampling frequency, amplified with a gain of 1000, 12 bits of resolution and bandpass filtered from 25 to 550 Hz. A combined wireless, miniaturized and synchronized unit specifically developed with PLUX12 was used for EMG acquisition and nerve-stimulation hardware.13 Self-adhesive pre-gelled Ag/AgCl electrodes were used for EMG acquisition and peripheral nerve stimulation. The acquisition electrodes were placed according to SENIAM standards14 and the ground electrode was placed at the radius’ styloid apophysis.
Figure 1 illustrates the procedure for EMG acquisition and electrical stimulation in both tests. A schematic representation of the interlimb contralateral pathway is also included in this figure.
Illustration of test 1 and test 2 stimulation electrodes positioning and respective evaluated muscles through EMG acquisition. Also present in this figure is a schematic representation of the interlimb contralateral pathway. In the figure, the black line represents the averaging wave of reflexes from 40 sweeps on biceps brachii for test 2 and tibialis anterior for test 1.
Data analysis
The first step of data analysis was to automatically detect the incidence of ILR in all subjects. After automatic detection, all the ILR sweeps were still visually validated individually by four MD specialists.
For the subjects with ILR incidence, in the EMG signal, the peak reflex amplitude values were automatically withdrawn. Only the first reflex after stimulus was considered to explore the shortest possible pathway for ILR.
The electromyographic signal was acquired and stored continuously. Each sweep was stored with a time window from −50 ms to 250 ms (considering 0 ms as the stimulus moment).
Reflexes were extracted from the averaging of the 40 EMG sweeps, acquired in each stimulation intensity (5–30 mA pulses with 5 mA step). Peak-to-peak amplitudes and latencies were computed from the resulting mean wave. For amplitude, the absolute difference between maximum and minimum values of the first reflex was considered. For latencies, the time distance between stimulus and reflex first peak point (maximum or minimum) was considered. The mean and s.d. value for amplitudes and latencies, in each intensity step, was computed for groups 1, 2 and control.
All the data analysis and results gathering was done using signal processing scripts developed in Python.
Results
Each group was analyzed with regard to the reflexes' incidence, amplitude and latency.
The intersubject incidence of ILR enables the analysis of the number of subjects that elicited significant reflexes in comparison with the total number, n, of the analyzed population. Table 1 provides the results for the intersubject incidence of reflexes for the three groups, different stimulation modes and tests. The incidence was ~50% for both tests and groups. Test 2 generally elicited more occurrence of reflexes.
Figures 2a and b present an example EMG signal, acquired in each intensity step (from 5 to 30 mA), for one healthy and one SCI subject, respectively. Figure 2b is representative of the findings in both SCI groups (G1/G2) and tests.
Results of ILR elicited with different stimulation intensities for test 1 in (a) healthy subjects (representative example from one subject of the control group); (b) SCI subjects (representative example from one subject of group 1). The black line represents the average of the 40 EMG responses to the stimulation. Background lines are the 40 responses overlapped and the black dot denotes the automatic peak and latency detection. The thick vertical black line denotes the stimulation instant, covering the stimulation artifact.
The stimulation instant is marked with a thick vertical line at 0 ms, partially covering the stimulation artifact. Comparing the results of both figures, we found a different behavior in the control group versus the SCI groups. Although the reflex latency for the healthy subjects remains almost unaltered with the increase of stimulation intensities in the SCI groups, the latency shows a notorious rise tendency pattern.
Figure 3 presents the mean values of the reflexes' peak-to-peak amplitudes from each group related to the stimulation intensities applied in all participants. This figure was compiled with results from test 1 and mode 1, but is consistent with both tests and stimulation modes. The reflexes' peak-to-peak amplitude remains almost constant with the different stimulation intensities for all three groups. However, there is a distinct difference among the groups regarding its base amplitude value.
As differences were found between groups regarding the reflexes' latency (as seen in Figures 2a and b), an analysis of this parameter was compiled in Figures 4a and b. These figures present the results of the mean reflexes' latency from each group related to the stimulation charge for tests 1 and 2, respectively.
The reflexes' latency shows different behaviors regarding each group and, unlike the reflex amplitude, is correlated with the stimulation charge—showing different increase tendencies for each group. Table 2 compiles the linear tendency equations and R2 for each group between stimulation charge and latency response.
In some patients (n=2 from group 1), during the acquisition procedure, a prominent twitch-like movement of the upper contralateral limb, following the stimulation frequency, was also verified.
Discussion
Incidence
The intersubject incidence of ILR, either in healthy subjects or in patients with SCI, is involved in scientific controversy.4, 5, 6, 7 This study evaluates the ILR incidence in healthy subjects and SCI subjects through the same methodology, for a proper discussion. Although, for this analysis, the sample is not sufficiently significant, in this study the intersubject incidence was revealed to be uncorrelated with the clinical condition of the patient or stimulation charge. These results support the latest works exploring ILR on healthy subjects4, 5, 6, 7 and SCI patients.2 It was verified that the intersubject incidence is always higher for test 2, with the stimulation on fibular nerve and acquisition at biceps brachii, than for test 1. These results suggest a higher excitability of this pathway than in the opposite direction.
Amplitude
Previous works with healthy subjects analyzed the ILR amplitude of each subject, normalizing the amplitude with their maximum voluntary contraction.4, 5, 6, 7 Owing to the clinical condition of the SCI patients, a different normalization process needs to be implemented. For reliable comparison between different groups, the ILR amplitude was analyzed by referring to the measured absolute value (in μV).
Although the amplitude of the ILR measured from the EMG signal can be highly correlated with external factors, some conclusions are prominent. A correlation between the ILR amplitude and the clinical condition of the patient is verified. In this case, healthy subjects produce generally ILR with higher amplitudes than the SCI subjects. This fact was expected as the SCI patients can have a compromised nerve conductivity. Within the ILR subjects, the highest injury group, group 1, shows amplitudes above the lowest injury level group, group 2. Possibly this is explained by the higher proximity between the interlimb connection level and the lesion level for the lowest injury group (group 2 C5–C8).
It was also found that the amplitude of the responses analyzed does not expose an obvious correlation with the amplitude/charge of stimulation.
Latency
Regarding the ILR latency on healthy subjects, it is verified that there is a small correlation between stimulation intensity and charge with the reflex latency. In test 1 the latency was stable, with a very low linear uprising tendency (between 40 and 60 ms). In test 2, for the same group, the latency was ~40 ms, independently of the stimulation intensity or charge. These results are in accordance with the standards for the healthy nerve conduction speed.15 A strong correlation of the ILR latency with the electrical pulse charge is verified in SCI patients. As it can be seen in a more prominent way in test 2 (Figure 4b), the latency evolves with stimulation charge, independently of the injury level. The linear equations and R2 present in Table 2 show a stronger correlation for groups 1 and 2 than for the control group. In test 1, group 1, the rising tendency is influenced by one SCI subject outlier (AIS-A) that revealed a different behavior with no latency increase response (Figure 5). This pattern was previously reported by McNulty and Burke,16 where the only patient analyzed showed a similar response. However, even with this outlier subject, the rising pattern is still linear, with a R2 value of 0.96.
Results of EMG response with different stimulation intensities of test 2 from the unique patient that exposed a different rise pattern of ILR latency related to the stimulation charge. The black line represents the averaging of the 40 EMG responses to the stimulation. Background lines are the 40 responses overlapped and the black dot denotes the automatic peak and latency detection. The thick vertical black line denotes the stimulation instant, partially covering the stimulation artifact.
Analyzing ILR latency referent to the first stimulation charge (base latency), some differences emerge between tests 1 and 2. Whereas in test 1 the base latency is identical in both SCI (G1/G2) and control groups (average=44.318 ms; std=3.466 ms; n=10), in test 2 the SCI subject’s latency starts with an offset. The lowest latency for SCI subjects in test 2 is ~90 ms (average=96.389 ms; std=2132 ms; n=9), whereas for the control group it is 40 ms (average=43 ms; std=1414 ms; n=3).
All these facts strongly suggest different pathways between SCI patients and healthy subjects.
Supporting theories
ILRs have been previously explored in healthy subjects and are hypothesized to facilitate a reciprocal gait coordination mechanism for bipedal locomotion that is mediated by long propriospinal fibers.4, 5, 6, 7 However, Calancie et al.2 state that the ILRs arise through an exclusive SCI patients’ pathway, emerging from a regenerative sprouting process of ascending afferent fibers, which do not reconnect again into the original target populations. It is assumed that this process is triggered after denervation of the spinal tract caused by the injury and that this new pathway, generated only 6 months after injury, is strengthened over time. Calancie et al.2 have not verified the existence of ILR in healthy subjects and state some inconsistency of the ILR mechanism studied in healthy subjects by Zehr et al.17 in comparison with the reported mechanism in SCI patients.
In this study, the same methodology was applied for the first time to both healthy and SCI subjects. The results are consistent with the previous studies that reported the presence of ILR in healthy subjects. The comparison conducted in this study also supports the idea of a different ILR transmission mechanism between healthy and SCI subjects, strongly reinforcing the hypothesis of nerve regeneration after spinal cord acute injury. This is concluded mainly owing to the differences in latency response to stimulation charge (Figures 2a and b, and Figures 4a and b).
This study evaluated the ILR transmission mechanism in SCI patients and compared them with a healthy control group. It was possible to establish descriptive parameters for the ILR cortico-spinal pathway characterization. With these results the ILR pathway can now be explored from the functional interlimb rehabilitation and training perspective for tetraplegic patients.
Data Archiving
There were no data to deposit.
References
Calancie B, Lutton S, Broton JG . Central nervous system plasticity after spinal cord injury in man: interlimb reflexes and the influence of cutaneous stimulation. Electroencephalogr Clin Neurophysiol 1996; 101: 304–315.
Calancie B, Molano MR, Broton JG . Interlimb reflexes and synaptic plasticity become evident months after human spinal cord injury. Brain 2002; 125: 1150–1161.
Alonso K, Azevedo E, Beinotti F, Maria R, Cliquet A . Electromyographic assessment of the tetraplegic upper limb during functional movement. J Neurologic Sci 2013; 333: e564.
Haridas C, Zehr EP, Misiaszek JE . Context-dependent modulation of interlimb cutaneous reflexes in arm muscles as a function of stability threat during walking. J Neurophysiol 2006; 96: 3096–3103.
Sakamoto M, Endoh T, Nakajima T, Tazoe T, Shiozawa S, Komiyama T . Modulations of interlimb and intralimb cutaneous reflexes during simultaneous arm and leg cycling in humans. Clin Neurophysiol 2006; 117: 1301–1311.
Haridas C, Zehr EP . Coordinated interlimb compensatory responses to electrical stimulation of cutaneous nerves in the hand and foot during walking. J Neurophysiol 2003; 90: 2850–2861.
Lamont EV, Zehr EP . Earth-referenced handrail contact facilitates interlimb cutaneous reflexes during locomotion. J Neurophysiol 2007; 98: 433–442.
Calancie B . Interlimb reflexes following cervical spinal cord injury in man. Exp Brain Res 1991; 85: 458–469.
Calancie B, Alexeeva N, Broton JG, Molano MR . Interlimb reflex activity after spinal cord injury in man: strengthening response patterns are consistent with ongoing synaptic plasticity. Clin Neurophysiol 2005; 116: 75–86.
Kirshblum SC, Waring W, Biering-Sorensen F, Burns SP, Johansen M, Schmidt-Read M . Reference for the 2011 revision of the International Standards for Neurological Classification of Spinal Cord Injury. J Spinal Cord Med 2011; 34: 547–554.
Rosellini WM, Yoo PB, Engineer N, Armstrong S, Weiner RL, Burress C et al. Voltage Controlled Capacitive Discharge Method for Electrical Activation of Peripheral Nerves. Neuromodulation 2011; 14: 493–500.
PLUX—Wireless Biosignals, S.A,. 2013. http://www.plux.info (retrieved on 28 November 2013).
Araújo T, Nunes N, Gamboa H . Miniaturized wireless controlled electrostimulator. In: Proceedings of Biodevices—International Conference on Biomedical Electronics and Devices (BIOSTEC 2012); Vilamoura, Portugal, 2012.
Hermens HJ, Freriks B, Merletti R, Hägg G, Stegeman D, Blok J . SENIAM 8: European Recommendations for Surface Electromyography. Roessingh Research and Development: Enschede, The Netherlands, 1999.
Parry GJ, Steinberg JS . Guillain-barré Syndrome: From Diagnosis to Recovery, 1st edn Demos Medical Publishing: St Paul, MN, USA, 2007.
McNulty PA, Burke D . Self-sustained motor activity triggered byInterlimb reflexes in chronic spinal cord injury, evidence of functional ascending propriospinal pathways. PLoS ONE 2013; 8: e72725.
Zehr PE, Collins DF, Chua R . Human interlimb reflexes evoked by electrical stimulation of cutaneous nerves innervating the hand and foot. Exp Brain Res 2001; 140: 495–504.
Acknowledgements
We thank the Research Foundation of São Paulo-FAPESP (Grant nos. 2003/05856-9 and 1996/12198-2), national research funding agencies CNPq and CAPES—Brazil and Foundation for Science and Technology from Portugal (Grant number SFRH/BDE/51380/2011) and Faculty of Science and Technology—New University of Lisbon (Grant number PEst-OE/FIS/UI0068/2014—CEFITEC) for the financial support to this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 3.0 Unported License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/3.0/
About this article
Cite this article
Araújo, T., Brandão, A., Didier, T. et al. Analysis of descriptive electrophysiological parameters in contralateral interlimb reflexes on tetraplegic patients. Spinal Cord 52, 894–900 (2014). https://doi.org/10.1038/sc.2014.169
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2014.169